Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Child Health
versão On-line ISSN 1999-7671
versão impressa ISSN 1994-3032
S. Afr. j. child health vol.14 no.1 Pretoria Abr. 2020
http://dx.doi.org/10.7196.SAJCH.2020.v14.i1.1620
RESEARCH
The quality of life, health needs and knowledge of children living with congenital heart disease in KwaZulu-Natal Province, South Africa
P PillayI; N PefileII; S CobbingIII; T GurayahIV
IBSc (Physio), MSc (Physio); Inkosi Albert Luthuli Hospital, Mayville, Durban, KwaZulu-Natal, South Africa
IIBSc, PGD (Public Health), MMedSc (Rehabilitation) Inkosi Albert Luthuli Hospital, Mayville, Durban, KwaZulu-Natal, South Africa
IIIBSc (Physio), MSc (Health Sciences), PhD; Inkosi Albert Luthuli Hospital, Mayville, Durban, KwaZulu-Natal, South Africa
IVBOcc Th, M OT Inkosi Albert Luthuli Hospital, Mayville, Durban, KwaZulu-Natal, South Africa
ABSTRACT
BACKGROUND. An understanding of the lived experiences of children with congenital heart disease (CHD) will aid in improving the way that both parents and medical practitioners manage them holistically.
OBJECTIVE. To explore the perceptions of children living with CHD in KwaZulu-Natal (KZN) province of South Africa (SA), on their quality of life (QoL), health needs and knowledge of their medical conditions.
METHODS. A sequential explanatory mixed-methods design was employed. The study population comprised children aged between 8 and 12 years with CHD who attended cardiology clinics at the study hospital. Convenience sampling was used. Forty-three children participated in Phase 1 and 7 participants were interviewed in Phase 2. The study setting was a tertiary-level public hospital in eThekwini District, KZN, SA. The research procedure comprised a file audit of confirmed CHD in prospective participants. Caregivers completed a consent form while the children assented and completed the PedsQL 4.0 questionnaire. Interviews were conducted in Phase 2.
RESULTS. Phase 1: Both genders had higher psychosocial functioning (PSF), compared with physical functioning (PF). Children with mixed cardiac defects had lower health-related quality of life (HRQoL), compared with cyanotic or acyanotic individuals. The effect of the number of cardiac procedures on the PF domain showed a significant effect (p=0.042). Phase 2: This group had poor knowledge of their medical condition and had specific health needs.
CONCLUSION. The findings highlight the need for improved knowledge/information on physical capabilities, medical information and support from family, caregivers and medical staff.
Individuals with congenital heart disease (CHD) need lifelong healthcare.[1] CHD birth prevalence has reached a stable estimate of 9 per 1 000 live births.[2] An estimated 11 000 children are born annually with CHD in South Africa (SA) and it is the 9th most prevalent recorded cause of death in children >5 years.[3] Patients with CHD should receive continuous evaluation to determine their appropriate levels of physical activity, educational and emotional support and to improve their health-related quality of life (HRQoL).[4] A significant provision of the SA Children's Act No. 38 of 2005 (2010) is that the age of consent for medical and surgical treatment is set at 12 years, provided that children of this age have the maturity to understand the benefits, risks and other implications of treatment.[5] Failure of a healthcare worker to understand how to communicate knowledge about CHD to children may have a detrimental effect on their overall health and QoL.[6]
Despite progress in the development and utilisation of paediatric HRQoL measures,[7] there is limited research in SA on the HRQoL of children within this age group with CHD. The aim of the present study was to explore the perceptions of SA children living with CHD on their QoL, health needs and knowledge of their medical condition.
Methods
A sequential explanatory mixed-methods design was employed.[8] In Phase 1 of the study, descriptive data were collected on the domains of HRQoL, using the SA version of the PedsQL 4.0 Generic Core Scales Child report for children aged 8 - 12 years.[9] Semi-structured interviews were employed during the second phase of the study, which consisted of interviewing participants on their health needs and knowledge of CHD. This study was conducted at a tertiary-level public hospital in KwaZulu-Natal (KZN) Province, SA. Full ethical approval was obtained from the University of KwaZulu-Natal's Biomedical Research Ethics Committee (ref. no. BE090.16).
The study population consisted of children aged between 8 and 12 years old with CHD who attended cardiology clinics at the study facility, during a 12-week data collection period. The population for Phase 1 consisted of 43 children who assented, after their parents had consented to participate in the study. The sample size was relatively small owing to the recruitment of participants of a specific age group within a specific timeframe. Seven children from Phase 1 agreed to attend in-depth semi-structured interviews for Phase 2 of the study. They were selected based on their willingness to participate and their ability to understand the interview questions (in either English or isiZulu). The selection of participants for the second phase of the study had to be altered from selecting patients based on diagnosis and HRQoL scores, owing to children in this age group being unwilling to be interviewed. In the end, however, the 7 children who participated were willing and able to give feedback that could be used. Data from Phase 1 were analysed using SPSS version 23 (IBM Corp., USA). As the data were not normally distributed, non-parametric tests were employed. The statistician reviewed the data and ran specific data analyses. Normality tests noted the data to be non-normal distribution with the Shapiro-Wilks test; therefore, non-parametric tests were used to analyse data. The data for age and gender were analysed using descriptive frequency variables. Descriptive variables were used to analyse data on physical function (PF), social function (SF), emotional function (EF), school function (ScF), psychological function (PSF) and HRQoL of this sample group. Non-parametric tests on independent samples analysed included the Kruskal-Wallis test which was used to compare the domains of HRQoL with gender and the number of cardiac procedures on HRQoL. Interview data from Phase 2 were transcribed manually and thematic analysis employed to interpret the data.[10] This t method allowed the identifying, analysing and reporting of themes within data. This method emphasised organisation and description of collected data. An inductive approach allowed themes to be linked to the data.[10]
Results
Demographics
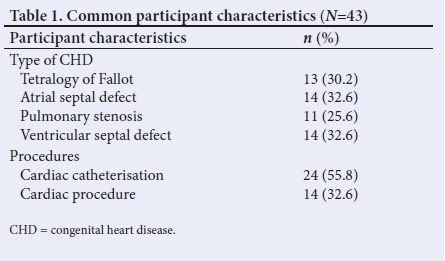
A total of 43 children participated in Phase 1; 23 (56.5%) were male and 20 (43.5%) female. The mean age was 10.07, median 10 and standard deviation 1.50. Seven children were interviewed in Phase 2: 4 male and 3 female, with tetralogy of Fallot (ToF) being their most common diagnosis (Tables 1 - 4).



The needs and knowledge of children living with CHD
The themes and quotes identified from interviews are shown in Table 5 to illustrate the qualitative results from Phase 2 of the study. Pseudonyms were used to maintain participant anonymity.
Our study found that both genders had higher PSF than PF. A significant effect (p=0.042) was noted when assessing the effect of the number of cardiac procedures on the PF domain. Phase 2 of the study found that these children demonstrated a relative lack of knowledge about their medical condition and had a need for information and support from family and healthcare professionals.
Discussion
Phase 1
The results of this study are similar to two African studies that identified VSD as the most common CHD.[11,12] and ToF as the most common cyanotic CHD in children.[12] ToF was the most common cyanotic heart defect presenting in early childhood, with surgical correction now routinely performed in the first year of life, giving patients an excellent long-term outlook with over 98% having a 20-year survival rate.[13] In our study, it emerged that boys had a higher overall HRQoL than girls, which contrasts with a study that showed that female gender was positively associated with higher life satisfaction and increased overall QoL.[14] Another study attributed poor PF to lack of knowledge, unrealistic expectations and misconceptions about the subjects' PF, which may be possible reasons for the low PF reported in our study.[15]
Children in the mixed cardiac defect group had lower HRQoL, although not statistically significant. An Iranian study[14] noted that QoL, health satisfaction, physical health and life satisfaction were independently associated with the presence of CHD, while the type of cardiac defect had no independent influence.
Cardiac surgery or hospitalisation, medication, severity of residual lesions and severity of physical limitations all had a negative impact on QoL.[14,16] A previous study noted that a greater number of cardiac interventions over the lifetime have been shown to have a significant negative impact on QoL,[17] which may explain the lower PF domain of HRQoL in children in our study.
Phase 2: Needs and knowledge of participants living with CHD
Participants' needs
Four out of 7 participants noted that they did not need help or assistance with any activities. A German study[18] of 10 - 30-year-olds with CHD noted that children express fewer information needs than adolescents and adults. A Belgium study[19] noted a desire for better quality of information about their medical condition and the process of transfer of care. Our study identified similar information to that in a study of 8 - 19-year-olds with CHD, who were unsure about their condition, and suggested reasons for this as either that they felt they had enough information, or they did not want to receive available information.[20] Likewise, the most important need of patients with CHD was to receive information about their illness, regarding the symptoms and course of the illness and to clarify any doubts they may have.[21]
A shift in roles between parents and themselves was acknowledged in children with CHD.[19] The client and family caregiver should be provided with both an explanation about the condition, progression, prevention, and management of symptoms, as well as the importance of regular follow-up, so as to encourage the client to learn health-related self-management behaviours.[21] In contrast to the present study, school-age children between 8 and 13 years old were noted to be increasingly knowledgeable about their chronic conditions and exhibited adequate skills to manage their activities. It is recommended that children develop self-care before adolescence, when there is a decline in self-management.[22]
Parental involvement in their child's care is fundamental, and at the same time the parents, as caregivers, might need support for facilitating their adolescents becoming independent and autonomous.[1] School performance of children with CHD is often impaired, and they usually fall behind in their school performance compared with their healthier schoolmates, owing to treatment processes involving hospital admissions and absence from school,[23] which may be the norm for our participants. Survivors of paediatric cardiac surgery required support services that included physical, occupational and speech therapy throughout their lives, which reinforced the need for a multidisciplinary team approach in managing patients with CHD.[24] Children experienced uncertainty about physical activity, and found it difficult to manage the physical aspects of their daily lives, if they were not given individualised information about how much physical activity they could participate in, without an adverse effect on their heart.[251 An SA study, involving under-2-year-olds with CHD and their parents, recommended developmental and psychosocial support services as a way to improve outcomes in children with CHD and their families.[11]
Knowledge of medical condition
Children are not always knowledgeable about their heart defect, with some having little understanding of their medical condition,!191 which was also the case with the participants in our study. A Canadian study[26] noted possible reasons for this as some patients not liking to think or talk about their heart, not understanding information from their doctors or information was difficult to understand because it was delivered rapidly.[11] Another possible reason for the poor knowledge of participants in our study was that patients' information needs were not met by the doctors. A possible reason for this is that doctors chose to address the parents, rather than the children themselves.[18] Poor knowledge and understanding of their heart condition in adolescents appeared to influence their HRQoL.[271 Ben was the only participant in our study who used the internet; however, it is difficult to validate the source and reliability of information from the internet because education thus obtained is considered as being of uncertain value.[251
Participants expressed a variety of emotions during their interviews that included fear, sadness, worry and anger. A large proportion of patients with CHD experienced psychological symptoms such as depression, anxiety, loneliness, behavioural problems and concentration difficulties.[28] Anxiety and depression could be attributed to recurrent hospitalisations, daily chronic medication and limitations on activities as a result of their illness.[23] Participants interviewed reported enjoying social sport activities with friends and siblings, which may be due to children having an innate need to be physically active. It has been suggested that children should be advised to participate in a large variety of activities to develop proper exercise habits, motor coordination, aerobic capacity, muscle strength, mental development and QoL.[29] Two participants, Bongiwe and Zandile, who noted that running was 'bad, were misinformed or incorrect, and this could be as a result of poor comprehension or parental overprotection or, as a UK study[30] suggested, children did not know the safe level of activity for their condition. Parents underestimating their child's physical ability could impose unnecessary restrictions on their child, thus depriving the child of the health and psychological benefits of exercise.[31] However, some children like Ben, who was diagnosed with Eisenmenger and pulmonary hypertension, need restrictions in activities and physical education at school. Playing inappropriate contact sports by choice may put children with chronic illness at significant risk of death, but some children were unaware of the danger.[30] Some participants in the present study understood their limitations as well as the repercussions on their health if they 'strained' themselves. While some participants in our study attempted to complete tasks independently, it is vital that patients are aware of their specific symptoms associated with the complications to which they are susceptible and know what actions to take if these symptoms present.[26] A good level of disease-specific knowledge has also been found to enhance treatment compliance.[18] Living with physical limitations may be frustrating, and sometimes the environment can result in restrictions such as those posed by overprotective parents and teachers.[1] In our study, participants who had the same diagnosis and similar management viewed parents' involvement in their life situations differently, e.g. some participants noted their parents' involvement in their healthcare decisions, which they felt were required. Parents nurturing their children, and a higher level of psychosocial maturity and autonomy, have been associated with better-perceived mental health status and QoL.[32]
In some cases, lack of knowledge can make it difficult for children with CHD to explain their cardiac condition to others,[20] which is why participants in our study may have chosen not to inform others, and hence the denial aspect with chronic illness. Providing teachers or employers with accurate information about the disease, including instructions on medication, exercise and work should be communicated timeously.[21] Interactions with peers revealed peer interest in their condition and, once peers had some information, they tended not to treat children with CHD any differently,[20] which was true for Luyanda, who informed her friends about her sternotomy scar, thus showing acceptance of her condition. Ben's understanding of his condition showed a level of maturity, describing how a friend's poor medical outlook would not affect him, despite the severity of his own condition. While maintaining a sense of personal privacy, the perspectives of patients and their parents regarding disease disclosure should be respected,[21] while it was also important that patients be provided with realistic evidence-based advice on their prognosis.
None of the participants in this study communicated directly or interacted with the doctor about their medical condition or treatment. Similarly, a German study[18] found that doctors communicated primarily with the parents and not directly with the child with CHD. Cardiologists interviewed in a previous study, stressed the importance of good communication when meeting families, but their strategies for facilitating such communication varied in terms of structure, relationship and degree of formality, and consisted of providing factual information to evaluate the emotional factors.[29] It has been proposed that education on CHD, QoL and self-care must begin during the school-age period if the child is to have the best opportunity to succeed in assuming responsibility for their own care as adults.[33]
Study limitations
The study was conducted in a specific age group in one hospital, which may have contributed to the relatively small sample size; this limits the generalisability of our findings and further resulted in limited statistical significance in the overall HRQoL measures of children with CHD. The results are still noteworthy, given the lack of evidence related to the HRQoL of SA children within this age group living with CHD.
Conclusion
The present study found that both genders had higher PSF and that the number of cardiac procedures had a significant influence (p=0.042) on the PF domain of HRQoL. These children demonstrated a relative lack of knowledge about their medical condition and its management. Participants demonstrated limited autonomy, but they had an overwhelming trust in their parents to take charge of medical decisions, which was necessary for the children. Participants' needs were focused on receiving appropriate information about their condition and good support structures. Recommending the use of HRQoL measures may be beneficial in the clinical management of children with CHD, as well as the ability of health professionals and parents to meet these individuals' needs more holistically.
Declaration. This manuscript was submitted in partial fulfilment of the requirements for the degree of Master of Physiotherapy.
Acknowledgements. None.
Author contributions. Equal contributions.
Funding. None.
Conflicts of interest. None
References
1. Bratt E, Lundell B, Nisell M. Adolescents with congenital heart disease and their parents needs before transfer to adult care. J Cardiovasc Nurs 2016; 31(5):1-6. https://doi.org/10.1097/JCN.0000000000000288 [ Links ]
2. Van der Linde D, Konings EEM, Slager AS, et al. Birth prevelance of congenital heart disease worldwide: A systematic review and meta-analysis. J Am Coll Card 2001;58:2241-2247. https://doi.org/10.1016/j.jacc.2011.08.025 [ Links ]
3. Nannan N, Dorrington R, Laubscher R, et al. Under-5 mortality statistics in South Africa: Shedding some light on the trends and causes 1997 - 2007. Cape Town: South African Medical Research Council, 2012. [ Links ]
4. Mellion K, Uzark K, Cassedy A, et al. Health-related quality of life outcomes in children and adolescents with congenital heart disease. J Pediatr 2014;164(4):781-788. https://doi.org/10.1016/j.jpeds.2013.11.066 [ Links ]
5. South African Children's Act 38 of 2005. 2010. www.justice.gov.za (accessed 25 November 2015). [ Links ]
6. Shearer K, Rempel G, Norris C M, Magill-Evans J. "It's no big deal": Adolescents with congenital heart disease. J Pediatr Nurs 2013;28(1):28-36. http://doi.org/10.1016/j.pedn.2012.03.031 [ Links ]
7. Varni J, Limbers CA, Burwinkle TM. How young can children reliably and validly self-report their health-related quality of life? An analysis of 8 591 children across age subgroups with the PedsQL 4.0 Generic Core Scales. Health Qual Life Outcomes 2007;1(5):1-13. http://doi.org/10.1186/1477-7525-5-1 [ Links ]
8. Creswell J. Research design:Qualitative, Quantitative, and Mixed Methods Approaches. 3rd ed. Thousand Oaks: SAGE Publications, 2009. [ Links ]
9. Varni J, Seid W, Kurtin P. PedsQL 4.0 : Reliability and Validity of the Pediatric Quality of Life Inventory Version 4.0 Generic Core Scales in Healthy and Patient Populations. Med Care 2001;39(8):800-812. https://doi.org/10.1097/00005650-200108000-00006 [ Links ]
10. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psych 2006;3(2):77-101. [ Links ]
11. Smith R. Neurodevelopment, quality of life and burden of care of young children who have undergone cardiac interventions in central South Africa: Three-month and six-month post cardiac intervention outcomes. PhD dissertation. Johannesburg: University of the Witwatersrand, 2017. [ Links ]
12. Sadoh WE, Uzodimma CC, Daniels Q. Congenital heart disease in Nigerian children: A multicenter echocardiographic study. World J Pediatr Congenit Heart Surg 2012;4(2):172-176. http://doi.org/10.1177/2150135112474026 [ Links ]
13. Kenny D, Stuart G. Long-term outcome of the child with congenital heart disease. Paediatr Child Health 2008;19(1):37-42. http://doi.org/10.1016/j.paed.2008.09.014 [ Links ]
14. Eslami B, Macassa G, Khankeh HR, Soares JJF. Quality of life and life satisfaction among adults with and without congenital heart disease in a developing country. Eur J Prevent Cardiol 2015;22(3):169-179. http://doi.org/10.1177/2047487313514017 [ Links ]
15. Fteropoulli T, Stygall J, Cullen S, Deanfield J, Newman SP. Quality of life of adult congenital heart disease patients: A systematic review of the literature. Cardiol Young 2013;1-13. http://doi.org/10.1017/S1047951112002351 [ Links ]
16. Teixeira FM, Coelho RM, Proenca C, et al. Quality of life experienced by adolescents and young adults with congenital heart disease. Pediatr Cardiol 2011;32(8):1132-1138. http://doi.org/10.1007/s00246-011-0039-0 [ Links ]
17. Knowles RL, Day T, Wade A, Bull C, Wren, C. Patient-reported quality of life outcomes for children with serious congenital heart defects. Arch Dis Child 2014;99:413-419. http://doi.org/10.1136/archdischild-2013-305130 [ Links ]
18. Lesch W, Specht K, Lux A, Frey M, Utens E, Bauer U. Disease-specific knowledge and information preferences of young patients with congenital heart disease. Cardiol Young 2014;24:321-330. http://doi.org/10.1017/S1047951113000413 [ Links ]
19. Moons P, Pinxten S, Dedroog D, et al. Expectations and experiences of adolescents with congenital heart disease on being transferred from pediatric cardiology to an adult congenital heart disease program. J Adolesc Health 2009;44(4):316-322. http://doi.org/10.1016/j.jadohealth.2008.11.007 [ Links ]
20. Birks Y, Sloper P, Lewin R, Parsons J. Exploring health-related experiences of children and young people with congenital heart disease. Health Expectations 2006;10:16-29. http://doi.org/10.1111/j.1369-7625.2006.00412.x [ Links ]
21. Chen C, Su W, Chiang Y, Shu Y, Moons P. Healthcare needs of adolescents with congenital heart disease transitioning into adulthood: A Delphi survey of patients, parents and healthcare providers. Eur J Cardiovasc Nurs 2016;16(2):1-11. http://doi.org/10.1177/1474515116643622 [ Links ]
22. Beacham B, Deatrick J. Health care autonomy in children with chronic conditions: Implications for self care and family management. Nurse Clin North Am 2013;48(2):305-317. http://doi.org/10.1016/j.cnur.2013.01.010.Health [ Links ]
23. Nousi D, Christou A. Factors affecting the quality of life in children with congenital heart disease. Health Sci J 2010;2(2):94-100. [ Links ]
24. O'Connor AM, Wray J, Tomlinson RS, et al. Impact of surgical complexity on health-related quality of life in congenital heart disease surgical survivors. J Am Heart Assoc 2016;(5):1-12. http://doi.org/10.1161/JAHA.114.001234 [ Links ]
25. Ronning H, Nielsen N, Swahn E, Stromberg A. Educational needs in adults with congenitally malformed hearts. Cardiol Young 2008;18(5):473-479. http://doi.org/10.1017/S1047951108002540 [ Links ]
26. Harrison JL, Silversides CK, Oechslin EN, Kovacs AH. Healthcare needs of adults with congenital heart disease study of the patient perspective. J Cardiovasc Nurs 2011;26(6):497-503. http://doi.org/10.1097/JCN.0b013e31820984c9 [ Links ]
27. Wang Q, Hay M, Clarke D, Menahem S. Associations between knowledge of disease, depression and anxiety, social support, sense of coherence and optimism with health-related quality of life in an ambulatory sample of adolescents with heart disease. Cardiol Young 2014;24:126-133. http://doi.org/10.1017/S1047951113000012 [ Links ]
28. Birkeland A. Psychosocial aspects of living with congenital heart disease. Child, family and professional perspectives. Published thesis, Department of Clinical Science, Faculty of Medicine, Umea University; 2012. [ Links ]
29. Vanhees L, Rauch B, Piepoli M, et al. Importance of characteristics and modalities of physical activity and exercise in the management of cardiovascular health in individuals with cardiovascular disease (Part III). Eur J Prevent Cardiol 2012;19(6):1333-1356. http://doi.org/10.1177/2047487312437063 [ Links ]
30. Kendall L, Parsons J, Sloper P, Lewin R. A simple screening method for determining knowledge of the appropriate levels of activity and risk behaviour in young people with congenital cardiac conditions. Cardiol Young 2007;17(2):151-157. http://doi.org/10.1017/S1047951107000285 [ Links ]
31. Uzark K, Jones K, Slusher J, Limbers CA, Burwinkle TM, Varni J. Quality of life in children with heart disease as perceived by children and parents. Pediatrics 2008;121(5):e1060-e1067. http://doi.org/10.1542/peds.2006-3778 [ Links ]
32. Mackie AS, Rempel GR, Islam S, et al. Psychosocial maturity, autonomy and transition readiness among young adults with congenital heart disease or a heart transplant. Congenit Heart Dis 2015;11:136-143. [ Links ]
33. Gurvitz M, Valente AM, Broberg C, et al. Prevalence and predictors of gaps in care among adult congenital heart disease patients. J Am Coll Cardiol 2013;61(21):2180-2184. http://doi.org/10.1016/j.jacc.2013.02.04 [ Links ]
 Correspondence:
Correspondence:
P Pillay
pillaypre@yahoo.com
Accepted 11 February 2019.














