Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Child Health
versión On-line ISSN 1999-7671
versión impresa ISSN 1994-3032
S. Afr. j. child health vol.13 no.4 Pretoria dic. 2019
http://dx.doi.org/10.7196/sajch.2019.v13i4.1587
CASE REPORT
Mesenteric cyst associated with tuberculosis in a child
H U IbrahimI; AMudiI; HKabirII; U A IbrahimII; U A SaboII
IMBBS, FWAC Paed;Department of Paediatrics, Aminu Kano Teaching Hospital and Bayern University, Kano, Nigeria
IIMBBS, FMC Paed;Department of Paediatrics, Aminu Kano Teaching Hospital and Bayern University, Kano, Nigeria
ABSTRACT
Mesenteric cyst is a rare occurrence in children and there are few reports of its association with abdominal tuberculosis (TB). We present the case of a 9-year-old boy with a 4-month history of fever, progressive abdominal pain and swelling, weight loss and no prior immunisation. There was a history of contact with a chronically coughing adult. He had massive ascites at presentation; the ascitic fluid was exudative but negative for TB. Radiological imaging showed left lobar consolidation on chest radiograph and a ring-enhancing hypodense cystic lesion on the jejunal mesentery on abdominal computed tomography scan. A clinical diagnosis of disseminated TB with mesenteric cyst was made. He was commenced on TB treatment with complete resolution of signs and symptoms by the eighth month of therapy. Mesenteric cysts resulting from TB may resolve over time with standard treatment for TB, as in the case of our patient, without the need for surgical intervention.
Mesenteric cyst is a rare cause of intra-abdominal pathology in children, and in a few instances may result as one of the manifestations of abdominal tuberculosis.[1,2] This is not surprising as the incidence of infection from Mycobacterium tuberculosis (TB) is still high, with several active infections reported annually.[3] We present the case of a paediatric patient with mesenteric cyst attributed to abdominal TB.
Case report
A 9-year-old boy was referred to this facility with complaints of fever, progressive abdominal pain and swelling, and weight loss for 4 months. There was a positive history of night sweats and contact with a chronically coughing adult relative, but no history of cough in the child and no prior history of immunisation for TB. He had earlier received care for the same complaints at various private and public health facilities including broad-spectrum antibiotics ceftriaxone and metronidazole. Notably, he had had an exploratory laparotomy in a private hospital for acute abdomen owing to suspected bowel perforation from enteric fever a month into the illness. However, the referral notes reported the finding of haemorrhagic peritoneal fluid, but no bowel perforation, cysts or features of abdominal TB were noted.
He was chronically ill-looking, wasted with gross abdominal distension from massive ascites demonstrable by fluid thrill and a ballotable mass extending from the left lumbar region to the umbilical region, and abdominal girth of 85 cm measured 13 cm from the tip of the xiphoid process. Other findings were midline surgical scar, dyspnoea, tachypnoea and bagginess of the rectovesical pouch.
Complete blood count showed lymphocytosis of 15 χ 107L and erythrocyte sedimentation rate (ESR) of 30 mm/hr. Tuberculin skin test was negative. Ascitic fluid was exudative (protein of 9 g/dL), but acid-fast bacilli (AFB) and geneXpert tests of the fluid were negative. The child's HIV status was negative on 2 separate occasions during the course of the current illness. Chest radiograph showed consolidation of the left mid and lower zones. Abdominal ultrasound showed a rounded, thick-walled cystic lesion with clear contents, measuring 118 χ 132 mm around the epigastric area. Abdominal computed tomography (CT) confirmed the findings of a ring-enhancing hypodense collection 114 χ 131 mm on the jejunal mesentery (Fig. 1a).
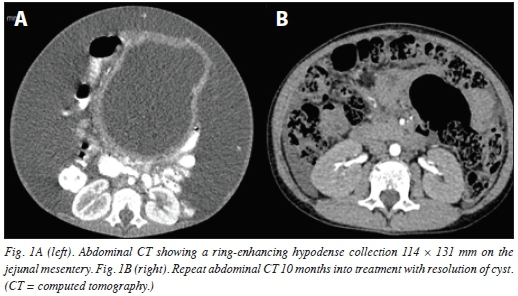
Within 2 weeks, a diagnosis of disseminated TB (chest and abdomen) based on a high index of suspicion was made. The patient was immediately commenced on first-line treatment for TB (rifampicin, pyrazinamide, isoniazid, ethambutol), oral prednisolone for 6 weeks and nutritional rehabilitation. During the early course of treatment, the patient also had 4 abdominal paracenteses to relieve severe abdominal distension and respiratory distress. By the third month of treatment, the patient had improved with reduction in abdominal girth (57 cm, 11 cm from the tip of the xiphoid process), no fever, improved appetite, gained weight and no more respiratory distress. At 6 months, remarkable improvement was noted, with no abdominal distension. At 8 months, there was complete resolution of signs and symptoms, and a repeat abdominal CT scan showed normal findings (Fig. 1b). Other close family members were screened for TB, and the mother and younger sister were found to be positive for TB and commenced on treatment.
Discussion
There are several mechanisms leading to the formation of mesenteric cysts. The theory of mechanical obstruction of the lymphatic system has been favoured over time; however, benign proliferation of non-communicating ectopic lymphatics in the mesentery is also thought to play a role.[4] Obstruction may be due to trauma, infection or neoplasm, leading to solitary or multiple cysts. In spite of the high incidence of TB infection, there are only a few reports about its association with mesenteric cysts.[1,2] More than half of patients with mesenteric cysts present with abdominal pain and abdominal distension.[4] In the presence of TB infection, constitutional symptoms such as fever, weight loss and night sweats may accompany abdominal symptoms.
Detailed radiological imaging using ultrasound, CT scan or magnetic resonance imaging (MRI) is required to aid the diagnosis of mesenteric cyst.[5] Additional supportive investigation should be considered as appropriate. Despite the advances made in the diagnosis of TB, it is important to note that its diagnosis in children may be challenging due to the low yield of diagnostic tests used in adults, therefore making bacteriological confirmation difficult in them. On account of this, treatment is often commenced based on clinical and radiological findings, positive tuberculin test, and contact with an adult with TB.[6] Response to standard treatment for TB with resolution of signs and symptoms may also confirm the diagnosis in retrospect. It is therefore recommended that children with high clinical suspicion for TB should be treated even if advanced testing such as GeneXpert MTB/RIF, a DNA-based test that detects both TB and resistance to rifampicin, is negative.[6]
Differential diagnoses include ovarian cyst, pseudocyst and other causes of abdominal masses. Complete excision of mesenteric cysts by open or laparoscopic procedure has been described as the standard of treatment;[1] however, mesenteric cysts resulting from TB may resolve over time with standard treatment for TB, as in the case of our patient.
Conclusion
Mesenteric cysts are rare conditions, with only few reports associated with TB. Considering the difficulty in confirming the diagnosis of TB in children, a trial of standard treatment for TB may resolve symptoms and signs from mesenteric cyst due to TB infection without the need for surgical intervention.
References
1. Emir H, Yesildag E, Sahin I, et al. A case of mesenteric cysts caused by abdominal tuberculosis. Eur J Pediatr Surg 2000;10(6):402-403. [ Links ]
2. Gujar AA, Rane N, Ambardeka R, et al. A rare case of tuberculous mesenteric cyst. Int J Res Med Sei 2017;3(11):3424-3426. [ Links ]
3. Centers for Disease Control. 2016. Tuberculosis Data and Statistics, https://www.cdc.gov/tb/statistics/default.htm (accessed 24 April 2018). [ Links ]
4. De Perrot M, Bründler MA, Tötsch M, et al. Mesenteric cysts. Dig Surg 2000;17(4):323-328. [ Links ]
5. Erdogan D, Yildiz YT, Boduroglu EC, Tanir NG. An abdominal tuberculosis case mimicking an abdominal mass. Ann Pediatr Surg 2013;9(2):81-83. [ Links ]
6. World Health Organization. Guidance for national tuberculosis programmes on the management of tuberculosis in children. Geneva: WHO, 2014. [ Links ]
 Correspondence:
Correspondence:
H U Ibrahim
ihafsat09@gmail.com
Accepted 7 February 2019














