Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Child Health
versão On-line ISSN 1999-7671
versão impressa ISSN 1994-3032
S. Afr. j. child health vol.13 no.4 Pretoria Dez. 2019
http://dx.doi.org/10.7196/sajch.2019.v13i4.1588
RESEARCH
Characteristics and outcomes of neonates with gastroschisis managed in a public tertiary hospital in a developing country
S GomI; A GrieveII; S VelaphiIII
IMBBS, MMed; Department of Paediatrics, School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIMB MCh, MMed; Department of Paediatric Surgery, School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIIMB MCh, MMed, PhD; Department of Paediatrics, School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
BACKGROUND. High survival rates in neonates with gastroschisis are reported in developed countries. Few studies have reported on prevalence and outcomes of neonates with gastroschisis from developing countries.
OBJECTIVES. To determine prevalence, characteristics and mortality rates in neonates with gastroschisis managed in a public tertiary hospital in South Africa (SA).
METHODS. Hospital records of neonates with gastroschisis managed at Chris Hani Baragwanath Academic Hospital (CHBAH), Johannesburg, SA from 2009 to 2016 were reviewed retrospectively for maternal and infant characteristics, management and outcome at hospital discharge.
RESULTS. A total of 97 neonates were admitted with gastroschisis, of whom 36 were born at CHBAH which had 167 822 live births over the 8-year period (prevalence of 2.1/10 000 live births); the remaining patients were referrals. Over two-thirds of patients were born to primigravida women and were of low birthweight. Complex gastroschisis was found in 36.3% of cases, with the majority (75%) requiring staged reduction. Mortality rate was 57%, with sepsis the most common cause. Factors associated with mortality were low birthweight (odds ratio (OR) 0.19; 95% confidence interval (Ci) 0.04 - 0.80), stage reduction with delayed closure (OR 3.92; 95% CI 1.05 - 14.59), place of birth (OR 4.8; 95% CI 1.44 -16.05) and complex gastroschisis (OR 0.08; 95% CI 0.02 - 0.35).
CONCLUSION. The mortality rate observed in this study was higher than that reported in developed countries. Antenatal diagnosis of this defect and adequate staff training at peripheral hospitals on the initial care and prevention of healthcare-associated infections could improve the outcomes of neonates with gastroschisis in developing countries.
Gastroschisis remains one of the relatively common congenital abnormalities in neonates. A number of studies have reported an increase in its prevalence in the last 10 to 15 years.[1] The International Clearinghouse for Birth Defects, Surveillance and Research reported an increase in the prevalence of gastroschisis beginning in the early 2000s, ranging from 2.04 to 6.46 per 10 000 live births worldwide, with the highest prevalence recorded in Cuba and the lowest in Ireland.[1,2] A study conducted in South Africa (SA), also reported an increase in the number of neonates born with gastroschisis accounting for 15.2% of admissions in 2007 compared with 6.2% in 2003.[2]
Characteristics of neonates with gastroschisis include being born to mothers of younger age, low parity and socioeconomic status and mothers who are tobacco smokers and/or recreational vasoactive drug users.[3] Data collected from 19 European registries showed that up to 77% of neonates born with gastroschisis had intra-uterine growth restriction,[4] thought to be due to loss of nutrients through the exposed bowel. Up to 50% of gastroschisis cases are spontaneous preterm births.[5] Less than 10% of neonates diagnosed with gastroschisis have other associated malformations or anomalies outside the gastrointestinal tract, while 25% have additional gastrointestinal abnormalities such as malrotation, intestinal atresia or stenosis, and volvulus.[6] Intestinal necrosis with severe intestinal inflammation is another common gastrointestinal tract abnormality associated with gastroschisis and is reported in 25 - 50% of cases.[6,7] Survival rates of neonates with gastroschisis in developed countries vary with mortality rates (between 0 - 10% in the USA and ~17% in Europe).[8,9] In developing countries, survival rates are much lower, with mortality rates of 50% and 52% in Brazil and Nigeria, respectively.[10,11] Two studies in other SA centres report mortality rates of 45%[2] and 65% respectively.[12] The quality of care and the infrastructure available at birthing centres affects the survival rate of babies with gastroschisis, as patients born in centres with a neonatal intensive care unit and paediatric surgical facilities are reported to have better outcomes.[13-15] Other factors identified to be associated with increased mortality include bloodstream sepsis,[2] surgical complications of abdominal compartment syndrome, short bowel syndrome, necrotising enterocolitis, the presence of ischaemic intestinal necrosis, intestinal perforation and atresias.[8,9] In the present study, we sought to assess the prevalence of gastroschisis, characteristics of neonates with gastroschisis and outcome at hospital discharge in a resource-limited setting.
Methods
Study design and setting
This was a retrospective descriptive study conducted at Chris Hani Baragwanath Academic Hospital (CHBAH), a public tertiary hospital in Johannesburg, SA, which is affiliated to the University of the Witwatersrand. CHBAH serves the community of Soweto and its surrounding areas with an estimated population of 5.1 million and is a referral centre for healthcare facilities in the southern part of Gauteng Province and North-West Province. The neonatal unit caters for admissions arising from 20 000 live births at CHBAH and 8 000 live births at clinics in Soweto per annum respectively.
Study procedures
Hospital records of neonates who were born and/or admitted at CHBAH between 1 January 2009 and 31 December 2016 with a diagnosis of gastroschisis were retrieved. The following data were collected: maternal characteristics, i.e. maternal age, gravidity, HIV status and place and mode of delivery. Infant characteristics included birthweight, gestational age, sex, the presence of other abnormalities, type of gastroschisis and management of gastroschisis. The primary outcome assessed was survival to hospital discharge. Secondary outcomes included the duration of stay, postnatal age at initiation of enteral feeds, need for mechanical ventilation and presence of probable or culture-confirmed sepsis. An episode of sepsis was defined as either: (i) probable sepsis if a patient had clinical signs and symptoms of sepsis with C-reactive protein levels >40 mg/L in the absence of positive blood culture and clinical condition showing improvement after antibiotic therapy was initiated, or (ii) culture-confirmed sepsis if there was a positive pathogenic organism in the blood or cerebrospinal fluid culture.
Neonates referred from 'other facilities' were categorised into either those originating from within or from outside Gauteng. Neonates were categorised according to birthweight (low birthweight, i.e. birthweight <2 500 g or normal birthweight, >2 500 g) and according to gestational age (preterm, i.e. gestational age <37 weeks or term, i.e. gestational age >37 weeks). Gastroschisis was grouped into either complex or simple gastroschisis based on the presence of other abnormalities of the gastrointestinal tract (atresia or stenosis, necrosis, and perforation i.e. complex gastroschisis) or the absence of other abnormalities (i.e. simple gastroschisis). Surgical management of gastroschisis was defined as either being an operative primary fascia closure or a placement of a silo bag for stage reduction with delayed closure.
Statistical analysis
Statistical analysis was performed using STATA version 15 (StataCorp, USA). Summary statistics were presented as mean values with standard deviation or median values with interquartile ranges (IQR) for parametric or non-parametric data respectively. Comparisons of the characteristics of survivors and non-survivors were performed using Student's i-test or the Mann-Whitney (7-test for continuous variables and the Chi-squared test for categorical variables (Fisher's exact test for values <5). Multivariate logistic regression was performed to assess factors associated with mortality.
Results
Prevalence of gastroschisis
There were 97 neonates admitted with a diagnosis of gastroschisis over the 8-year period (2009 - 2016) and 37.1% of them were born at CHBAH (inborn) with the remaining 62.9% being referrals (out-born). There were 167 822 live births at CHBAH over this time period, therefore the prevalence of gastroschisis was 2.1/10 000 live births. Though there was a trend towards an increase in prevalence over the study period, there was marked variation in annual prevalence varying from as low as 0.50/10 000 live births in 2009 to as high as 4.90/10 000 live births in 2014.
Characteristics of neonates admitted with gastroschisis
The maternal and infant characteristics of neonates admitted with gastroschisis are presented in Table 1. The median maternal age at time of delivery was 20 years. Sixty-eight percent of these neonates were born to primigravida mothers. Most mothers (n=76; 84%), were attending antenatal clinics and 21% of mothers (n=19/89) with known HIV status were HIV positive. The majority of mothers (n=67; 74%) delivered their babies vaginally and the average gestational age of neonates at delivery was 36 weeks. Of all gastroschisis cases, approximately 52% (n=50) were born preterm, 71% (n=69) were of low birthweight, with an average birthweight of 2 270 g.
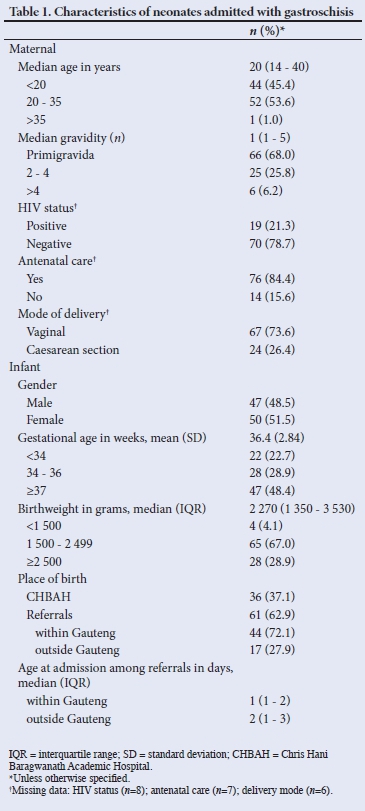
Of the patients who were referred, 72% (n=44) were from Gauteng and the rest from North-West Province. The median (IQR) postnatal age at admission among the referrals was 2 (1 - 3) days, with those from outside Gauteng being admitted a day later than those from within the province who had a median (IQR) age of 1 (1 - 2) day on admission. Only 2.2% (n=2) of gastroschisis cases were diagnosed antenatally.
Types and surgical management of gastroschisis
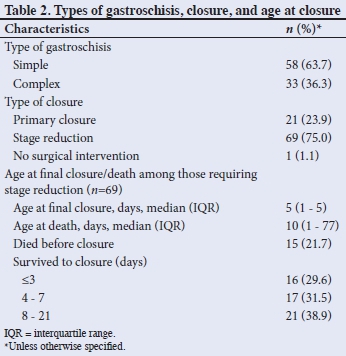
The majority of gastroschisis cases were of the simple type (n=58; 63.7%) and only one neonate had an associated major congenital anomaly that did not affect the gastrointestinal tract (GIT), i.e. spina bifida occulta. Among the neonates admitted with gastroschisis (N=97), data on outcomes were missing in 6 cases and therefore were excluded from further analyses. One patient was not offered any surgical management as she presented with an entirely necrotic bowel and therefore was referred to palliative care. This patient was born at home and only presented on day 3 of life at her base hospital before referral to CHBAH. Among those who were assessed to require active management (n=90), operative primary fascia closure was successful in only 21 patients (23.3%), with the majority (n=69; 76.7%) requiring placement of a silo bag and stage reduction. Of the 69 babies requiring silo stage reduction and delayed closure, 21.7% (n=15) died before final closure could be achieved. Among those who survived to final closure, 29.6% (n=16) were closed within the first 3 days, 61.1% (n=33) within the first week and 38.9% (n=21) closed beyond a week of silo placement. Overall, the median (IQR) age at final closure was 5 (1 -15) days (Table 2).
Secondary outcomes in neonates with gastroschisis
Secondary outcomes assessed were the time it took to start oral feeds, need for mechanical ventilation and presence of sepsis (Table 3). More than half of the patients (n=49; 53.8%) died before oral feeds were commenced. Among those who were started on feeds, the median age at starting oral feed was ~16 (5 - 33) days. The average stay on mechanical ventilation was 13 days, with 61.8% (n=55) staying on the ventilator for more than a week. A total of 62 patients (68%) had at least one episode of sepsis during their stay in the hospital, with the majority (n=45; 73%) having culture confirmed sepsis. Common organisms isolated in neonates with culture-confirmed sepsis were Gram-negative bacteria in 52.4% (n=32) of cases.
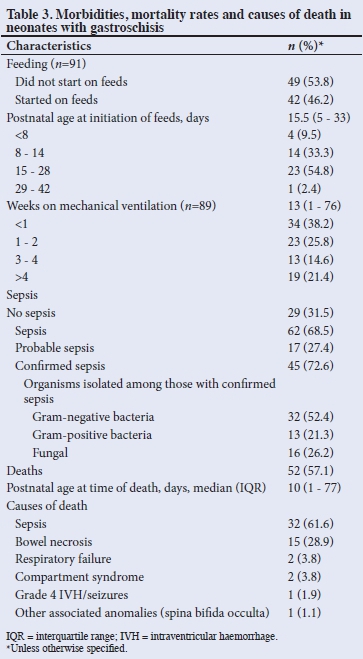
Mortality rate
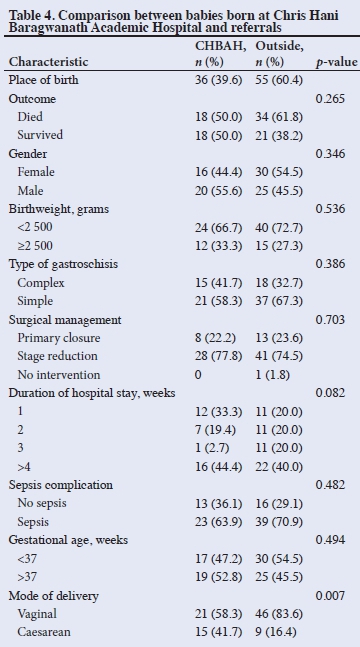
The mortality rate at hospital discharge among neonates with gastroschisis was 57%. The median (IQR) age at death was 10 (1 - 77) days (Table 3). The common causes of death were sepsis (61%) and bowel necrosis (28%). Among the patients who died, 62% died within the first three weeks of admission. On univariate analysis, factors associated with mortality were low birthweight (OR 6.19; 95% CI 1.69 - 22.59; £=0.006); female sex (OR 1.88; 95% CI 1.02 - 3.44; p=0.042); stage reduction with delayed closure (OR 4.69; 95%, CI 1.61 - 13.65; p=0.005) and complex gastroschisis (OR 4.5; 95% CI 1.86 - 10.89; p=0.001). A multivariate analysis showed that complex gastroschisis, stage reduction with delayed closure and low birthweight were associated with mortality, with place of birth also emerging as a predictor of poor outcome (Table 5).
Discussion
The period prevalence of gastroschisis in this study was 2.1/10 000 live births. This is similar to what has been reported in other countries and other centres in SA.[1,12] Though the annual prevalence varied from year to year, there was a trend of an increase in line with other previous reports.[1,2,16] About two-thirds of patients were referrals and <5% were diagnosed antenatally, despite >80% of mothers having received antenatal care. More than 40% of neonates with gastroschisis were born to mothers who were teenagers and >60% were primigravida. Two-thirds of babies with gastroschisis were of low birthweight and about half of them were delivered prematurely. The mortality rate was high at 57.1%, and factors associated with mortality were low birthweight, having complex gastroschisis, delayed surgical repair of the defect and place of birth.
The low antenatal diagnosis of gastroschisis in this study is in contrast to what is reported from the developed world where more than 78 - 83% of patients with gastroschisis are diagnosed on ultrasound antenatally. Currently, obstetric ultrasound is not routinely offered to all pregnant mothers in SA. In the current guidelines for maternity care in this country, antenatal sonography is reserved for high-risk pregnancies only. The lack of antenatal diagnosis of this congenital abnormality could have contributed to the high mortality rate noted in this study, because of delays in getting these patients to a facility that has resources and expertise to manage them. Thus, it is critical that these guidelines are revised to offer all pregnant women antenatal ultrasound to screen for fetal congenital abnormalities.
Previous studies have reported an association between the finding of gastroschisis and young maternal age, low parity, and low birthweight.[17,18] The low birthweight is thought to be due to loss of nutrients through the wall of the eviscerated bowel.[4-7] A high index of suspicion for gastroschisis should be considered among pregnant women whose fetuses are noted to have growth restriction. Thus, where resources are limited, and antenatal ultrasonography is offered to selected pregnant women, fetal growth restriction should be included as one of the indications for antenatal sonography. Mortality rates for gastroschisis reported here are similar to those of other centres in SA and other developing countries such as Nigeria and Brazil[10-12] however, they far exceed the mortality rates in developed countries which are <10% of cases.[9,19] The lack of trained clinical personnel, antenatal sonography for the diagnosis of gastroschisis and limited paediatric surgical services contribute to the high mortality observed in developing countries. Delays in transferring neonates to centres with expertise and experience in the management of surgical patients increases the likelihood of gut exposure to external non-sterile environments, thereby increasing the risk of infection and/or inflammation. Inflammation of the bowel results in swelling of the bowel, making it difficult to achieve primary closure. Delays in the closure of gastroschisis are known to result in delay in starting enteral feeding, requiring prolonged periods of total parenteral nutrition and use of central venous access.[20] Use of central lines and prolonged use of parenteral nutrition has been shown to be associated with an increased risk of healthcare-associated infection.[20] Thus, the high sepsis rate and its related mortality reported in this study could partly be due to the low primary closure rate of about 24%. A study that reported a higher primary closure rate under similar settings as this study reported a relatively lower mortality rate. The other contributor to mortality was extensive bowel necrosis, suggesting inadequate care of bowel post-delivery. This highlights the importance of adequate training of all medical personnel at birthing centres involved in the care of neonates with gastroschisis.
Consistent with the report by Steven et al.,[12] the present study found female neonates (with gastroschisis) were associated with poorer outcomes. Delayed closure was also associated with higher mortality than primary closure. Previous studies have shown variable results regarding time of closure and outcome, with some showing no significant difference in outcome parameters between the primary closure group and the stage reduction group,[7,21] while others have reported that primary closure is associated with better outcomes compared with stage reduction with delayed closure.[2,22,23] A multivariate regression analysis showed predictors of mortality were complex gastroschisis, stage reduction with delayed surgical closure, low birthweight and place of birth, in line with previous findings.[7,18] Delayed surgical closure most likely increased the duration of stay in the neonatal intensive care unit (NICU), therefore the increased risk for healthcare-associated infections which are often associated with high mortality rates. Place of birth as a predictor of mortality may be a reflection of poorer standards of care available at tertiary centres which may be inadequately equipped to manage these high-risk infants.[12-14,24]
Study strengths and limitations
Two limitations were identified in this study: (i) it is a retrospective rather than a prospective study and (ii) six neonates had incomplete data on outcomes and were excluded in the final analysis, therefore the mortality rates may be under- or overestimated. The strengths of the study were: (i) the time period for which data were derived allowed us to observe trends and (ii) the reasonable sample size.
Conclusion
While there has been an overall increase in trends in the prevalence of gastroschisis at our hospital, considerable variation is evident from year to year. A high number of neonates with gastroschisis were referrals, underscoring the need for antenatal obstetric ultrasound screening for congenital abnormalities so that these neonates can be timeously delivered to hospitals with adequate surgical services and intensive care. Training of clinical personnel at birthing centres will ensure better standards of care for babies who may have missed antenatal diagnosis. Expanding neonatal intensive care training and services to avoid delays in referrals and limit healthcare-associated infections and deaths in neonates presenting gastroschisis should be major priorities.
Declaration. I, Simon-Peter Terumbur Gom declare that this research report is my own work. It is being submitted in partial fulfilment
for the award of the Master of Medicine (MMed) paediatric degree in the Department of Paediatrics, University of the Witwatersrand, Johannesburg. This work has never been submitted before for any degree or examination at this or any other university and has not been published in other journal or scientific publication.
Acknowledgements. This work would not have been possible without the intellectual support of Professor Sthembiso Velaphi. I acknowledge the contribution of Dr Andrew Grieve which brought this work to fruition. I am thankful to Professor Peter Cooper and Professor Asharaf Coovadia. Special thanks to Dr Karen Petersen and Dr Firdose Nakwa and all my trainers and the entire Department of Paediatrics at CHBAH for allowing access to patient records and the support staff, in particular, Ms Kei Mabokela.
Author contributions. SG conceptualised the study, collected and analysed the data and wrote the initial draft. SV reviewed the initial draft and supervised the entire work. AG reviewed the draft and assisted with data collection.
Funding. None.
Conflicts of interest. None.
References
1. Mastroiacovo P, Lisi A, Castilla EE, et al. Gastroschisis and associated defects: An international study. Am J Med Genet A 2007;143A(7):660-671. https://doi.org/10.1002/ajmg.a.31607 [ Links ]
2. Sekabira J, Hadley G. Gastroschisis: A third world perspective. Pediatr Surg Int 2009;25(4):327-329. https://doi.org/10.1007/s00383-009-2348-4 [ Links ]
3. Draper ES, Rankin J, Tonks AM, et al. Recreational drug use: A major risk factor for gastroschisis? Am J Epidemiol 2008;167(4):485-491. https://doi.org/10.1093/aje/kwm335 [ Links ]
4. Barisic I, Clementi M, Haeusler M, Gjergja R, Kern J, Stoll C. Evaluation of prenatal ultrasound diagnosis of fetal abdominal wall defects by 19 European registries. Ultrasound Obstet Gynecol 2001;18(4):309-316. https://doi.org/10.1046/j.0960-7692.2001.00534.x [ Links ]
5. Stephenson CDL, MacKenzie AP. Gastroschisis. uptodate. July 18, 2016, ed. University of Cape Town: UPTODATE; 2016. [ Links ]
6. Skarsgard ED. Management of gastroschisis. Curr Opin Pediatr 2016;28(3):363-369. https://https://doi.org/10.1097/MOP.0000000000000336 [ Links ]
7. DAntonio F, Virgone C, Rizzo G, et al. Prenatal risk factors and outcomes in gastroschisis: A meta-analysis. Pediatrics 2015;136(1):e159-e169. https://doi.org/10.1542/peds.2015-0017 [ Links ]
8. Bradnock TJ, Marven S, Owen A, et al. Gastroschisis: One year outcomes from national cohort study. BMJ 2011;343:d6749. https://doi.org/10.1136/bmj.d6749 [ Links ]
9. Davis RP, Treadwell MC, Drongowski RA, Teitelbaum DH, Mychaliska GB. Risk stratification in gastroschisis: Can prenatal evaluation or early postnatal factors predict outcome? Pediatr Surg Int 2009;25(4):319-325. https://doi.org/10.1007/s00383-009-2342-x [ Links ]
10. Uba AF, Chirdan LB. Omphalocoele and gastroschisis: Management in a developing country. Niger J Surg Res 2003;5(1):57-61. https://doi.org/10.4314/njsr.v5i1.12147 [ Links ]
11. Vilela PC, de Amorim MMR, Falbo GH, Santos LC. Risk factors for adverse outcome of newborns with gastroschisis in a Brazilian hospital. J Pediatr Surg 2001;36(4):559-564. https://doi.org/10.1053/jpsu.2001.22282 [ Links ]
12. Stevens P, Muller E, Becker P. Gastroschisis in a developing country: Poor resuscitation is a more significant predictor of mortality than postnatal transfer time. S. Afr J Surg 2016;54(1):4-9. [ Links ]
13. Nichol PF, Byrne JL, Dodgion C, Saijoh Y. Clinical considerations in gastroschisis: Incremental advances against a congenital anomaly with severe secondary effects. Am J Med Genet Part C Semin Med Genet 2008;148C:231-240 https://doi.org/10.1002/ajmg.c.30180 [ Links ]
14. Insinga V, Verso CL, Antona V, et al. Perinatal management of gastroschisis. J Pediatr Neonat Individual Med 2014;3(1):e030113. https://doi.org/10.7363/030113 [ Links ]
15. Drewett M, Michailidis GD, Burge D. The perinatal management of gastroschisis. Early Hum Dev 2006;82(5):305-312. https://doi.org/10.1016/j.earlhumdev.2006.02.003 [ Links ]
16. Beckh-Arnold EMP. Gastroschisis and omphalocoele: Audit at two referral Hospitals in Johannesburg, South Africa: 2000-2005. MSc Med thesis. Johannesburg: University of Witwatersrand, 2011:1-45. [ Links ]
17. Vu LT, Nobuhara KK, Laurent C, Shaw GM. Increasing prevalence of gastroschisis: Population-based study in California. J Pediatr 2008;152(6):807-811. https://doi.org/10.1016/j.jpeds.2007.11.037 [ Links ]
18. Tsai MHH, Chu HR, Yang SM, Lien PH. Clinical features of newborns with gastroschisis and outcomes of different initial interventions: Primary closure versus staged repairs. Pediatr Neonatol 2010;51(6):320-325. https://doi.org/10.1016/S1875-9572(10)60062-9 [ Links ]
19. Caniano DA, Brokaw B, Ginn-Pease ME. An individualized approach to the management of gastroschisis. J Pediatr Surg 1990;25(3):297-300. https://doi.org/10.1016/0022-3468(90)90070-P [ Links ]
20. Sangkhathat S, Patrapinyokul S, Chiengkriwate P, Chanvitan P, Janjindamai W, Dissaneevate S. Infectious complications in infants with gastroschisis: An 11-year review from a referral hospital in southern Thailand. J Pediatr Surg 2008;43(3):473-478. https://doi.org/10.1016/j.jpedsurg.2007.10.026 [ Links ]
21. McNamara WF, Hartin CW, Escobar MA, Lee Y-H. Outcome differences between gastroschisis repair methods. J Surg Res 2011;165(1):19-24. https://doi.org/10.1016/j.jss.2010.05.054 [ Links ]
22. Allin BS, Tse WHW, Marven S, Johnson PR, Knight M. Challenges of improving the evidence base in smaller surgical specialties, as highlighted by a systematic review of gastroschisis management. PloS One 2015;10(1):e0116908. https://doi.org/10.1371/journal.pone.0116908 [ Links ]
23. Parihar D, Goel N, Raikwar P, Batra APS, Kaur J, Nandi S. Early primary repair of gastroschisis without general anaesthesia. J Evol Med Dental Sci 2015;4(98):16292-16294. https://doi.org/10.14260/jemds/2015/2403 [ Links ]
24. Woodward GA, Kirsch R, Trautman MS, Kleinman ME, Wernovsky G, Marino BS. Stabilization and transport of the high-risk infant. In: Avery's Diseases of the Newborn. 9th ed. Elsevier Inc, 2012:341-356. [ Links ]
 Correspondence:
Correspondence:
S Gom
Ter_Gom@yahoo.com
Accepted 13 May 2019














