Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Child Health
On-line version ISSN 1999-7671
Print version ISSN 1994-3032
S. Afr. j. child health vol.13 n.2 Pretoria Jun. 2019
http://dx.doi.org/10.7196/sajch.2019.v13i2.1675
OPINION
Early detection of hearing impairment in high-risk neonates: Let's talk about the high-risk registry in the South African context
Risk-based newborn hearing screening has been recommended as an alternative approach by the Joiiit Committee on Infant Hearing (JCIH) in contexts where universal newborn hearing screening (UNHS) is not yet attainable. However, little evidence exists on the relevant risk factors that can be used to facilitate and enhance this method of screening,[1] particularly in low- and middle-income countries where the social determinants of health are vastly different to those in developed contexts - and contextualised risk factors are important for successful screening programmes.[2, 3]
In establishing contextually relevant risk factors for hearing impairment, in any context, the current authors argue that it is important to note the differences between the terms 'aetiology' and 'risk factor', where aetiology is related to a cause-and-effect relationship with the presence of a disease-causing agent.[4] Where such a direct relationship cannot be established between the disease and agent, but a statistical association is present, the term risk factor is used.[4] This definition suggests that a risk factor increases the chances or probability of the occurrence of a condition, while not ali individuais with a risk factor may necessarily present with the condition, whereas the aetiology guarantees the occurrence of the condition. It should therefore be recognised that not ali babies presenting with risk factors for hearing impairment may necessarily present with a hearing impairment. In resource-constrained environments, such a distinction in definition is crucial, as resource allocation tends to be risk/benefit based.
There are a number of rationales for the Identification and use of risk factors for hearing impairment. These include assisting in identifying children who should undergo audiological assessments in geographical regions where UNHS programmes do not exist,[5, 6] identifying children who require medicai and/or audiological monitoring,[7] facilitating the identification of children who are at risk for auditory neuropathy111 and effective primary prevention of disabling conditions, as well as their earlier identification, which allows for tiinely intervention.[8] It is for these reasons that audiologists need to interrogate risk rather than aetiology, specifically in a context such as South Africa (SA), which is faced with many challenges that may potentially result in increased risks for hearing iinpairment. The re-engineering of priinary healthcare to have more emphasis on prevention also makes this interrogation timely for the audiology community. Addressing risk at the primary levei of prevention is important, as mitigation of risk may influence aetiology, arguably in a positive manner, and lead to early and cost-effective identification of hearing impairment in high-risk neonates.
Currently, audiological literature consists of high-risk registries compiled by the JCIH that have evolved over time, as well as a list adapted by the Health Professions Council of SA[91 for the SA context. Despite the JCIH high-risk registries being considered applicable internationally, findings from studies by Beswick et al.[10,11] and Kanji and Khoza-Shangase[12] have shown the need to specifically tailor these to ones context. This highlights the importance of context itself, although it is a neglected risk influencer. In a country such as SA, a context-specific challenge such as the quadruple burden of disease is crucial to consider.
In studies by the present authors that explored risk-based hearing screening within two hospitais in the public healthcare sector in Gauteng Province, SA,[6,12, 13] the need for a clear definition of risk, and the importance of its contextualisation, were raised. One of these studies included 325 babies who had been admitted to the neonatal intensive care unit, high care and/or kangaroo mother care (KMC) wards.[14] Among the case history factors recorded in this cohort, 11 were identifiable on the HPCSA (2018) high-risk registry (Table 1). Despite this high occurrence of factors listed as risks for hearing impairment, none of the 93 babies in this cohort returning for diagnostic audiological assessment presented with hearing impairment. This led the authors to further interrogate the definition of risk, and the influences of risk at presentation of hearing impairment. This interrogation cannot be avoided in a resource-constrained context such as SA, where resource allocation has to be justified, and use of those resources accounted for.
Medicai and technological advancements have led to more advanced medicai care. For example, these advancements have allowed for the survival of preterm neonates. However, despite these advancements, extremely preterm neonates and extremely low birthweight neonates remain at high risk for death and disability.[15, 16] This risk of death and disability may be very different in low- v. high-income countries, which highlights the importance of considerations of the role of context.
Within the SA context, one may argue that the quadruple burden of disease[17, 18] has a significant influence on the types of risk factors associated with hearing impairment. It is around this framework of quadruple burden of disease that the present authors deliberated, and coined the concept of quadruple influence on risk that they introduce in this publication. The authors argue that risk for hearing impairment within the SA context is influenced by four factors. They propose that ali four factors should be carefully considered when assessing risk/benefit and when making planning decisions, particularly within the re-engineered primary healthcare model that the SA health department has adopted. This quadruple influence on risk is depicted in Fig. 1.
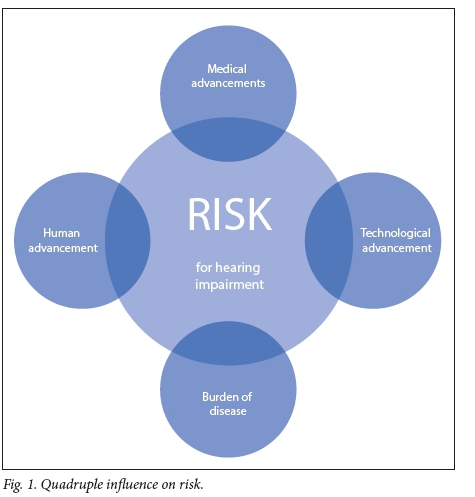
The authors argue that medical advancements, technological advancements, burden of disease and human advancements are factors that influence risk for hearing impairment in the SA context. With regard to medical advancements, as an illustration, although prematurity itself may not be a risk indicator, it may be a risk marker, which predisposes the neonate to other medical conditions requiring management. For example, with medical advancements, preterm neonates prone to septic infections may be detected early and treated with aminoglycosides. However, this medical management may have ototoxic side-effects, which place the neonate at risk for hearing impairment.
As far as technology is concerned, screening for hearing impairment in newborns and infants has progressed, with a variety of objective screening measures now available;[19] this is over and above screening measures for conditions linked to hearing impairment. Technological advancements that influence the identification of medical conditions, as well as their treatments, that impact on hearing function play a significant role in risk definition and its treatment and prioritisation. For example, technological advancements that allow for earlier diagnosis of hyperbilirubinaemia and consequent earlier treatment raise implications for this condition on the risk registry for hearing impairment. Another example would be the use of ventilation to provide respiratory support in preterm neonates, where the impact of the associated noise levels on hearing function (noise-induced hearing loss) has still not been clearly established. Burden of disease is the third factor influencing the risk for hearing impairment debate. Considerations around burden of disease in any given context ensure that risk factors are contextually relevant and contextually responsive. Within the SA context, exclusion of conditions such as HIV/AIDS and tuberculosis (and their treatments) from any risk debate is foolhardy and irresponsible, particularly when considering the high local incidence of these conditions.[20]
Lastly, with regard to human advancement, the present authors argue that as humans advance in terms of their levels of education, awareness and interactions, their identification of, response to and reaction to disease and disability play a major role in the risk-factor debate. The authors also propose that human advancement could indicate the greater level of autonomy that those receiving health services have and continue to gain in relation to their own indigenous knowledge systems and beliefs, which may influence health-seeking behaviour within contexts where their culture has been in the minority - the cultural influence on risk. Khoza-Shangase and Mophosho[21] argue that ignoring linguistic and cultural influences on the provision of clinical services has a significant impact on the efficacy of the services provided.
It is for the above reasons that the current authors propose careful and continuous deliberations around the quadruple influence on risk factors for hearing impairment. Grounding all academic, research and clinical endeavours in context forces the audiology profession to be relevant, responsive and responsible in all its clinical and academic endeavours. It also forces the profession to be cognisant of the influences of diversity in what is believed and done, and to maximise outcomes within SA healthcare spending at a time of low economic growth and fiscal constraint - that is, doing the best, and being efficient, with the limited resources available. Context allows the profession to directly engage with the social determinants of health in SA, and calls on it to play the advocacy role for patients where these are not optimal. This allows the profession to engage in best practice that is poised for next practice in all its clinical initiatives and endeavours.
A Kanji, K Khoza-Shangase
Department of Audiology, Faculty of Humanities, University of the Witwatersrand, Johannesburg, South Africa Amisha.Kanji@wits.ac.za
References
1. Joint Committee on Infant Hearing. Year 2007 position statement: Principles and guidelines for early hearing detection and intervention programmes. Pediatrics 2007;120(4):898-921. https://doi.org/10.1542/peds.2013-0008 [ Links ]
2. Colella-Santos MF, Hein TAD, De Souza GL, Do Amaral MIR, Casali RL. Newborn hearing screening and early diagnostic in the NICU. BioMed Res Int 2014;120(4):1-11. https://doi.org/10.1155/2014/845308 [ Links ]
3. Kanji A, Khoza-Shangase K. Objective hearing screening measures: An exploration of a suitable combination for risk-based newborn hearing screening. J Am Acad Audiol 2018;29(6):495-502. https://doi.org/10.3766/jaaa.16155 [ Links ]
4. Rifkin E, Bouwer E. Cause and effect vs. risk factors. In: Rifkin E, Bouwer E, eds. The Illusion of Certainty: Health Benefits and Risks. Baltimore: Springer, 2007:15-31. [ Links ]
5. Núnez-Batalla F, Trinidad-Ramos G, Sequí-Canet JM, De Aguilar VA, Jáudenes-Casaubón C. Risk factors for sensorineural hearing loss in children. Acta Otoninolaringológica Espanola 2012;63(5):382-390. [ Links ]
6. Kanji A, Khoza-Shangase K. In pursuit of successful hearing screening: An exploration of factors associated with follow-up return rate in a risk-based newborn hearing screening programme. Iranian J Pediatrics 2018;28(4):e56047. https://doi.org/10.5812/ijp.56047 [ Links ]
7. Joint Committee on Infant Hearing. Year 2000 position statement: Principles and guidelines for early hearing detection and intervention programs. Am J Audiology 2000;9:9-29. [ Links ]
8. Olusanya BO. Newborns at risk of sensorineural hearing loss in low-income countries. Arch Dis Childhood 2009;94:227-229. [ Links ]
9. Health Professions Council of South Africa. Early Hearing Detection and Intervention (EHDI) Guidelines. Pretoria: HPCSA, 2018. http://www.hpcsa.co.za/Uploads/editor/UserFiles/downloads/speech/ Early_Hearing_Detection_ and_Intervention_(EHDI)_2018.pdf (accessed 2 January 2019). [ Links ]
10. Beswick R, Driscoll C, Kei J. Monitoring for postnatal hearing loss using risk factors: A systematic literature review. Ear Hearing 2012;33(6):747-756. [ Links ]
11. Beswick R, Driscoll C, Kei J, Khan A, Glennon S. Which risk factors predict postnatal hearing loss in children? J Am Acad Audiol 2013;24(3):205-213. https://doi.org/10.3766/jaaa.24.3.6 [ Links ]
12. Kanji A, Khoza-Shangase K. The occurrence of high-risk factors for hearing loss in very low-birth-weight neonates: A retrospective exploratory study of targeted hearing screening. S Afr J Comm Disorders 2012;59:3-7. [ Links ]
13. Kanji A, Khoza-Shangase K, Ballot D. Hearing screening follow-up return rate in a very low birth weight project: A retrospective record review. S Afr J Child Health 2010;4(4):95-99. [ Links ]
14. Kanji A. Early detection of hearing loss: Exploring risk-based hearing screening within a developing country context. PhD thesis. Johannesburg: University of the Witwatersrand, 2016. [ Links ]
15. Glass HC, Costarino AT, Stayer SA, Brett C, Cladis F, Davis PJ. Outcomes for extremely premature infants. Anesth Anal 2015;120(6):1337-1351. [ Links ]
16. Sutton PS, Darmstadt GL. Preterm birth and neurodevelopment: A review of outcomes and recommendations for early identification and cost-effective interventions. J Trop Pediatrics 2013;59(4):258-265. [ Links ]
17. Department of Health, South Africa. National Health Insurance: Policy Paper. Pretoria: DoH, 2011. [ Links ]
18. Naidoo S. The South African national health insurance: A revolution in healthcare delivery! J Pub Health 2012;34(1):149-150. https://doi.org/10.1093/pubmed/fds008 [ Links ]
19. Kanji A, Khoza-Shangase K, Moroe N. Newborn hearing screening protocols and their outcomes: A systematic review. Int J Pediatr Otorhinolaryngol 2018;115:104-109. https://doi.org/10.1016/j.ijporl.2018.09.026 [ Links ]
20. Khoza-Shangase K. Risk v. benefit: Who assesses this in the management of patients on ototoxic drugs? J Pharm BioAllied Sci 2017;9:171-177. [ Links ]
21. Khoza-Shangase K, Mophosho M. Language and culture in Speech-Language and Hearing Professions in South Africa: The dangers of a single story. S Afr J Comm Dis 2018;65(1):a594. [ Links ]














