Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Child Health
On-line version ISSN 1999-7671
Print version ISSN 1994-3032
S. Afr. j. child health vol.13 n.1 Pretoria Apr. 2019
http://dx.doi.org/10.7196/SAJCH.2019.V13I1.1537
CASE REPORT
Splenic abscess: Conservative management in children
S AroorI; S KanaparthiI; S C MundkurII; S ShashidharaI; K C KondaI
IMD Paed; Department of Paediatrics, Kasturba Medical College, Manipal Academy of Higher Education, Karnataka, India
IIDNB Paed; Department of Paediatrics, Kasturba Medical College, Manipal Academy of Higher Education, Karnataka, India
ABSTRACT
Isolated splenic abscess is rare in children, and occurs predominantly in the immunocompromised, with high rates of mortality and morbidity. We reviewed seven cases of splenic abscess managed at our centre. Six out of seven children (aged 7 months - 15 years, four male and three female) had multiple abscesses. Fever, abdominal pain, hepatosplenomegaly and leukocytosis were the predominant clinical manifestations. Burkholderia pseudomallei and coagulase-negative Staphylococcus aureus were isolated as the causative agents in two children. Five children were successfully managed conservatively, and two with ultrasonography-guided aspiration. Early institution of parenteral antibiotics and ultrasonography-/computed tomography-guided aspiration can help in preventing splenectomy in such children.
Isolated splenic abscess, though rare in children, is associated with high mortality and morbidity. The reported incidence of splenic abscess is 0.2 - 0.7%.[1] Immunocompromised children (with sickle cell anaemia or AIDS, on chemotherapy or suffering from malnutrition) are at increased risk, and diagnosis may be masked if a high index of suspicion is not observed. Moreover, the common manifestations of fever and elevated total leukocyte count may not be seen in immunocompromised children. Splenectomy, the gold standard treatment, has fallen out of favour, given the important immunological functions of the spleen in children. We present seven children with splenic abscess who were managed conservatively at our centre, thereby avoiding splenectomy.
Cases
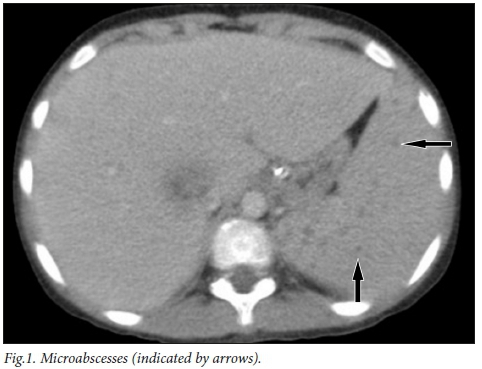
A total of seven children with a diagnosis of splenic abscess were studied. Clinical characteristics and management are described in Table 1. One child had microabscesses in the spleen (Fig. 1, arrows showing microabscesses).
Discussion
Isolated splenic abscess is rare in children, and is more commonly seen in the immunosuppressed and in children with concurrent systemic diseases. Gram-negative, followed by Gram-positive, bacteria are the most frequently isolated organisms from blood and abscess aspirates.[2] Blood and aspirate cultures range from 30 - 73%. Salmonella, Escherichia, enterococci, staphylococci, streptococci, mycobacteria and fungi (Candida, Aspergillus) are the common organisms isolated.[2] An aseptic splenic abscess is also, rarely, seen in autoimmune disorders such as inflammatory bowel disease.[3] Among the seven cases studied in the present group, Burkholderia pseudomallei was isolated from the bone marrow culture of one child. Splenic abscess due to Burkholderia is rare, and usually only seen in immunocompromised children in endemic areas. One child showed coagulase-negative Staphylococcus aureus in blood culture. Abscess aspiration done in two cases showed no growth. The low rate of blood culture positivity was probably due to the commencement of antibiotics in the primary centres from which children were referred. Most of the children were in the age group 11 - 15 years. One child presented at 7 months of age. Splenic abscess in infancy is very rarely reported.[4] In this case, infancy itself is a risk factor, and no other aetiology for immunodeficiency was found. HIV infection and malnutrition were predisposing factors in one child, whereas malnutrition alone was observed in three children. Predisposing factors were not identified in three children.
Fever and abdominal pain were the most common presenting symptoms. Six children (85%) had hepatosplenomegaly and leukocytosis, which is in line with other studies.[2] Hypoalbuminaemia was seen in four cases, indicating the presence of severe infection. One child had disseminated infection with features of shock (tachycardia, hypotension) requiring inotropic support. Pleural effusion, elevated left hemidiaphragm and air-fluid levels in the left hypochondrium may be seen in X-rays. Left-sided pleural effusion was observed in one case. In the present group, six children had multiple splenic abscesses, and one had a solitary abscess. Similarly, Mustafa et al.[5]reported that the incidence of multiple splenic abscesses was higher than that of solitary abscesses. However, in a case series by Choudhury et al.,[2]solitary and multiple splenic abscesses were seen in equal numbers. Ultrasonography (USG) and computed tomography (CT) scans are the most commonly used imaging techniques, with a sensitivity ranging from 75 - 93% and of 96%, respectively. [1] USG was diagnostic in all children in the present study. Magnetic resonance imaging and radionuclide studies are cumbersome procedures and have been replaced by USG and CT.
Splenectomy is the gold standard treatment in adults; however, owing to critical immunological functions of the spleen in children, splenic preservation is highly recommended for children. Resolution of the splenic abscess with antibiotics alone has been reported in the literature. Improvement following splenic abscess aspiration is reported in 50 - 95% of cases, avoiding splenectomy in these patients.[1]
Antibiotic therapy alone is recommended for lesions <3 - 4 cm.[2] Lesions >4 cm would require either needle aspiration or percutaneous catheter drainage.[2,6]
Splenic abscess in immunocompromised children, multiple microabscesses, multilocular abscesses and those with thick fluid tend to respond poorly to aspiration.[1,2] Inability to attain efficient drainage and lack of clinical improvement are the indications for splenectomy[1,2]
Antibiotics are required to treat the associated sepsis in the stabilisation of the child before the procedure. Broad spectrum antibiotics should be started immediately once the diagnosis of splenic abscess is established. Cephalosporins (third or fourth generation), vancomycin plus an aminoglycoside or carbapenem would be an initial choice of antibiotic. Whenever a specific organism is isolated, antibiotics directed against the organism should be selected. The duration of antibiotic therapy is not well established, and is dictated by the underlying disease. When splenectomy is contemplated, vaccination against encapsulated organisms should be administered as soon as possible. Multiple splenic abscesses, Gram-negative bacteria and high APACHE II scores were poor prognostic factors in a study by Chang et al.[6]
All seven cases were successfully managed without splenectomy. There was no mortality in the study group. Two children were treated with USG-guided aspiration and intravenous antibiotics whereas the other five were managed with antibiotics alone. Aminoglycosides, third-generation cephalosporins and metronidazole were used as the first-line antibiotics. The child with Burkholderia was treated with ceftazidime and meropenem, whereas the child with coagulase-negative Staphylococcus aureus was treated with ceftriaxone and amikacin.
Conclusion
Splenic abscess, though a rare entity in children, needs quick assessment and treatment owing to the associated mortality and morbidity. Early institution of parenteral antibiotics and USG- or CT-guided aspiration would help in preventing splenectomy in children. This study further reinforces the importance of conservative management to avoid the potential complications of splenectomy in children.
Acknowledgments. None.
Author contributions. SK and KCK made substantial contributions to the concept, data collection and drafting of the manuscript. SA, SK, SCM and SS were involved in critical revision of the article.
Funding. None.
Conflicts of interest. None.
References
1. Madoff LC. Splenic abscess. In: Bennett JE, Dolin R, Blaser MJ. Mandell, Douglas and Bennett's Principles and Practice of Infectious Diseases. 8th ed. Philadelphia: Saunders, 2015:979-981. https://doi.org/10.1007%2Fs00417-015-2950-1 [ Links ]
2. Roy Choudhury S, Debnath PR, Jain P, et al. Conservative management of isolated splenic abscess in children. J Pediatr Surg 2010;45(2):372-375. https://doi.org/10.1016%2Fj.jpedsurg.2009.10.074 [ Links ]
3. Jordan AJ, Becker K-P, Sertemir M, et al. Multiple aseptic splenic abscesses in a 15-year-old patient. BMC Gastroenterol 2014;14:20. https://doi.org/10.1186%2F1471-230x-14-20 [ Links ]
4. Aslam A, Ahmed Shatla ES, Imanullah S, Bedair EMA. Splenic abscess: A rare complication of the UVC in newborn. Case Rep Pediatr 2014;2014:1-3. https://doi.org/10.1155%2F2014%2F903421 [ Links ]
5. Mustafa M, Menon J, Muniandy R. Splenic abscess: Aetiology, clinical spectrum and therapy. IOSR J Pharm 2015;5(1):2250-3013. [ Links ]
6. Chang K, Chuah S, Changchien C, et al. Clinical characteristics and prognostic factors of splenic abscess: A review of 67 cases in a single medical center of Taiwan. World J Gastroenterol 2006;12(3):460-464. https://doi.org/10.3748%2Fwjg.v12.i3.460 [ Links ]
 Correspondence:
Correspondence:
S Kanaparthi
shravan.1354@gmail.com
Accepted 19 June 2018














