Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Child Health
On-line version ISSN 1999-7671
Print version ISSN 1994-3032
S. Afr. j. child health vol.11 n.4 Pretoria Dec. 2017
http://dx.doi.org/10.7196/sajch.2017.v11i4.1414
RESEARCH
doi:10.7196/sajch.2017.v11i4.1414
Implementation of the Road-to-Health-Booklet health promotion messages at primary health care facilities, Western Cape Province, South Africa
L M Du PlessisI; H E KoornhofII; M L MaraisII; R BlaauwI
IPhD; Division of Human Nutrition, Department of Global Health, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
IIM Nutr; Division of Human Nutrition, Department of Global Health, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
ABSTRACT
BACKGROUND. Age-specific health promotion messages appear in the Road-to-Health booklet (RtHB), an assessment and monitoring tool for child health in South Africa. Healthcare workers should communicate health promotion messages to caregivers at each clinic visit. This investigation was part of a larger RtHB survey.
OBJECTIVE. To assess the implementation of health promotion messages and identify barriers to its successful implementation.
METHODS. A cross-sectional descriptive study with analytical components was conducted in the Western Cape Province. Knowledge and practices of caregivers and healthcare workers were assessed at 143 randomly selected primary healthcare facilities. Information was obtained through questionnaires, direct observation of consultations and recording of health promotion material in facilities.
RESULTS. In total, 2 442 children (0 - 36 months; mean (standard deviation) age 5.10 (6.24) months), 2 481 caregivers and 270 healthcare workers were included. Caregivers' educational level varied, with only 24.3% having completed Grade 12. Healthcare workers had a median of 5 (range 0.5 - 37.0) years' work experience in primary healthcare. All healthcare workers indicated that health promotion messages were important, however, messages were only conveyed in 51% of observed consultations. When it was communicated, health promotion messages were age-appropriate in 97% of cases. Barriers to the implementation of health promotion messages hinged on time and staff constraints, workload and language barriers. Various forms of health promotion material were available in facilities.
CONCLUSIONS. Suboptimal implementation of the health promotion messages in the RtHB are apparent despite healthcare workers realising the importance of health promotion. Barriers to optimal implementation must be urgently addressed by the National Department of Health and healthcare workers in partnership with caregivers and with support from society to promote child health and care.
With the conception of primary healthcare (PHC) at Alma Ata in 1978 to promote health for all, health promotion was included as one of the tools to address the inequality in healthcare globally. The International Conference on Primary Health Care stated that health promotion was also vital to sustain global economic and social development.[1] South Africa (SA)'s first comprehensive Strategic Plan for Maternal, Newborn, Child and Women's Health and Nutrition (2012 - 2016) was launched in 2012.[2] The plan embraces primary healthcare (PHC) and aims to reduce mortality and improve the health and nutritional status of women, mothers, newborns and children through promotion of healthy lifestyles and provision of integrated, high-quality health and nutrition services. At PHC level, the National Department of Health (NDoH) replaced the Road-to-Health card with a Road-to-Health booklet (RtHB) as a national assessment and monitoring tool for child health in February 2011.[3] The RtHB is a comprehensive tool and includes records for the following interventions: immunisation; developmental screening; oral health; health promotion (HP); growth monitoring; infectious diseases, including HIV and tuberculosis; vitamin A supplementation; and deworming. The HP section includes age-specific health promotion messages (HPMs) related to infant and young child feeding, communication and play. It also includes messages about feeding during illness and the danger signs of childhood illnesses. The intention is that healthcare workers (HCWs) should communicate the applicable and age-appropriate messages to caregivers (CGs) at each clinic visit.[3]
Our study formed part of a larger survey which aimed to evaluate the implementation of the RtHB among children aged 0 - 36 months and their CGs attending PHC facilities in the Western Cape Province (WC), SA. This section of the research aimed to assess the implementation of the health promotion component of the RtHB, and to identify barriers to its successful implementation. The implementation of the HP component of the RtHB is reported separately from the larger survey, since this intervention differs from other interventions in the RtHB. While the other interventions in the RtHB are administered to or performed on children and require CGs to attend the clinic, the HP component is focused on behavioural changes in CGs and HCWs' knowledge.
Methods
A full account of the study methodology has been described elsewhere.'41 For this part of the survey, the knowledge and practices of CGs and HCWs with regards to infant and young child feeding (IYCF) and care, and the role of the RtHB in this regard, were assessed.
This survey was conducted over a 3-year period (2012 - 2014) to coincide with the ongoing rollout of the RtHB. A total of 143 PHC facilities across all 6 health districts (Cape Town City, Cape Winelands, Central Karoo, Eden, West Coast and the Overberg) in the WC was surveyed. Two health districts were selected for each year of the survey. Lists of all functional PHC facilities (defined as operational facilities not being renovated or overly involved with other research activities) in each district were obtained from the WC DoH. A random proportional sample of 35% of all facilities was selected from each region. To optimise sample size, PHC facilities with annual attendance figures of <2 000 children aged <5 years were excluded.
All HCWs responsible for the implementation of the RtHB were recruited at each facility, provided informed consent was obtained.
As the rollout of the RtHB continued, children aged 0 - 12 months, 0 - 24 months and 0 - 36 months, as well as their CGs were recruited during years 1 (2012), 2 (2013) and 3 (2014), respectively.
Data collection was conducted over 2 days at each facility to allow sufficient time for interviews and observations. At each facility, consecutive eligible children between the ages of 0 and 36 months were recruited. The CGs of these children were screened and those who met the selection criteria were included in the study. Only CGs with a child of suitable age qualified for participation in the survey. CGs who were unable to converse in English, Afrikaans or isiXhosa, visiting the clinics for specialist services, private or emergency care or not in possession of their children's RtHBs (n=123) ,were excluded. CGs who qualified and who gave informed consent were interviewed using a researcher-administered questionnaire. All questionnaires were professionally translated and available in English, Afrikaans and isiXhosa, and a translator assisted researchers where required. Furthermore, consultations with the HCW were observed.
A pilot project was conducted after all investigators had been trained and standardised. Data from the pilot project were not included in the final analysis. Questionnaires and checklists were tested for face validity during the pilot studies and for content validity by eight experts in the field of dietetics and nutrition.
The researcher-administered questionnaire consisted of two sections: (i) basic demographic information; and (ii) questions on CGs' knowledge and IYCF practices. CGs were asked comprehensive questions about their young child's food intake for the 24-hour period prior to the survey. These questions were structured to list all possible options for infants younger than 6 months and those older than 6 months.
Following the interview, the researcher accompanied the CG to the HCW consultation and completed the observation checklist, noting which messages were included in the consultation, the messages most frequently covered, whether the messages were age-appropriate, and if CGs' understanding of the HPMs was assessed by HCWs.
HCWs who conducted the consultations with the CGs, a maximum of 3 per clinic, were asked to complete a self-administered questionnaire after informed consent was obtained. This questionnaire obtained information on basic demographics, the training which HCWs had received relating to the RtHB, as well as HCWs' knowledge and practices relating to IYCF and HP. HCWs were also asked to report how often they counselled CGs on the HPMs in the RtHB and on their perceived barriers to successful implementation of these messages.
A checklist was completed to assess the use of HP material in clinics, which included posters, pamphlets and other educational aids. The head nurse was also questioned about the existence and perceived success of HP programmes in the facility.
Data were captured and analysed using Microsoft Office Excel and STATISTICA version 12, (StatSoft Inc., USA). Data were presented using descriptive statistics or median (interquartile range (IQR)) values when not normally distributed. The latter were tested with the Shapiro-Wilk test. Contingency tables were used when comparing two nominal variables, and independence was tested using the maximum-likelihood (M-L) χ2 test; a p-value <0.05 was considered statistically significant. In cases where data did not reflect the total study population, the relevant numbers are indicated in brackets.
Ethics approval
Ethical approval was obtained from the Health Research Ethics Committee of the Faculty of Health Sciences, Stellenbosch University (ref. no. N11/09/270) and the research committee of the DoH in the WC. Written informed consent was obtained from the CGs of children visiting the facility, as well as from HCWs responsible for implementation of the RtHB. Participants received a copy of the signed consent form. Confidentiality was ensured by allocating a unique identification number to each participant, which was used throughout the survey.
Results
Demographic information
In total, 2 442 children, 2 481 CGs and 270 HCWs who met all the inclusion criteria were recruited to participate in the survey. The mean (standard deviation (SD)) age of the children included was 5.10 (6.24) months (range 6 weeks - 34.15 months); 50.3% were male (boys, n=1 229 v. girls, n=1 213 (49.7%)). Eleven percent of CGs (n=281/2 481) had received no education or had not completed primary school. Although 44.5% (n=1 105/2 481) had entered secondary school (grades 8 - 12), only 24.3% (n=604/2 481) had completed Grade 12, and 14.7% (n=365/2 481) had achieved a tertiary qualification. The majority of CGs (73.2%; n=1 815/2 477) were in possession of a functional mobile phone. Of the 270 recruited HCWs, most were female (97%; n=262/270) and had received tertiary education (69.3%; n=187/270). Forty-two percent (n=113/269) of HCWs were professional nurses, 16.2% (n=44/269) were enrolled nurses, and 14.1% (n=38/269) were chief professional nurses, all of whom had a median (range) of 5.0 (0.5 - 37.0) years of work experience in PHC.
Health promotion practices on the day of survey
HCWs conveyed HPMs to CGs in 50.8% (n=1 169/2 300) of the observed consultations. Where HPMs were conveyed to CGs during the consultations, the HCWs ensured that CGs understood the messages in 70.9% (n=829/1 169) of cases. The percentage of CGs counselled by HCWs varied significantly between districts, with only HCWs in Eden (63.7%; n=366/575) and West Coast (55.1%; n=216/392) districts conveying HPMs in >50% of observed consultations (p=<0.0001; M-L χ2).
The main HPM discussed with CGs in terms of IYCF was reported to be age-appropriate in 97.2% of cases (n=1 128/1 160). The message most often communicated in the 0 - 6 months age group was that of exclusive breastfeeding (n=330); in the 6 - 12 month age group it was the combination of breastfeeding and complementary feeding (n=106); and for the 12 month - 5 year age group, eating a variety of foods featured most commonly (n=39).
HCWs' knowledge, attitudes, and practices
Forty-six percent of the HCWs (n=124/269) indicated that they 'always' counselled CGs about the HPMs in the RtHB and the rest (except one, who indicated 'never') indicated that they 'sometimes' counselled CGs (53.5%; n=144/269). All of the HCWs indicated that HPMs were important. Their responses also indicated that they felt that they had received adequate training to communicate these messages comfortably (82.6%; n=219/265) to CGs.
Only HCWs who do not always council CGs on HPMs were asked to indicate why they do so Responses were received from 15 HCWs. These reasons related mainly to time constraints (73%; n=11), workload (40%; n=6), staff shortages (60%; n=9), and language barriers (40%; n=6). This resulted in HCWs relaying information in a brief manner, depending on a caregiver's inclination to listen.
HCWs indicated different methods used to communicate the health promotion messages to the mothers/CGs. These methods included among others: reading them to the mother (42.0%); asking questions to establish if the mother/CG understands the messages (76.6%); telling the mother to read the messages at home (55.0%), discussing the messages in detail (53.2%); giving the mother/CG time to ask questions and clarify any misunderstandings (61.7%); and referring the mother to the dietician, if needed (68.8%).
When asked 'At what age do you recommend foods other than breastmilk or formula feeds to be introduced to an infant?' HCWs' answers averaged at ~6 months, with the mean (SD) age recorded as 6.08 (1.45) months. Only 122 HCWs responded to the question, 'For how long do you recommend to a HIV-negative mother that she breastfeeds her infant?' Responses varied between '2 years and beyond' (38.5%), 'between 12 and 24 months' (22.9%) and 'no longer than 6 months' (14.8%). Some HCWs also stated that the mother and baby could continue to breastfeed for as long as they wanted to (15.5%). Other options included 'no longer than 12 months' (6.6%) and 'she should not breastfeed at all' (1.6%).
CG knowledge, and feeding practices
When questioned, 66.3% (n=1 644/2 481) of CGs indicated that they had read the HPMs in the RtHB. Nearly 80% of CGs responded that they understood the messages (79.6%; n=1 308/1 644), 68.7% (n=1 129/1 644) regarded the HPMs as very important and 59% (n=972/1 644) felt that they could make use of the messages. Although in the minority, it was concerning to note that some CGs did not know why HPMs were included in the booklet (2.4%; n=39) and were unsure of what to do with the messages (2.9%; n=47). CGs who indicated that they had not read the HPMs in the RtHB claimed that they were unaware of the HPMs (28.9%; n=242/837), were too
busy (33.2%; n=278/837), did not understand the language (8.4%; n=70/837) were illiterate (4.5%; n=38/837) and did not think that it was important (6.0%; n=50/837).
According to the CGs, HCWs' assessment of CGs' existing knowledge regarding HPMs was shown to be limited. On the day of survey, only 53.0% (n=402/759) of the CGs who reported that they had not yet read the HPMs in the RtHB, actually received counselling on HPM. In addition, in a similar proportion of cases, HCWs did not check to ensure CGs' understanding of the HPMs delivered to those who reported not to have understood the content of the RtHB (25.0%; n=68/272) v. those who reported an understanding (30.5%; n=260/853).
When asked about the meaning of the term 'exclusive breastfeeding, 50.2% (n=1 243/2 478) of CGs were able to respond correctly. CGs' understanding of the term 'exclusive breastfeeding' increased significantly with level of education (p=0.0001, M-L χ2). Significantly more CGs who indicated that they had read the HPM were able to correctly describe the term 'exclusive breastfeeding' (54.4%) compared with those who could not describe the term correctly (45.5%) (p<0.0001; M-L χ2).
Data on feeding practices were recorded for children who were younger (n=651) and older than 6 months (n=785) for the preceding 24-hour period. More children who were <6 months of age received complementary food and drinks such as tea, thin porridge and semisolid or solid food (n=355; 52%) than those who were exclusively breastfed (n=280; 43%) or infant-formula fed (n=36; 5.5%).
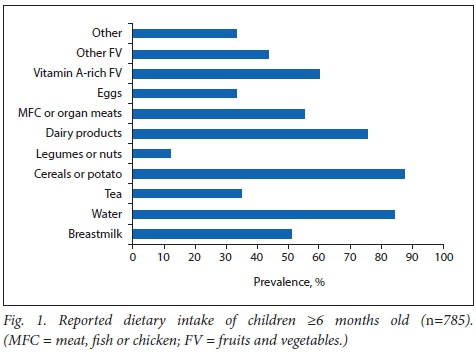
The dietary intake of children (>6 months old) over the previous 24-hour period is shown in Fig. 1. Cereals or potato (87.5%; n=687/785), water (84.3%; n=662/785) and tea (35%; n=275/785) were the most commonly consumed sources of solid foods and fluids, followed by dairy (75.4%; n=592/785), vitamin A-rich fruit and vegetables (60.3%; n=473/785) and meat, chicken, fish or organ meats (55.2%; n=433/785).
No significant differences were found between the feeding practices of CGs who reported that they understood the content of the RtHB (80.2%; n=522/651) compared with those who did not (19.8%; n=129/651) (p=0.88; M-L χ1). In addition, the level of CGs' education was not associated with feeding choice for children who were <6 months old (p=0.702), with the practice of mixed feeding shown to be high among all education levels. The level of education of the CGs of children who were reportedly exclusively breastfed varied as follows: 15.8% (n=44/279) had an education level below Grade 7; 81% (n=226/279) had reached grades 8 - 12; and 3.2% (n=9/279) had a postgraduate qualification. Although more CGs indicated that they had read the HPMs (66%; n=1 644), the feeding practices of those who read the messages did not differ significantly from those who indicated that they had not read them (p=0.78; M-L χ2).
Health promotion programmes and material
The use of resources and materials supporting HP, such as posters, pamphlets, and educational aids, was observed at facilities (n=142). The majority (96.4%; n=137/142) of facilities made use of at least one type of HP resource. Most facilities made use of posters (95.1%; n=135/142) and pamphlets (83.8%; n=119/142) in coloured print, which were mainly sourced from non-governmental organisations (NGOs). Additional sources identified included the DoH, commercial companies, and academic institutes. More specifically, posters and pamphlets on child health were observed in 71 and 57 facilities, respectively. Posters and pamphlets were available in all three predominant languages in the study area, in 68.1% (n=92/135) and 69.7% (n=83/119) of the facilities, respectively. Half of the observed facilities used additional educational aids (n=62/141), such as oral rehydration stations, diagrams, flip charts, books and booklets. The majority of the facilities were running HP programmes (n=111/142) that head nurses perceived to be successful (n=46/51). No data were obtained on the availability of health promoters.
Discussion
This sub-investigation of a larger RtHB survey assessed the implementation of the HP messages, mostly related to IYCF, in the RtHB at the PHC clinic level in the WC, SA and aimed to identify barriers to its implementation.
Both HCWs and CGs expressed their belief in the importance of HP, and almost half of HCWs reported that they 'always' counselled CGs on the HP messages in the RtHB. Similarly, it was observed that half of the HCWs counselled CGs on the HP messages on the day of the survey. The majority of CGs who were counselled on HPMs received age-appropriate messages and HCWs checked the CGs' understanding of the messages. The majority of CGs also indicated that they understood the messages. Two-thirds of CGs indicated that they had read the messages. It was concerning to note that a third of the CGs had not read the messages and were unaware of their presence in the RtHB. Reasons for not counselling CGs on the HPMs hinged on time and staff constraints, as well as workload and language barriers. These barriers correspond with those reported in a national evaluation of services rendered to children <5 years of age in SA. The report revealed that nutrition support, education and counselling is not happening as part of normal service delivery owing to staff shortages, heavy workload and a lack of nutrition-trained personnel.[5]
Improving the nutrition of infants and young children is critical for the improvement of their growth, nutritional status and health, and for the development ofthese children.[6-10] HCWs are considered the key link between policy and practice, placing a responsibility on this cadre to convey, among other, IYCF messages to CGs.[11-15] In order to improve IYCF practices in the country, all contact opportunities between HCW and CG at PHC facilities should be fully utilised. Nutrition and nursing managers should therefore create awareness around the strategic importance of nutrition education and promotion at the PHC level, as stipulated in the Roadmap for Nutrition (2013 - 2017).[16]
SA national data indicate a relatively high breastfeeding initiation rate of 88%,[17] but only ~8% of babies are exclusively breastfed at the age of 6 months. Considering the very low average exclusively breastfed practices in SA, the reported exclusively breastfed practices in this survey seem high. Only half of the CGs could correctly describe the term 'exclusively breastfed', and it is most likely that exclusively breastfed practices were therefore over-reported. Other studies conducted in SA have indicated that the term 'exclusively breastfed' was not well understood or practised.[15,18] A chapter dedicated to breastfeeding in the South African Demographic and Health Survey (2016),[19] concluded that breastfeeding interventions with a solid evidence base for impact were, among others, the education levels of mothers and HCWs on the topic. Consistent and persistent messages on exclusive breastfeeding should therefore be communicated by all HCWs to mothers as a matter of urgency.
SA national data and reviews of national data indicate that a large percentage of infants receive solid foods within the first few days after birth, with an average age of introduction of other liquids/ foods between two and three months.[17,20,21] This trend of introducing solids and other complementary foods or liquids too early has been confirmed by smaller studies in the country.[22-25] From the reported mixed-feeding practices - breastmilk and formula milk, breastmilk and solid food, formula milk and solid food, or a combination of all three feeds - in the current survey, it seems that a large proportion of babies were fed other foods and fluids before the age of 6 months. Data on the complementary diet further revealed that cereal and potato, as well as water and tea, were commonly consumed. A monotonous diet, high in bulky starch and containing low levels of micronutrients, is often used by SA mothers when introducing complementary foods. Water and tea are also commonly introduced fluids. These fluids displace other nutrients in the complementary diet, and in combination with dense, bulky starches of low nutrient density lead to growth faltering.[20]
In SA, both undernutrition and overnutrition are prevalent in young children, which is partly due to poor breastfeeding and complementary feeding practices.[16] Despite economic growth, political and social transition, and the implementation of national nutrition programmes over the past few decades, malnutrition, especially stunting (low height-for-age), remains a stubborn problem that negatively impacts economic growth and prosperity.[26]Combined and focused efforts to improve nutrition during the first 1 000 days of life (from conception to a child's second birthday) can have the most significant impact on stunting. All mothers should therefore receive the best possible nutrition and care during pregnancy, and every mother should be supported to breastfeed her child and introduce safe, adequate, nutritious food from 6 months of age, with continued breastfeeding up to 2 years of age and beyond. This support should, in part, come from HCWs, but should be backed by a whole-of-society approach.[19]
HCWs were of the opinion that they had received adequate training to convey HP messages with confidence. Their knowledge on the period of exclusive breastfeeding and timing of introduction of complementary foods was correct. HCWs knowledge of breastfeeding in the context of HIV was not optimal. According to the Department of Performance Monitoring and Evaluation report, the knowledge and skills of nurses depended upon the amount of nutrition training they had received in the previous 2 years. The report described the nutrition knowledge of nurses as being superficial, and mentioned that this problem was not found in KwaZulu-Natal where nurses had received nutrition training from the University of KwaZulu-Natal.[5-This report also found that behaviour change interventions including nutrition education, breastfeeding support, complementary feeding counselling, and growth monitoring scored lower (<50%) than clinical interventions, which were more effectively implemented.[5] This finding corresponds with global data describing the slow progress on nutrition interventions that require behaviour change modification.[8]
Training of HCWs in nutrition, specifically in IYCN, is a contentious issue, with various international and national research studies indicating the need for refresher courses and retraining of HCWs in basic nutrition messages.[13,14,27-30] The DMPE report suggests the development and implementation of service standards and norms for, among others, nutrition education and counselling, to scale up services and communication to enhance nutrition-related interventions.[5]
Infant feeding practices of CGs who reported to have read and understood the content of the RtHB and those who had not read or understand it were not significantly different. The practice of EBF is more important than the ability to describe the term correctly, yet, significantly more CGs who indicated that they had read the HPM were able to correctly describe the term EBF. CGs' understanding of the term EBF was also shown to increase significantly with their level of education. Creating awareness of the HPMs to CGs as well as a broader investment in human capital, particularly educating teenagers, who are the 'bearers and carers' of the next generation,[31-could improve IYCF in SA.
It is acknowledged that there are challenges to conducting HP in the PHC setting.[32,33] Alternative venues and methods for HP should therefore be investigated. A HP programme initiated by the SA NDoH in 2014, the 'MomConnect' programme, uses cellular phone technology to register pregnant women in both public and private healthcare. The programme empowers women by providing them with all the information and instructions that could ensure a healthy pregnancy and delivery of a healthy baby.[34] After delivery, the messages switch over to focus on information on the health needs of a new-born (including messages on exclusive breastfeeding, immunisation, family planning for the mother, oral rehydration during diarrhoea and check-up periods at the clinic) and continue for up to one year after birth.[35] Since the majority of CGs in this survey owned a mobile phone that was in working condition, the 'MomConnect' programme holds promise as an additional tool to strengthen and reiterate the HPMs in the RtHB.
Study limitations
The format of questioning on EBF knowledge was not ideal. In-depth questioning is necessary to explore this specific practice. Owing to the extent of the questioning on all sections of the RtHB, there was a time limit during the survey that did not allow for in-depth questioning.
Ideally, qualitative data would have complemented the quantitative data collection in this research. Focus group discussions, for example, could have provided more detailed and rich data in this regard.
Conclusion and recommendations
Health promotion to CGs of infants and young children is of critical importance to address the inequality of the health system and to ensure a healthy and productive nation in years to come. HCWs should therefore provide consistent, evidence-based messages and guidelines to CGs of infants and young children. Updates, continuous training and retraining ofHCWs are therefore self-evident. At present, suboptimal implementation of the HPMs in the RtHB is apparent despite HCWs' understanding of the importance of HP and efforts to relay these messages. The barriers to optimal implementation must be addressed by the NDoH in partnership with HCWs and CGs as a matter of urgency and this should be supported by society to enable child health and care to become more promotion-oriented and less reactive.
A checklist of all age-appropriate HPMs could be included in the RtHB to ensure that CGs are counselled on all aspects of IYCF. Currently, the HPMs in the RtHB only appear in English. Pamphlets or pocket-sized folded cards with translated HPMs into local languages could be made available to CGs who are not fluent in English. Educational DVDs could be screened in waiting room areas and other technology, including mobile phone applications, could be utilised to convey HPMs, with cognisance to the educational level of CGs.
Acknowledgements. We would like to convey our sincere thanks to the Western Cape Department of Health, specifically the Sub-Directorate Nutrition, for granting permission to conduct the survey. In addition, we would like to convey our sincere gratitude to all the caregivers, infants and healthcare workers at each facility who participated in our survey. Lastly, we would like to thank all the members of the RtHB survey research group, as well as the administrative staff members of the Division of Human Nutrition and Prof D. Nel from the Centre for Statistical Consultation, Stellenbosch University, for his statistical advice and support.
Author contributions. All authors contributed equally to study conceptualisation and design, data collection, analysis and interpretion, as well as writing the manuscript.
Funding. RB: Stellenbosch University (Fund for Innovation in Rural Research, Harry Crossley Foundation) and Western Cape Department of Health. No funder had any role in the design, analysis or writing of this article.
Road to Health Survey Research Group. Bam N, Blaauw R, Boshoff H, Clarke P, Coetzee C, Daniels L, de Kock I, de Vos I, de Vries K, du Buisson L, du Plessis LM, du Preez U, Ehlers A, Engelbrecht C, Evans N, Ferreira N, Findlay A, Foot J, Fordjour V, Frey C, Groenewald L, Hallinan T, Hartman D, Jackson G, J van Rensburg S, Jooste M, Kamhoot A, Kapena C, Kelly T, Kerbelker R, Koen N, Koornhof HEK, Kotlowitz J, le Grange M, le Roux M, Lee T, Liebenberg S, Louw A, Louw S, Marais ML, Maritz A, Martens A, Meyer I, Mncwabe N, Moens M, Morris N, Naude K, Nel M, Nel S, Nkomani S, Nyenes R, Olivier L, Pienaar T, Pilditch K, Potgieter S, Richardson C, Rickard L, Robinson R, Röhrs S, Samuels S-L, Simjee Z, Slazus C, Smit L, Smit Y, Stander L, Stone P, Strydom E, Strydom K, Swanich L, Swartz P, Swart D, Taverner T, Taylor A, Teuchert N, Turner L, Uys M, van de Venter A, van der Merwe L, van der Schyff S, van Niekerk E, van Rhyn N, van Wyk N, van Zyl F, Venter B, Verster B, Verster J, Visser J, Visser ME, Wasserfall L, Wakelin M, Webber S, Wicomb R, Yeh E.
References
1. World Health Organization (WHO). Declaration of Alma-Ata. International Conference on Primary Health Care. Alma-Ata, USSR. Geneva: WHO, 1978. http://www.who.int/publications/almaata_declaration_en.pdf (accessed 6 June 2017). [ Links ]
2. National Department of Health (NDoH). National Strategic Plan for Maternal, Newborn, Child and Women's Health and Nutrition 2012 - 2016. Pretoria: NDoH, 2012. [ Links ]
3. NDoH. 2nd Triennial Report of the Committee on Morbidity and Mortality in Children Under 5 Years (COMMIC). Pretoria: NDoH, 2014. [ Links ]
4. Blaauw R, Daniels L, du Plessis LM, et al. Assessing the utilisation of a child health monitoring tool. S Afr J Child Health 2017;11(4):174-179. https://doi.org/10.7196/SAJCH.2017.v11i4.1326 [ Links ]
5. NDoH, Department of Social Development, Department of Performance Monitoring and Evaluation, South Africa. Diagnostic/Implementation Evaluation of Nutrition Interventions for Children from Conception to Age 5. Pretoria: NDoH, 2014. http://www.nutritionsociety.co.za/attachments/article/76/Summary-Evaluation-of-Nutritional-Interventions-for-Children-from-Conception-to-Age-5-.pdf (accessed 6 June 2017). [ Links ]
6. Bhutta ZA, Ahmed T, Black RE, et al. What works? Interventions for maternal and child undernutrition and survival. Lancet 2008;371(9610):417-440. https://doi.org/10.1016/S0140-6736(07)61693-6 [ Links ]
7. Dewey KG, Huffman SL. Maternal, infant and young child nutrition: Combining efforts to maximise impacts on child growth and micronutrient status. Food Nutr Bull. 2009;30(2):S187-S189. https://doi.org/10.1016/S0140-6736(07)61693-6 [ Links ]
8. International Food Policy Research Institute (IFPRI). Global nutrition report 2014: Actions and accountability to accelerate the world's progress on nutrition. Washington, DC: International Food Policy Research Institute, 2014. http://www.ifpri.org/publication/global-nutrition-report-2014-actions-and-accountability-accelerate-worlds-progress (accessed 6 June 2017). [ Links ]
9. Martorell R, Horta BL, Adair LS, et al. Weight gain in the first two years of life is an important predictor of schooling outcomes in pooled analyses from five birth cohorts from low- and middle-income countries. J Nutr 2010;140(2):348-354. https://doi.org/10.3945/jn.109.112300 [ Links ]
10. Victora CG, Adair L, Fall C, et al. Maternal and child undernutrition: Consequences for adult health and human capital. Lancet 2008;371(9609):340-357. https://doi.org/10.1016/S0140-6736(07)61692-4 [ Links ]
11. WHO, Global Health Workforce Alliance. Scaling up, saving lives. Geneva: WHO, 2008. http://www.who.int/workforcealliance/documents/Global_Health%20FINAL%20REPORT.pdf?ua=1 (accessed 6 June 2017). [ Links ]
12. Kassier SM, Veldman FJ. Cry, the beloved bottle: infant-feeding knowledge and the practices of mothers and caregivers in an urban township outside Bloemfontein, Free State province. S Afr J Clin Nutr 2013;26(1):17-22. [ Links ]
13. Davies A. PMTCT: How 'informed 'is the literate mother's decision regarding infant feeding options in the Gert Sibande district, Mpumalanga province, South Africa. M Nutr Thesis. Stellenbosch: Stellenbosch University, 2005. http://scholar.sun.ac.za/handle/10019.1/4957 (accessed 6 June 2017). [ Links ]
14. Van der Merwe S, Du Plessis LM, Jooste H, Nel D. Comparison of infant-feeding practices in two health sub-districts with different baby-friendly status in Mpumalanga province. S Afr J Clin Nutr 2015;28(3):121-127. [ Links ]
15. NDoH. Roadmap for nutrition in South Africa 2013 - 2017. Pretoria: NDoH, 2013. [ Links ]
16. Doherty T, Chopra M, Nkonki L, Jackson D, Greiner T. Effect of the HIV epidemic on infant feeding in South Africa: 'When they see me coming with the tins they laugh at me'. Bull World Health Organ 2006;84(2):90-96. http://www.who.int/bulletin/volumes/84/2/90.pdf (accessed: 6 June 2017) [ Links ]
17. Mhlanga RE. Maternal, newborn and child health: 30 years on. In: Barron P, Roma-Reardon J, eds. South African Health Review 2008. Durban: Health Systems Trust, 2008:115-128. http://www.hst.org.za/publications/841 (accessed 6 June 2016). [ Links ]
18. Du Plessis LM, Pereira C. Commitment and capacity for the support for breastfeeding in South Africa. S Afr J Clin Nutr 2013;26(3 Suppl):S120-S128. [ Links ]
19. Du Plessis LM, Peer N, Honikman S, English R. Breastfeeding in South Africa: are we making progress? In: Padarath A, King J, Mackie E, Casciola J, eds. South African Health Review 2016. Durban: Health Systems Trust, 2016:109-123. http://www.hst.org.za/publications/south-african-health-review-2016 (accessed 6 June 2017) [ Links ]
20. Du Plessis LM, Kruger S, Sweet L. Complementary feeding: Critical window of opportunity from 6 months onwards. S Afr JClin Nutr 2013;26(3 Suppl):S129-S140. [ Links ]
21. NDoH Statistics South Africa (SSA), South African Medical Research Council (SAMRC) and ICF. South African Demographic and Health Survey 2016: Key Indicators. Pretoria: NDoH, 2017 [ Links ]
22. Sibeko L, Dhansay MA, Charlton KE, Johns T, Grey-Donald K. Beliefs, attitudes, and practices of breastfeeding mothers from a peri-urban community in South Africa. J Hum Lact 2005;21(1):31-38. https://doi.org/10.1177/0890334404272388 [ Links ]
23. Faber M, Benade AJS. Breastfeeding, complementary feeding and nutritional status of 6-12-month-old infants in rural KwaZulu-Natal. S Afr J Clin Nutr 2007;20(1):16-24. [ Links ]
24. Mushaphi LF, Mbhenyane XG, Khoza LB, Amey AK. Infant-feeding practices of mothers and the nutritional status of infants in the Vhembe District of Limpopo Province. S Afr J Clin Nutr 2008;21(2):36-41. [ Links ]
25. Ghuman MR, Saloojee H, Morris G. Infant feeding practices in a high HIV prevalence rural district of KwaZulu-Natal, South Africa. S Afr J Clin Nutr 2009;22(2):74-79. [ Links ]
26. Said-Mohamed R, Micklesfield L, Pettifor J, Norris S. Has the prevalence of stunting of South African children changed in 40 years? A systematic review. BMC Public Health 2015;534:1-10. https://doi.org/10.1186/s12889-015-1844-9 [ Links ]
27. WHO. Department of Child and Adolescent Health and Development. Implementing the global strategy for infant and young child feeding. Geneva: WHO, 2003. http://www.who.int/nutrition/publications/implementing_gs_iycf_report_content.pdf (accessed 6 June 2017). [ Links ]
28. Savage-King F. Helping mothers to breastfeed. Rev ed. Nairobi: African Medical and Research Foundation, 1992. [ Links ]
29. WHO. Department of Child and Adolescent Health and Development. Child and adolescent health and development: Progress report 2000 - 2001. Geneva: WHO, 2002. http://apps.who.int/iris/bitstream/10665/67435/1/WHO_FCH_CAH_02.19.pdf (accessed 6 June 2017). [ Links ]
30. Menghini KG. Designing and evaluating parent education materials. Adv Neonatal Care 2005;5(5):273-283. https://doi.org/10.1016/j.adnc.2005.07.003 [ Links ]
31. Black RE, Victora CG, Walker SP, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013;382(9890):427-451. https://doi.org/10.1016/S0140-6736(13)60937-X [ Links ]
32. Wills J, Rudolph M. Health promotion capacity building in South Africa. Glob Health Prom 2010;17(3):29-34. https://doi.org/10.1177/1757975910375167. [ Links ]
33. Onya H. Health promotion in South Africa. Promot Educ 2007;14(4):233-237. https://doi.org/10.1177/10253823070140041001. [ Links ]
34. NDoH. Minister Aaron Motsoaledi: Health Department Budget Vote 2015/16. Pretoria: NDoH, 2015. http://www.gov.za/speeches/minister-aaron-motsoaledi-health-dept-budget-vote-201516-5-may-2015-0000 (accessed 6 June 2017). [ Links ]
35. Peter J, Barron P, Pillay Y. Using mobile technology to improve maternal, child and youth health and treatment of HIV patients. S Afr Med J 2016;106(1):3-4. https://doi.org/10.7196/SAMJ.2016.v106i1.10209 [ Links ]
 Correspondence:
Correspondence:
L M du Plessis
lmdup@sun.ac.za
Accepted 17 July 2017.














