Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Child Health
versión On-line ISSN 1999-7671
versión impresa ISSN 1994-3032
S. Afr. j. child health vol.11 no.4 Pretoria dic. 2017
http://dx.doi.org/10.7196/sajch.2017.v11i4.1267
RESEARCH
doi:10.7196/sajch.2017.v11i4.1267
Infant hearing screening in a developing-country context: Status in two South African provinces
K Khoza-ShangaseI; A KanjiI; L Petrocchi-BartalII; K FarrIII
IPhD (Audiology); Department of Speech Pathology and Audiology, School of Human and Community Development, University of the Witwatersrand, Johannesburg, South Africa
IIMA (Audiology); Department of Speech Pathology and Audiology, School of Human and Community Development, University of the Witwatersrand, Johannesburg, South Africa
IIIBA (Speech Hearing Ther); Department of Speech Pathology and Audiology, School of Human and Community Development, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
BACKGROUND. Newborn hearing screening (NHS) programmes are an important step toward early detection of hearing loss and require careful examination and planning within each context. The Health Professions Council of South Africa (HPCSA) has recommended specific contexts in which to actualise early hearing detection and intervention (EHDI) application. It is therefore imperative to explore if, and how, the current experience measures up to these recommendations.
OBJECTIVE. To explore the feasibility and the current status of the implementation of NHS at various levels of healthcare within the South African context.
METHODS. A non-experimental, descriptive, cross-sectional survey research design was employed, using a combination of questionnaires and face-to-face semi-structured interviews. Participants comprised 30 primary healthcare (PHC) nursing managers across two provinces (Gauteng and North West) and 24 speech-language therapists and/or audiologists directly involved with NHS in secondary and tertiary levels of care within Gauteng.
RESULTS. Our findings indicated that there was a lack of formal, standardised, and systematic EHDI implementation at all three levels of health care (primary, secondary and tertiary) with valuable reasons such as insufficient knowledge, lack of equipment, budgetary constraints, and human resource challenges being provided for this. Regardless of the level of care and varied resource allocations and levels of specialisation,EHDI implementation as advocated by the HPCSA in its 2007 position statement currently does not seem feasible, unless the number of barriers identified are addressed, and NHS becomes mandated.
CONCLUSION. Our findings have highlighted the need to ensure that context-specific studies in EHDI are conducted to ensure that national position statements are sensitive to contextual challenges and therefore allow for evidence-based practice, particularly in developing countries where resource constraints dictate success and/or failure of any well-intended programme.
There is a need for context-relevant research aimed at facilitating effective provision of early hearing detection and intervention (EHDI) services in South Africa (SA). Early detection of hearing loss is the initial stage in any EHDI programme, and is conducted by means of newborn hearing screening (NHS).[1] This has become standard practice in developed countries, with universal newborn hearing screening (UNHS) being implemented as a preferred mandated early childhood healthcare standard,[1] unlike in most developing countries where it is not mandated. [2] Adherence to the early intervention principles as they pertain to audiology is the goal of any efficacious intervention programme. These principles include a recommendation for diagnosis of hearing impairment with early intervention services implemented by 6 months of age internationally,[3] and by a maximum of 8 months of age in SA.[4]
In SA, where different levels of healthcare exist, NHS programmes have not been standardised. Evidence indicates that where these programmes are implemented, there are differences between the public and private healthcare sectors, as well as between the various levels of healthcare from primary (such as primary healthcare clinics, community healthcare centres and midwife obstetric units) to secondary and tertiary levels, such as regional and provincial hospitals.[5] The current practice is that where hearing screening occurs, it does so at an individual level with 'targeted' hearing screening being the practice rather than UNHS, and this has also been implemented haphazardly.[6] Targeted hearing screening in babies with risk factors for hearing loss has its pitfalls, particularly where risk factors relevant to the context have not been well documented and categorised. SA, as a developing country, has not been able to implement UNHS or systematic and uniform targeted NHS as part of EHDI for various reasons.[6] Reasons for the lack of EHDI implementation have included, firstly, resource constraints that have forced the SA Department of Health to have key priorities within the health sector. These priorities tend to be focused on saving lives rather than addressing quality of life in individuals with non-threatening conditions, such as hearing loss. Specifically, the burden of life-threatening diseases such as HIV/AIDS and tuberculosis receives higher priority ratings than habilitation services. Secondly, resource constraints in the form of personnel also impact the implementation of UNHS programmes nationally. There is a documented short supply of qualified audiologists in the country in relation to population size, with the public healthcare sector having the most obvious supply-demand mismatch.[7] It is because of this high patient-audiologist ratio that the current authors support de-specialisation of screening services to personnel other than audiologists who can be trained to perform hearing screening with regulated minimum standards to adhere to. Such personnel could include nurses as well as the new planned cadre of professionals in the form of middle-level workers (i.e. audiology technicians). This alternative planning is important when one considers that the developing world is reported to be home to two-thirds of the world's children with hearing loss. In SA, where the public sector sees the highest numbers of people born with hearing loss, the prevalence is 3 - 6 per 1 000 births[2] - this alternative planning is therefore crucial when one considers the negative impact of unidentified and/or late identified hearing impairment.
Detection of hearing impairment may be low on the priority list and presents with comparatively less urgency within the risk/benefit calculation of the DoH. However, there is evidence for the importance of normal hearing function in childhood development. Hearing impairment affects areas such as cognition, language, literacy development and educational competence, social and emotional competence, as well as the individual's vocational and thus financial outcomes - this highlights the importance of EHDI to individuals, families, as well as to societies and governments.[7] It is important that EHDI receives attention in the planning and budgeting of any health department and this should include efficient and effective screening measures to ensure that NHS is conducted in a valid, reliable and ethical manner.
A variety of objective screening measures may be employed within an NHS programme.^6 These include otoacoustic emissions (OAEs), automated auditory brainstem response (AABR), or a combination of OAE and AABR. OAEs have been proven to be simple, fast, and cheaper, but have the disadvantages of providing limited assessment of the auditory system and being negatively impacted by vernix, middle-ear fluid and ambient noise. AABR is known to provide more information regarding the auditory system and has the added advantage of providing better detection of auditory neuropathy in infants. However, AABR does require more knowledge and expertise to conduct than OAEs, which limits the number of screening personnel who can utilise it unless they are trained. AABR is also typically more costly and requires a longer test time compared with OAEs.[6] These factors related to screening measures may influence the implementation of a comprehensive screening programme within different contexts.
Various EHDI position statements recommend the use of different screening measures for different screening contexts. As an example, the Joint Committee on Infant Hearing (JCIH) recommends the use of OAE or AABR for infants admitted to well-infant nurseries and AABR for infants admitted to the neonatal intensive care unit (NICU), while the Health Professions Council of South Africa's (HPCSA)[4] position statement in 2007 recommended the use of AABR for infants who had been admitted to the NICU, and OAE for screening during immunisation visits at PHC clinics within the SA context.[3,4] While the ideal hearing screening measure within the SA context is yet to be defined, it is clear that the use of objective measures which are minimally invasive, and are quick to administer, is key to successful screening programmes.
Given SA's socioeconomic, cultural and linguistic diversity, considerations of congruency in the implementation of international standards to the context is of paramount importance. The HPCSA has recognised the need for contextual and cultural congruency for EHDI to be effective within the SA context.[4] To ensure effective and relevant implementation of EHDI and to continuously improve the limited existing EHDI services, the authors argue for the importance of evidence-based assessments of these international standards within the SA healthcare context. Owing to the paucity of contextually relevant evidence, our study was conducted within the various levels of the public healthcare sector where it has been observed (and reported) that hearing screening is not peformed routinely. It is also within this context that clinical services are most commonly accessed by the majority of South Africans. Localising this research within these levels of public healthcare is also viewed as strategic, particularly with the re-engineering of primary healthcare with the new National Health Insurance plans.
Methods
The aims of the research were to explore the current status of newborn and infant hearing screening (NIHS) at primary healthcare level (clinic-based) and to explore the current status of NIHS at secondary and tertiary care levels (hospital-based).
A non-experimental, descriptive, cross-sectional survey design was employed, using a combination of questionnaires and face-to-face semi-structured interviews. This was conducted within a variety of healthcare contexts, with sampling through non-probability purposive sampling. Participants comprised 30 primary healthcare (PHC) nursing managers across two provinces (Gauteng (GP) and North West (NWP)) and 24 speech-language therapists and/or audiologists who were directly involved with NIHS within Gauteng.
For the PHC nurses to be included in the current research, they were required to be in charge of the PHC clinic's overall functioning, were to be working within either Gauteng or the North West Province; and needed to be conversant in English as the interviews were conducted in English. For the speech-language therapists and/or audiologists to be included in the research, they needed to be qualified and registered with the Health Professions Council of South Africa, be employed within public healthcare facilities at secondary and tertiary levels (hospital based); and be involved in neonatal screening programmes as part of their workload.
Ethical clearance was obtained from the University of the Witwatersrand ethics committee prior to the research being conducted (ref. no. M091040 & M1411105). The structured questionnaire consisted of demographic information, work context, hearing screening context, and information management and quality control. The interviews were also tape recorded. Data from the nursing managers were collected via verbatim documentation of respondents' answers and audio recordings of interviews that were transcribed. Data from the speech-language therapists and/or audiologists were collected from self-administered questionnaires.
To ensure research reliability, controls were exercised pertaining to participant variables, questionnaire and interview parameter, as well as data analysis procedures. Site observations and an independent rater during data analysis, as well as pilot studies, were employed to ensure reliability and validity. Data were analysed qualitatively through descriptive statistics. Data were analysed qualitatively and through thematic content analysis where transcriptions were evaluated to determine and code the emerging themes. Quantitative data analysis, through the use of frequency calculations, were condensed into tabular format for ease of frequency comparisons, and these were then depicted into graphical presentations. Data from the PHC level were handled, analysed and presented separately from the secondary and tertiary levels.
Results
Primary healthcare level
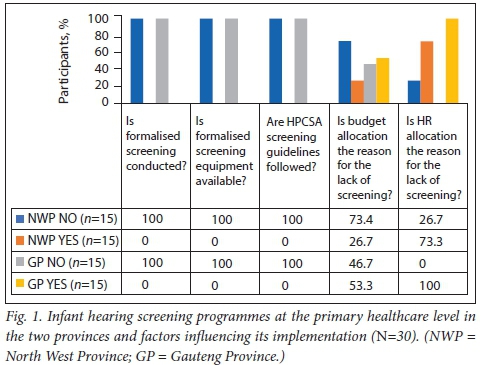
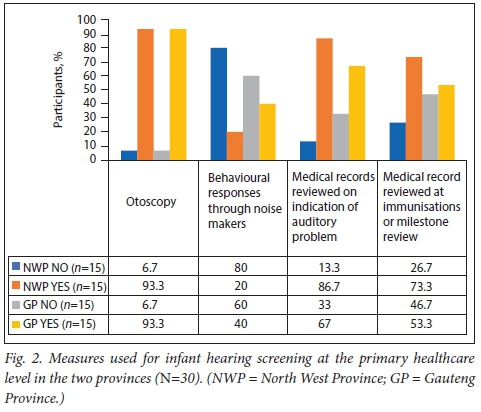
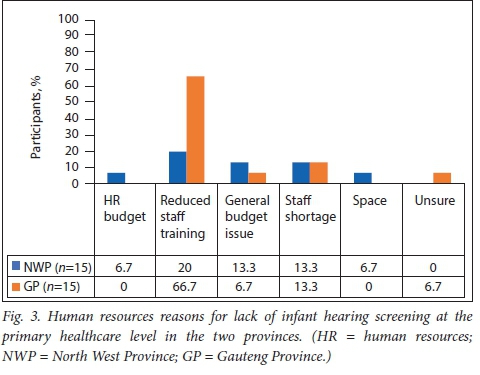
As depicted in Figs 1 and 2, none of the PHC clinics reported offering formalised NIHS. None of the clinics had the necessary equipment to provide hearing screening, with significant reliance on otoscopy and medical record reviews. More than half of the respondents in the Gauteng Province (53.3%) and a quarter of those in the North West Province (26.7%) believed that general budgetary issues were probable reasons for the lack of hearing screening services at their clinics. All the participants in Gauteng and more than two-thirds in the North West (73.3%) cited human resource (HR) restrictions as a major factor in the lack of NIHS programmes in PHC in these provinces. Only 10% (n=3/30; NWP) of respondents cited district management decisions as the reason for the lack of NIHS, where district-level authorisation was required for the execution of NIHS services. Fig. 3 shows the findings of an in-depth analysis of HR-related issues that were cited as factors influencing the implementation of NIHS, including the HR budget, reduced staff training, general budget issues, staff shortages, and space. In both provinces, reduced staff training and staff shortages were the most frequently cited HR-related factors, with reduced staff training being the leading HR challenge cited by 66.7% of the respondents from Gauteng.
Secondary and tertiary level (hospital-based)
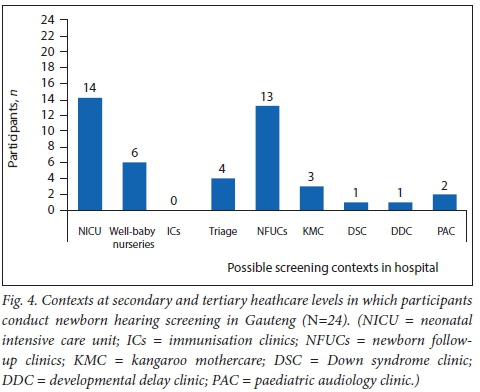
All 24 participants (audiologists and/or speech-language therapists) indicated that they were involved in NHS. Sixteen (67%) reported to be involved in 'targeted' (where only neonates with risk factors are screened) NHS programmes, while 8 (33%) conducted UNHS programmes; 7 of them were employed at tertiary healthcare facilities, which indicates that 'targeted' NHS is the predominant approach used within the hospital context. Regarding the risk factors used for 'targeted' NHS, 5 participants (21%) reported complying with the HPCSA risk factors, 4 (17%) reported using the JCIH recommendations and 4 (17%) reported using risk factors from both position statements. One participant mentioned the use of risk factors that had been adapted from the Gauteng Early Hearing Prevention and Intervention Guidelines (unpublished guidelines developed by the Gauteng National Forum of Audiologists), while 10 (42%) did not respond to the question. It is evident from these results that slightly less than 50% of the participants within the sample were uncertain about the risk factors that informed their protocols and practices. Furthermore, it was evident that great variability exists among audiologists within the Gauteng PHC sector (secondary and tertiary) regarding the risk factors they employed in the NHS programmes -the variation in the age at which infants received their initial hearing screening. For UNHS programmes, all screenings were reported to be conducted before 3 months of age; while 6 months is the cut-off age for 'targeted' NHS. The most commonly listed age for the initial hearing screening was established as 'below 1month of age' by 42% («=10/24) participants. Despite the great variability in our findings, all screening was conducted before 6 months of age.
The various contexts in which participants reported to conduct the initial NHS are shown in Fig. 4. The NICU was found to be the most common screening context reported by 58% of the participants, with screening at newborn follow-up clinics being second (54%) within these levels of healthcare - these values do not add up to 100% as participants could engage in screening at more than one context.
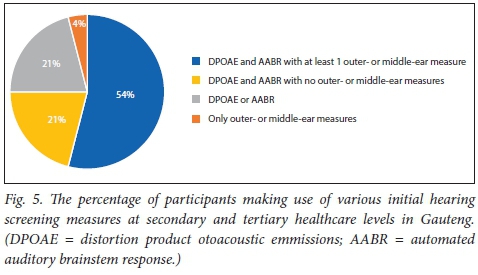
The measures used by participants to conduct initial hearing screenings (as shown in Fig. 5) were as follows: 75% (n=18/24) reported using both distortion product otoacoustic emmissions (DPOAE) and AABR, and 13 of them indicated the additional use of at least one outer-ear or middle-ear screening measure, such as otoscopy, high-frequency (1 000 Hz probe tone) and acoustic reflex screening; 21% (n=5/24) reported using DPOAE and AABR, with no use of outer and middle ear screening measures; 21% (n=5/24) reported using either DPOAE or AABR; and 1 participant reported using only otoscopy and tympanometry for NIHS.
Of the 14 participants who screen in the NICU or at discharge from the NICU, 12 reported making use of AABR as one of the screening measures. Inconsistencies were noted in the measures used by participants across the different facilities as well as within the same facility.
Discussion
Our results revealed that no PHC clinics within the North West and Gauteng were performing formalised hearing screening as endorsed by the HPCSA position statement. Budgetary and HR issues, mainly staff training and staff shortages, were underscored as the main reasons why this clinical service gap of EHDI exists. It was evident that financial reasons were significant factors influencing clinics' staff training, staff complement, equipment availability and physical structure. The documented inequalities in district finance allocation[8] may explain the variation in the responses between the two provinces. Our findings indicate that the recommendations in the HPCSA's 2007 position statement have not been successfully implemented at the PHC level, where 85% of South Africans access healthcare. The inability and failure to implement EHDI has significant repercussions that have been well documented. EHDI services are considered the basis for achieving the most favourable outcomes in infants with hearing loss.[2,4,6] Arguably, our findings might be rationalised within the context of considering the burden of HIV/AIDS and TB in SA, which continue to dominate the health priorities of the national government over non-life-threatening conditions, such as hearing loss.[7] Furthermore, EHDI in SA are in the early stages of development with very little contextual evidence for their effectiveness and applicability.[7] Reports in the literature confirm the importance of advocating for legislation to mandate EHDI,'2,6,71 instead of the current reliance on caregiver concern as the primary identifier of possible hearing loss. Our study aimed to provide contextual evidence to substantially guide the SA EHDI realisation process. Our findings strongly contend that the current HPCSA EHDI clinic guidelines are practicable. At present, fundamental barriers, including reduced resources, staff complement and training, and clinic budgets, preclude successful implementation of the guidelines. Despite these barriers, positive aspects were identified within the PHC immunisation schedule context - respondents were willing to implement formal hearing screening as part of the PHC immunisation schedule and patient return rates for immunisation would ensure a high patient yield.
This may relate to variation in the management of regional priorities and the higher level of authority that district-level governance is now able to employ.'81 To improve local accountability, decentralised management of health districts has been reinforced within the DoH strategic plan'8-and the HPCSA position statement recommends the inclusion of the accountable DoH division to jointly facilitate the appropriate hearing screening programme.[4] NIHS and the HSPCA 2007 guidelines need to be more adaptable to district-level hearing and screening practices, to make them fit for and applicable to the screening process. Petrocchi-Bartal and Khoza-Shangase[7] recognise that the SA PHC sector is frequently less resourced than the advanced private healthcare sector. Theunissen and Swanepoel[9] referred to a shortage of equipment and staff as the main factors influencing NHS services in the SA context, and this is supported by our findings. The lack of staff training was stated as the main contributing factor to lack of NIHS in PHC. Although our study revealed important findings about the PHC context and SA EHDI initiatives, we included only 30 clinics from two provinces, which limits the generalisability of the findings.
The results from secondary and tertiary levels of care indicate the use of a 'targeted' approach to NHS. This is in contrast to the HPCSA's call for the implementation of UNHS. This call for widespread UNHS was based on at least two studies,[6,10] which reported that reported 50% of congenital hearing losses would be missed in the case of 'targeted' NHS, as not all children with congenital hearing loss present with risk factors. Nine years after the position statement was released, it is evident that a complete move from 'targeted' to universal NHS has not been made. Theunissen and Swanepoel[9] found that UNHS was conducted in just 2% of the hospitals included in their study. Although the current research considered the protocols that are adhered to by individual audiologists and not the general hospital protocols, our findings suggest that adherance to UNHS protocols is increasing compared with those of Theunissen and Swanepoel.[9]
Regarding the NHS protocols adhered to by participants, variation was noted between the participants from different research sites, as well as between participants employed within the same facility. Inconsistent responses were found with regard to the risk factors that were adhered to for NHS. This was noted for both the general risk factors as well as risk factors that are specific to the delayed-onset hearing loss. There was also variation in the age at which initial hearing screening was conducted. The HPCSA[4] stipulates that the protocols that are developed and carried out may vary between contexts because they need to be tailored to the specific needs of the community and the facilities. Furthermore, the programmes need to be developed in a way that maximises follow-up and ensures minimal false-positive results.[4] However, the HPCSA position statement[4] outlines that a team of professionals who are responsible for the screening within each specific context must develop the protocol to ensure minimal variation within a healthcare facility. Theunissen and Swanepoel[9] reported similar findings of variability and reported that screening procedures across Gauteng were unsystematic. They also reported that hearing screening was not routinely conducted as per the recommendations in the HPCSA and JCIH EHDI position statements. The World Health Organization (WHO)[11] makes note of the existence of similiar protocol variations as were discovered in our study and states that this variation is not necessarily due to financial or technological differences but rather to educational differences and the varying value that is placed on NHS, which emphasises the importance of adequate NHS education in obtaining standardised procedures.
With regard to the measures used for screening, the majority of the participants reported having access to objective screening measures. These measures are endorsed by the HPCSA[4] EHDI position statement because they display excellent sensitivity and specificity for hearing loss detection. The HPCSA endorses the use of both OAEs and AABR for different screening environments. As AABR is more sensitive to neural pathologies and infants who stay in the NICU are at a greater risk for developing neural pathologies, the HPCSA recommends AABR for screening in this environment.[6] We found that this stipulation was being complied with by the majority of the participants at the secondary and tertiary levels of care, as only two of the participants screening in NICU contexts reported not including the use of AABR in their test battery.
Conclusion
Our findings emphasise the importance of carefully structured studies evaluating the applicability of the HPCSA 2007 protocol implementation. Continuously assessing hearing screening protocol guidelines and/ or position statements ensures evidence-based practice and enforces programme implementation that is contextually relevant and explicit at any given point in time. This is especially true where programme application can be significantly affected by barriers such as reduced resources. Current findings also illustrate the importance of political support for the implementation of programmes. Mandating NHS by the NDoH will not only ensure regulations around EHDI, but will also facilitate resource allocation to ensure that services are delivered.
Careful planning with regards to research focus within the SA context should have standardisation of NHS protocols as a priority in order to allow for evidence-based implementation. Successful implementation will require careful compilation of protocols, collaboration between staff at facilities within specific districts and/or provinces as well as between the various levels of healthcare, discussion at provincial and national forums, and the provision of in-service training of audiologists, and other professionals, about correct NHS practices and protocols may further aid the implementation of standardised practice. Additionally, there is a need for research on the NHS practices at a national level. This research should be ongoing to determine the changes in NHS practices and whether these practices are improving in terms of the alignment with HPCSA recommendations. Information from the research along with data on the benchmark and quality indicators stipulated in the HPCSA 2007 position statement will assist in continually evaluating the status of EHDI in SA. Further research may discover improved methods for ensuring that the NHS and post-neonatal care pathways are sustainable in the public healthcare sector.
Acknowledgements. None
Author contributions. All authors contributed equally to the preparation of the manuscript.
Funding. None
Conflicts of interest. None
References
1. Burke M, Shenton RC, Taylor MJ. The economics of screening infants at risk of hearing impairment: An international analysis. Int J Pediatric Otorhinolaryngol 2012;76:212-218. https://doi.org/10.1016/j.ijporl.2011.11.004 [ Links ]
2. Khoza-Shangase K, Michal G. Early intervention in audiology: Exploring the current status from a developing country context. Br J Med Medic Res 2014;120(4):2238-2249. https://doi.org/10.9734/bjmmr/2014/7322 [ Links ]
3. Joint Committee on Infant Hearing. Year 2007 position statement: Principles and guidelines for early hearing detection and intervention programs. Pediatrics 2007;120(4):898-921. https://doi.org/10.1542/peds.2007-2333 [ Links ]
4. Health Professions Council of South Africa. Early Hearing Detection and Intervention Programmes in South Africa, Position Statement Year 2007. http://www.hpcsa.co.za/Uploads/editor/UserFiles/downloads/speech/early_hearing _detection_statement.pdf (accessed 14 December 2017). [ Links ]
5. Cullinan K. Health services in South Africa: A basic introduction. 2006. http://www.health-e.org.za/wp-content/uploads/2013/04/Health_services_briefing_doc.pdf (accessed 15 April 2016). [ Links ]
6. Kanji A, Khoza-Shangase K. Feasibility of newborn hearing screening in a public hospital setting in South Africa: A pilot study. S Afr J Comm Disorders 2016;63(1):a142. https://doi.org/10.4102/sajcd.v63i1.150 [ Links ]
7. Petrocchi-Bartal L, Khoza-Shangase K. Infant hearing screening at primary healthcare immunisation clinics in South Africa: The current status. S Afr J Child Health 2016;10(2):139-143. https://doi.org/10.7196/SAJCH.2016.v10i2.1114 [ Links ]
8. National Department of Health (NDoH). Strategic plan 2010/11 -2012/13. Pretoria: NDoH, 2010. http://www.nationalplanningcycles.org/sites/default/files/country_docs/South%20Africa/ south_africa_strategic_health_plan_2010-2013.pdf (accessed 29 May 2010). [ Links ]
9. Theunissen M, Swanepoel DW. Early hearing detection and intervention services in the public health sector in South Africa. Int J Audiol 2008; 47(Suppl 1):S23-S29. https://doi.org/10.1080/14992020802294032 [ Links ]
10. Chu K, Elimian A, Barbera J, Ogburn P, Spitzer A, Quirk JG. Antecedents of newborn hearing loss. Obstet Gynecol 2003;101(3):584-588. https://doi.org/10.1097/00006250-200303000-00027 [ Links ]
11. World Health Organization. Newborn and Infant Hearing Screening: Current Issues and Guiding Principles for Action. Geneva: WHO, 2010. [ Links ]
 Correspondence:
Correspondence:
K Khoza-Shangase
Katijah.Khoza@wits.ac.za
Accepted 29 March 2017














