Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Child Health
On-line version ISSN 1999-7671
Print version ISSN 1994-3032
S. Afr. j. child health vol.11 n.4 Pretoria Dec. 2017
http://dx.doi.org/10.7196/sajch.2017.v11i4.1326
RESEARCH
doi:10.7196/sajch.2017.v11i4.1326
Assessing the utilisation of a child health monitoring tool
R BlaauwI; L DanielsII; L M du PlessisI; N KoenI; H E KoornhofIII; M L MaraisIII; E van NiekerkI; J VisserIV
IPhD (Nutr) Division of Human Nutrition, Tygerberg Academic Hospital, Stellenbosch University, Cape Town, South Africa
IIMPH; Division of Human Nutrition, Tygerberg Academic Hospital, Stellenbosch University, Cape Town, South Africa
IIIM Nutr Division of Human Nutrition, Tygerberg Academic Hospital, Stellenbosch University, Cape Town, South Africa
IVM (Nutr); Division of Human Nutrition, Tygerberg Academic Hospital, Stellenbosch University, Cape Town, South Africa
ABSTRACT
BACKGROUND. The Road-to-Health booklet (RtHB), a standardised national tool for growth monitoring and the assessment of health among children from birth to five years of age, was introduced in South Africa in February 2011.
OBJECTIVES. The study assessed the implementation of growth monitoring and promotion, immunisation, vitamin A supplementation, and deworming sections of the RtHB. Caregivers' (CGs) and healthcare workers' (HCWs') knowledge, attitudes and practices were investigated as well as HCWs' perceptions of barriers undermining implementation.
METHODS. A cross-sectional descriptive study was conducted on a proportional sample of randomly selected primary healthcare facilities across six health districts (35%; n=143) in the Western Cape Province. HCWs involved in the implementation of the RtHB booklet, children (aged 0 - 36 months) and CGs were included. Information was obtained through scrutiny of the RtHB, observation of consultations and structured questionnaires.
RESULTS. A total of 2 442 children, 2 481 CGs and 270 HCWs were recruited. Weight measurements (94.7%, n=2 251/2 378) were performed routinely. Less than half (40.2%; n=997/2 481) of CGs reported that their child's growth had been explained to them. Sixty-eight percent of HCWs (n=178/260) correctly identified criteria for underweight classification, whereas only 55% (n=134/245) and 39% (n=95/245) could do so for stunting and wasting, respectively. The RtHB sections were completed adequately for immunisation (89.3%; n=2 171/2 431) and vitamin A supplementation (94.6%; n=1 305/1 379) but not for deworming (48.8%; n=176/361). Most HCWs (93%; n=209/223) knew the correct regimens for vitamin A supplementation, but few CGs knew when treatment was due for vitamin A supplementation (16.4%, n=409/1 646) and deworming (26.2%; n=650/2 481). Potential barriers identified related to inadequate training, staff shortages and limited time.
CONCLUSION. Focused efforts and resources should be channelled towards HCWs' training and monitoring regarding growth monitoring and promotion to optimise utilisation of the RtHB. Mobilisation of community health workers is needed to strengthen community awareness of preventive health interventions.
Nearly half of all deaths in children under five is caused by malnutri-tion.[1] This is not only due to a lack of sufficient and adequately nutritious and safe food, but also various processes that involve among others healthcare, education, sanitation and hygiene. Good nutritional status leads to higher individual earnings and mental acuity, which in turn support macroeconomic and societal growth.[2] Therefore, malnutrition impairs productivity, which poses a strain on national growth. In this regard malnutrition represents a barrier to the successful achievement of the Sustainable Development Goals (SDGs).[2]
The importance of growth monitoring and promotion (GMP) as part of preventive and curative health to reduce malnutrition and mortality is recognised worldwide.[3] The South African (SA) government is committed to reducing mortality and morbidity among mothers and children as reflected in the key strategic outcomes for the health sector.'4-The Road-to-Health chart (RtHC), which was based on the National Centre for Health Statistics (NCHS) reference data, was previously used as a child health monitoring tool in SA. This two-page patient-held record was used to assess weight-for-age and to chart immunisations, deworming, and vitamin A supplementation;[5,6] however, appropriate implementation of this tool was a challenge.[6] In 2007, an evaluation of the RtHC conducted in three public healthcare centres in Gauteng Province showed that it was not used effectively as a curative, preventive or promotive tool for monitoring child health as neither healthcare workers (HCWs) nor parents utilised it optimally.[5]
A revision of the RtHC in SA was necessary owing to the 2006 release of the World Health Organization (WHO) growth standards, the increasing prevalence of childhood stunting, overweight and obesity and changes made to childhood immunisation schedules. A 28-page Road-to-Health booklet (RtHB) was developed to be used nationally as of February 2011. It includes the following preventive and treatment interventions: immunisation; developmental screening; oral health; health promotion; growth monitoring; infectious diseases (including human-immunodeficiency virus (HIV) and tuberculosis (TB)); vitamin A supplementation; and deworming.[7]
This survey aimed to assess the implementation of the RtHB among infants and children (referred to collectively as children) aged 0 - 36 months and their caregivers (CGs) attending primary healthcare (PHC) facilities in the Western Cape Province (WC), SA.
The objectives were to: (i) evaluate the implementation of GMP, immunisation, vitamin A supplementation (6 - 36 months), and deworming components of the RtHB; (ii) investigate the knowledge, attitudes and practices of both CGs and HCWs relating to these components; and (iii) identify HCWs' perceptions of the barriers undermining appropriate implementation of the RtHB.
Methods
Ethical disclosure
The survey was approved by the Health Research Ethics Committee of Stellenbosch University (ref. no. N11/09/270) and the research committees of the Department of Health (DoH), WC, and the City of Cape Town.
Written informed consent was obtained from the CGs of children visiting the facility, as well as from HCWs responsible for implementation of the RtHB. Participants received a copy of the signed consent form. Confidentiality was ensured by allocating a unique identification number to each participant, which was used throughout the survey.
Sample selection
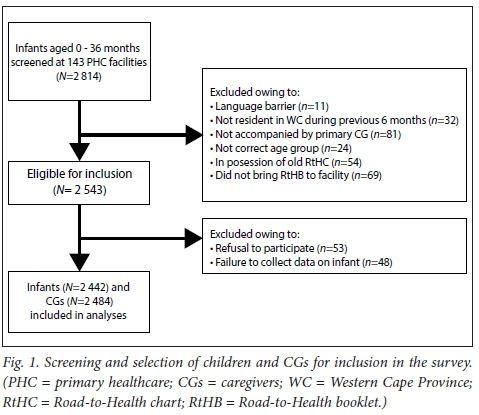
To coincide with the ongoing rollout of the RtHB, this survey was conducted over three phases during the period 2012 to 2014. A total of 143 PHC facilities across all 6 health districts in the WC were surveyed. Two health districts were selected for each phase of the survey. Lists of all functional PHC facilities (defined as operational facilities not being renovated or overly involved with other research activities) in each district were obtained from the WC DoH. A random proportional sample of 35% of all facilities was selected from each region. To optimise the sample size, PHC facilities with annual attendance figures of <2 000 children aged <5 years were excluded.
During each phase of the survey, all HCWs responsible for the implementation of the RtHB were recruited at each facility, provided that informed consent was obtained. As the rollout of the RtHB continued, children aged 0 - 12 months, 0 - 24 months and 0 - 36 months, as well as their CGs, were recruited during phases 1, 2, and 3, respectively.
Children and their CGs were eligible for inclusion if CGs were present and in possession of the new RtHB, were able to communicate in English, Afrikaans or isiXhosa (the three official languages in the WC), and if they had resided in the WC for 6 months prior to the survey. Children and CGs were excluded if they attended the facility for a reason unrelated to the child, or if emergency medical care was required. In the case of more than one child per CG, only one child was selected with the use of a simple randomisation procedure. Where possible, children and their CGs were recruited consecutively, once informed consent was obtained.
Data collection
Data were collected over a period of 2 days at each facility. Investigators were required to scrutinise the RtHB of every child included in the study and attended consultations between HCWs, children and their CGs. Investigators used a checklist to document their observations which assessed the implementation of each component of the RtHB. In addition, clinical notes and referrals made by HCWs, as well as communication of return visits with CGs, were recorded. Missed opportunities - defined for the purposes of this survey as 'the failure to provide appropriate monitoring, treatment, or intervention on the day of data collection' - were also noted.
Anthropometric measurements performed by HCWs were observed and evaluated according to the guidelines described in the WC RtHB training package.'71 Based on guidelines described in the training package,171 the checklist included a step-by-step description of all relevant anthropometric measuring and plotting procedures, including weight-for-age, length/height-for-age, and weight-for-length/height growth charts. The checklist also collected information on how each section of the RtHB had been completed by HCWs.
An additional checklist was used to evaluate the accuracy and availability of anthropometrical apparatuses at each facility. Length boards were calibrated against a known 1 m non-flexible length and paediatric scales against known 2 kg, 5 kg, and 10 kg weights. Inaccurate equipment was corrected at each facility, where possible, once data collection was completed.
Questionnaires were used to document CGs' and HCWs' sociodemographic information, knowledge, attitudes, and practices (KAPs) relating to each component of the RtHB, as well as perceived barriers to the successful implementation of the tool. Self-administered questionnaires were completed by HCWs, whereas CG questionnaires were completed by investigators during a structured interview. All questionnaires were available in English, Afrikaans, and isiXhosa and were completed with the assistance of a translator where necessary.
All investigators underwent training and standardisation, followed by a pilot study. Data from the pilot study were not included in the final analysis. Questionnaires and checklists were tested for face validity during the pilot study and for content validity by 8 experts in the field of dietetics and nutrition.
Anthropometric measurements were analysed using the WHO Anthro programme. Underweight, stunting and wasting were expressed as the proportion of individuals with Z-scores below -2 SD.[8,9] Overweight and obesity were expressed as the proportion of individuals with weight-for-length/height Z-scores above 2 SD and 3 SD, respectively. [8,9] In children who were >6 months old, a mid-upper arm circumference (MUAC) value of >11.5 cm and <12.5 cm was regarded as moderate acute malnutrition, while a MUAC value of <11.5 cm was classified as severe acute malnutrition.[10]
Data were captured and analysed using Microsoft Office Excel and STATISTICA version 12 (StatSoft Inc., USA). Data are expressed using descriptive statistics. Contingency tables were used when comparing two nominal variables and independence was tested using the maximum-likelihood (M-L) χ2 test. Comparisons of data against reference values were done using 1-sample signed-rank non-parametric tests. A p-value of <0.05 was considered statistically significant. In cases where the data do not reflect the total study population, the relevant numbers are indicated in brackets.
Results
Demographic information
A total of 2 442 children, 2 481 CGs, and 270 HCWs participated in this survey (Fig. 1). The mean (standard deviation (SD)) age of children included in the study was 5.10 (6.24) months (range 6 weeks - 34.15 months), with nearly equal numbers of boys and girls (50.3%, n= 1 229 v. 49.7%, n= 1 213, respectively). Data collected from CGs indicated a mean (SD) age of 28.4 (8.2) years (range 13.8 - 73.0 years). Most CGs (92%; n=2 282/2 481) were the mother of the child and the primary CGs of one (42.5%; n=1 050/2 471) or two (31.8%; n=787/2 471) children. Eleven percent of CGs (n=281/2 481) had received no schooling or had not completed primary school; only 24.3% (n=604/2 481) had completed grade 12 (secondary school). Fourteen percent (n=365/2 481) of CGs had received further tertiary education.
Of the 270 recruited HCWs, 14.1% (n=38/269) were chief professional nurses, 42% (n=113/269) were professional nurses, and 16.2% (n=44/269) enrolled nurses. Most were female (97%, n=262/270), had achieved a tertiary qualification (69.3%; n=187/270) and had a median period of 5.0 years (range 0.5 - 37.0 years) of experience working in PHC.
Growth monitoring and promotion
Growth monitoring on the day of survey
With the exception of weight, anthropometric measurements were not performed routinely for the majority of children aged 0 - 36 months, indicating poor implementation of this section of the RtHB. Fig. 2 shows the concerning number of missed opportunities for appropriate growth monitoring on the day of survey.
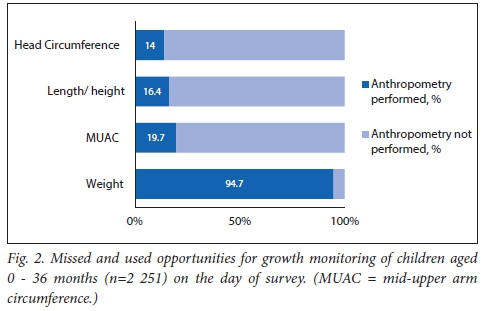
Correct procedures, as described in WC provincial government guidelines, were followed for weight measurements in 68.1% (n=1 534/2 251) of cases, followed by head circumference (56%; n=186/332), length/height (18.3%; n=71/338), and MUAC (10.2%; n=31/304).
In cases where the relevant anthropometry was performed, weight-for-age and length/height-for-age values were plotted on the RtHB growth charts in 90.3% (n=1 186/1 314) and 62.9% (n=178/283) of cases, respectively. However, plotting of weight-for-length/height was omitted in more than half (54.4%, n=149/274) of the observed cases. When measurements were plotted, most (>90%) were done correctly.
Prevalence of malnutrition
A total of 262 children (12%) were classified as underweight, which was most prevalent among children aged 0 - 6 months (13%, n=181/1 323). Owing to poor practices for length/height measurements, it was decided to omit results for stunting, wasting, overweight and obesity.
Table 1 shows the prevalence of acute malnutrition based on MUAC values for each of the age groups. It is clear that the younger children experienced the highest prevalence of malnutrition.
Anthropometric equipment available at PHC facilities
Forty-one PHC facilities (28.7%; n=41/143) did not have an infant length board available on site and in at least two facilities, length boards were being kept in storage. Fourteen facilities (9.8%; n=14/143) did not routinely measure standing height and measuring tapes were utilised in eleven facilities to measure length.
Facility equipment was found to be inaccurate with significant differences shown between standard 5 kg (p=0.000) and 10 kg (p=0.014) weights, as well as the mean value of the measurements displayed on facility scales. For the 2 kg weight, differences were not statistically significant (p=0.050).
HCW and CG knowledge, attitude, and practices regarding growth monitoring and promotion
Of those who completed this section, most HCWs were able to identify the correct frequency with which to perform various anthropometric measurements: weight measurements (81.3%; n=100/123), length/height (66.7%; n=82/123), MUAC (58.5%; n=72/123), and head circumference (28.8%; n=36/125) (Figure 3). Although the majority of HCWs could correctly identify the criteria for underweight (68.4%; n=178/260), far fewer could do so for stunting (54.6%; n=134/245) and wasting (38.7%; n=95/245).
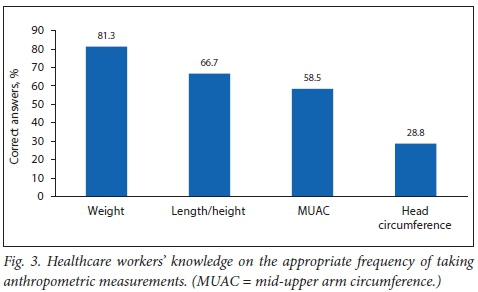
HCWs' ability to classify MUAC measurements was limited. Only half (50.2%; n=63/125) were able to correctly interpret a MUAC of <11.5 cm in children 6 months or older as severe acute malnutrition. Most HCWs (82.2%; n=212/258) were however able to identify the correct technique used to measure MUAC, and were aware of the correct rounding off procedures for length/height measurements (72.8%; n=91/125).
The majority of CGs 'strongly agreed' (79.2%; n=1 963/2 478) or 'agreed' (20.1%; n=499/2 478) that it was important for children to be weighed regularly. However, less than half of CGs reported that their child's growth was explained to them on the day of the survey (40.2%; n=530/1 320).
Immunisation
This section of the RtHB was deemed complete if a child had received all scheduled, age-appropriate immunizations and if all required documentation including date, batch number, and the HCW signature had been recorded in the booklet. The immunisation section of the RtHB was shown to be well implemented, with the records of 89.3% (n=2 171/2 431) of children up to date and fully completed. At the time of data collection, immunisations were due for 1 127 children, of which 92.5% (n=1 027/1 105) were administered. This indicates that few opportunities for immunisation were missed on the day of survey (7%; n=78/1 105).
HCWs were asked about their opinion on the changed immunisation schedule indicated in the RtHB by selecting one or more phrases which best represented their points of view. Only 39% (n=106) of HCWs chose to answer this question, of whom 79.8% indicated that 'It improves the overall health of children'. Although in the minority, responses such as 'a missed opportunity has no effect' and 'it is not culturally acceptable to all' are concerning and require further investigation.
Vitamin A supplementation
The vitamin A supplementation section of the RtHB was fully completed (date and signature indicated) for 94.6% (n=1 305/1 379) of children aged >6 months. On the day of survey, vitamin A supplementation was due for 346 children and was administered to 91.2% (n=301/330) of those.
Nearly all (98.8%) of the HCWs were able to identify the correct frequency with which to administer vitamin A supplementation. Age-appropriate dosages of vitamin A were also known by the majority of HCWs - more than 93% (n=209/223) answered correctly for all age categories. For both frequency (p=0.625) and dosages (p=0.439), no significant difference was found between those who had received formal training on the RtHB and those who had not.
In contrast to the encouraging level of HCW knowledge, only a small number of CGs (16.4%; 409/1 646) knew that a young child should receive vitamin A supplements every 6 months. However, significantly more CGs who reported to know the purpose of the RtHB (71.6%; n=293/409) knew the correct frequency with which vitamin A should be administered (p<0.01, χ2(1)=20) compared with 60% (n=1 244/2 072) who indicated that they knew the purpose of the RtHB but did not know the correct vitamin A frequency.
Deworming
Almost all HCWs (97.3%; n=262/269) knew the correct frequency with which to administer deworming treatment and no significant difference was found between those who had received formal training on the RtHB and those who had not. About two-thirds (67.6%, n=135/200) of children due for deworming on the day of survey received treatment. However, further examination of RtHBs revealed that for children aged >12 months, for whom data were available, this section was fully completed (dose, date and signature indicated) in only 48.8% (n=176/361) of all cases.
Only one in four CGs (26.2%; n=650/2 481) were aware that a child older than 1 year should receive deworming treatment every 6 months. However, significantly more CGs who reported to know the purpose of the RtHB (73.3%) knew the correct frequency of deworming treatment compared with those who did not know the purpose of the RtHB (57.9%) (p<0.01, χ2(1)=50.2).
HCW and CG knowledge, attitudes, and perceived barriers pertaining to the RtHB
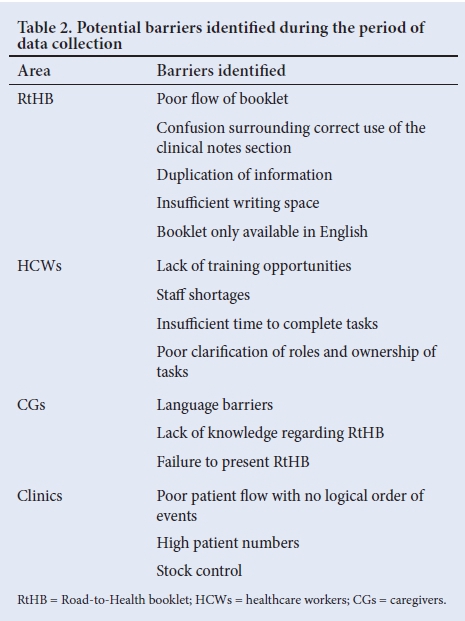
Three-quarters (75.2%; n=203/270) of the HCWs had received training on the implementation of the RtHB. Training consisted mainly of lectures of up to 2 hours long (32.8%; n=41/125), full-day workshops (23.2%; 29/125), and half-day workshops (14.5%; n=18/125). More than two-thirds (66.3%; n=176/265) of HCWs reported that the implementation of the RtHB had 'increased/significantly increased' their workload. However, two-thirds of HCWs (61%; n=164/269) indicated that they had sufficient time to complete the RtHB as part of their daily routine.
In addition to staff shortages and high patient numbers, insufficient stock supply was mentioned by some HCWs as a factor that hampered the effective implementation of the RtHB. Delayed delivery and no stock at the distributors or depots were mentioned as the main reasons for stock shortages. However, when asked the question 'Are there adequate stock levels of the following products available at your PHC clinic?' most HCWs indicated the 'always' response.
Two-thirds (61.9%; n=1 535/2 479) of the CGs indicated that they knew the purpose of the RtHB. Although 32% (n=796/2 479) of CGs indicated that all the information in the RtHB had been explained to them, 30.9% (n=767/2 479) indicated that no information had been explained to them. When asked whether they understood the content of the RtHB, 31.4% (n=774/2 464) CGs reported that they understood 'everything' and 23.4% (n=576/2 464) understood 'none'.
Table 2 provides potential barriers to successful RtHB implementation, as observed by investigators and perceived by CGs and HCWs during the course of the survey. These potential barriers, in summary, related to: logistical problems experienced by HCW with reference to the RtHB and clinic demographics, staff management issues affecting HCWs, as well as knowledge and understanding of the RtHB by CGs.
Discussion
Since its adoption in 2011, the RtHB has replaced the RtHC in the majority of cases in all districts of the WC. While certain sections of the booklet were utilised and documented well, data from this survey suggest that the implementation of most components of the RtHB require strengthening. Owing to the observational nature of the survey, the following commentary is confined to what was observed on the day of data collection and from a retrospective review of RtHBs.
Growth monitoring and promotion
Early identification and appropriate classification of malnutrition is pivotal to appropriate and timely intervention, especially in children <5 years of age. Regular weighing, with correct plotting of the weight and height and interpretation of the growth curve on the RtHB, form the core of the GMP strategy.[4]
With the exception of weight, anthropometric measurements (head circumference, height/length, MUAC) were not recorded routinely for the majority of children who were >6 months of age. The possible reasons why height/length measurements were not recorded routinely may include a lack of time, insufficient human resources, and the unavailability of equipment to measure length. Furthermore, although training was provided, HCWs may still not be clear on the purpose and importance of these measurements for determining a child's health. For many years HCWs have been using only the weight-for-age measurements according to the RtHC, and therefore may not have realised the relevance of performing a length/height measurement.
Parallel to the actions required from the HCWs, the CGs need to understand that GMP may contribute to the prevention of child malnutrition, provided good quality measurements are performed.[6,11]This current survey found that less than half of CGs had their child's growth explained to them. Previous studies also found that mothers were not provided with feedback on the growth assessment of their children, identifying missed opportunities in healthcare education.[11-14]
In SA, time constraints and short staffing limit HCWs' ability to fully comprehend guidelines, allocate adequate time to patients and provide the necessary nutrition counselling.[15]
As key role-players in monitoring the development of children, the HCWs need to be familiar with growth monitoring charts and be able to perform measurements and interpret the results accurately. Similar to other studies which indicated poor knowledge in terms of identification of malnutrition, most HCWs in the current survey were able to identify the correct frequency with which to perform weight measurements; however, fewer were able to do so for length/ height, MUAC and head circumference. A study conducted by Cloete et al.[l6] in the Metropole region, WC, SA, found that only 52% and 38% of HCWs could correctly interpret the criteria for underweight and wasting, respectively. A study conducted in Limpopo Province, SA, found that only 40.6% of nurses could correctly identify stunting, 47.9% could identify underweight and only 11.5% could identify wasting.[6] Inaccurate plotting and interpretation of measurements were also reported in other studies.[6,15,17]
Another factor hampering optimal implementation of growth monitoring were the inaccuracies noted in the current survey in facilities' growth monitoring equipment. The chance that malnutrition may be properly managed is therefore slim, as children's measurements may be incorrectly classified - this will hinder appropriate diagnosis, referral and follow-up treatment. The lack of appropriate height/length measurement resources found in this survey needs to be addressed, as almost a third of PHC facilities did not have the equipment available, which could lead to the use of inaccurate measuring tools, such as measuring tapes. This lack of growth monitoring equipment corresponds with the results reported in a diagnostic and implementation evaluation of nutrition programmes in SA.[15] Regular motivation from district PHC managers to reinforce this practice as well as regular monitoring could contribute to improved implementation in the long term. In addition, anthropometric apparatuses must be available and accurately calibrated for effective growth monitoring to occur.
Immunisation
As immunisation is regarded as a cost-effective intervention for reducing child morbidity and mortality,[18,19] the global Expanded Programme on Immunisation (EPI), launched by the WHO in 1974,[18] was introduced in SA (EPI-SA) in 1995. The current EPI-SA schedule has adopted a primary series of 6, 10 and 14 weeks, ensuring protection at the earliest age, with boosters where applicable, and an early measles vaccine at 9 months. The EPI-SA aims to offer daily immunisation services (provided free of charge at all PHC facilities in SA) in order to improve coverage, and reduce vaccine-preventable diseases and childhood mortality.
Despite these developments, the EPI programme in SA is facing a number of challenges, including low vaccination coverage in some areas and poor knowledge of the community of the immunisation programme and purpose.[20] Barriers to the successful implementation of the programme include insufficient knowledge of the EPI programme and immunisations in general by HCWs, as well as financial constraints that affect stock levels,[13,20] and insufficient staff numbers.[13] In the current survey, a promising 9 out of 10 children aged 0 - 36 months had received age-appropriate vaccines.
Vitamin A supplementation
The National DoH recommends that all children should be screened at every visit to ensure that vitamin A supplementation is up to date.[21] The results of the current survey are promising in that the vitamin A section of the RtHB was fully completed for the majority of children aged >6 months. Vitamin A supplementation was administered in 91% of due cases, which corresponds with results from previous studies.[15,23] Similar findings were reported in two different studies at PHC clinics in the WC, in that about a third (25% and 34%, respectively) of children received vitamin A supplementation when it was due and recording of the supplementation in the RtHC was made in 97% and 77% of cases, respectively.[14,22]
A study of registered professional nurses in Limpopo Province, SA, indicated that more than half of participants (52.1%) knew the correct frequency of administering vitamin A supplementation and deworming medication.[6] Although nearly all of the HCWs in the current survey were able to identify the correct frequency with which to administer vitamin A supplementation, this knowledge was not transferred as only a small number of CGs knew that a young child should receive vitamin A supplementation every 6 months. It appears that knowledge had a positive effect as significantly more CGs who reported to know the purpose of the RtHB, knew the correct frequency with which vitamin A should be administered. Literature reports that relatively few CGs knew why their children should receive vitamin A supplementation, ranging from 24% to 39%.[14,22]
If mothers and CGs had a better understanding of the benefits of routine nutrition interventions, they would be more likely to seek these services. This could result in CGs insisting on better service and a reduction in the number of missed opportunities.[22] Furthermore, in SA, results from diagnostic and implementation evaluation of nutrition programmes targeting children <5 years of age found that, given the workloads at most PHC facilities, interventions that involve education or counselling are not as readily provided as interventions that are 'commodity-based' such as medicines, or immunisations.[15]
Deworming
Children between 1 and 5 years of age are targeted for regular deworming as they are most burdened with soil-transmitted helminth infections and bilharzia. These infections adversely affect the growth, ability to learn and intellectual development of children.'41 Results from the current survey showed that approximately two-thirds of children due for deworming on the day of the survey received treatment. However, the completion of this section in the RtHB was poor in ~50% of the cases.
A survey that assessed people's knowledge, as well as attitudes and practices of intermittent deworming in Nigeria, found that only 44.8% of children <5 years of age were dewormed at 3-month intervals. These findings show a need for active health promotion programmes to enhance compliance to intermittent deworming.[23] Results from the current survey showed that only a quarter of the CGs were aware that a child older than 1 year should receive deworming treatment every 6 months. A study on missed opportunities at healthcare facilities in the City of Cape Town showed failure to dispense important disease prevention drugs such as vitamin A and deworming tablets. These missed opportunities contribute to the high incidence of child mortality and morbidity.[13]
Staff knowledge
This survey demonstrated clear gaps in HCWs' knowledge relating to various components of the RtHB. Concerns over gaps in HCWs' knowledge were further reinforced by a recent national evaluation report on nutrition interventions for children.[15] The report identified a lack of sufficient knowledge and skills among staff responsible for rendering nutritional interventions such as growth monitoring, nutrition education and counselling. Staff shortages and insufficient nutrition training were found to contribute to ineffective implementation across all departments.[15]
Conclusion and recommendations
Various barriers can influence the implementation of nutrition interventions at the PHC level, e.g. poor staff knowledge and skills, lack of time, staff shortages, and/or frequent staff changes of trained staff owing to attrition or rotation. Our survey revealed that the growth monitoring section of the RtHB requires improvement from a knowledge and implementation perspective. The survey also revealed a lack of appropriate height/length measurement resources. Administration of immunisations and vitamin A was performed adequately; however, knowledge of CGs on the frequency of deworming and vitamin A supplementation needs attention.
Regular training and refresher training needs to be presented to all HCWs, especially related to the new growth indicators in the RtHB. Emphasis should be placed on the importance of performing the height/ length, MUAC and head circumference measurements regularly and accurately. Regular reinforcing of this practice by PHC facility managers, the provision of appropriate apparatuses and resources to perform the required anthropometric measurements, regular monitoring of HCWs' practices, as well as dedicated efforts from all HCWs to optimally implement the RtHB are deemed essential to improve the implementation of this tool. If implementation is not adequately achieved, children will not be appropriately identified, classified and treated. Furthermore, community health workers can be more actively involved to assist the HCWs to create awareness of these preventive services and the importance of the RtHB as a monitoring tool in the broader community.
To be consistent with international guidelines and national policy, sufficient focus, effort and resources should be channelled towards early identification of nutritionally at-risk children. Continuous training of HCWs, evaluation, and monitoring of each intervention will be necessary to achieve successful implementation of the RtHB and securing integrated healthcare for all infants and young children. This will require a shift away from task-oriented behaviour to preventive and promotive practices by HCWs.
Acknowledgements. We would like to convey our sincere thanks to the Western Cape Department of Health, specifically the Sub-Directorate Nutrition, for granting permission to conduct the survey. In addition, we would like to convey our sincere gratitude to all the caregivers, infants and HCWs at each facility who participated in our survey. Lastly, we would like to thank all the members of the RtHB survey research group (mentioned below) as well as the administrative staff members of the Division of Human Nutrition and Prof. D Nel from the Centre for Statistical Consultation, Stellenbosch University, for his help with statistical analyses.
Author contributions. Study conception and design: RB, LD, LdP, HEK, NK, MLM, EvN, JV. Data collection: RB, LD, LdP, HEK, MLM, EvN, JV. Data analysis and interpretation: RB, LD, LdP, HEK, NK, EvN, JV. Conceptualising and writing the manuscript: RB, LD, LdP, HEK, NK, MLM, EvN, JV.
Funding. RB: Stellenbosch University (Fund for Innovation in Rural Research, Harry Crossley Foundation) and Western Cape Department of Health. No funder had any role in the design, analysis or writing of this article.
Conflicts interest. None.
Road-to-Health Survey Research Group. Bam N, Blaauw R, Boshoff H, Clarke P, Coetzee C, Daniels L, de Kock I, de Vos I, de Vries K, du Buisson L, du Plessis LM, du Preez U, Ehlers A, Engelbrecht C, Evans N, Ferreira N, Findlay A, Foot J, Fordjour V, Frey C, Groenewald L, Hallinan T, Hartman D, Jackson G, J van Rensburg S, Jooste M, Kamhoot A, Kapena C, Kelly T, Kerbelker R, Koen N, Koornhof HEK, Kotlowitz J, le Grange M, le Roux M, Lee T, Liebenberg S, Louw A, Louw S, Marais ML, Maritz A, Martens A, Meyer I, Mncwabe N, Moens M, Morris N, Naude K, Nel M, Nel S, Nkomani S, Nyenes R, Olivier L, Pienaar T, Pilditch
K, Potgieter S, Richardson C, Rickard L, Robinson R, Röhrs S, Samuels S-L, Simjee Z, Slazus C, Smit L, Smit Y, Stander L, Stone P, Strydom E, Strydom K, Swanich L, Swartz P, Swart D, Taverner T, Taylor A, Teuchert N, Turner L, Uys M, van de Venter A, van der Merwe L, van der Schyff S, van Niekerk E, van Rhyn N, van Wyk N, van Zyl F, Venter B, Verster B, Verster J, Visser J, Visser ME, Wasserfall L, Wakelin M, Webber S, Wicomb R, Yeh E.
References
1. Black RE, Victora CG, Walker SP, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013;382(9890):427-451. https: 10.1016/S0140-6736(13)60937-X. [ Links ]
2. Webb P. Nutrition and the Post-2015 Sustainable Development Goals. A Technical Note. Geneva: WHO, 2014. United Nations System Standing Committee on Nutrition. https://www.unscn.org/files/Publications/Briefs_on_Nutrition/Final_Nutrition%20and_the_SDGs.pdf (accessed 2 December 2016). [ Links ]
3. Ashworth A, Shrimpton R, Jamil K. Growth monitoring and promotion: Review of evidence of impact. Matern Child Nutr 2008;4(Suppl 1):86-117. https://doi.org/10.1111/j.1740-8709.2007.00125.x. [ Links ]
4. National Department of Health. Strategic Plan for Maternal, Neonatal, Child and Women's Health (MNCWH) and Nutrition in South Africa 2012 - 2016. Pretoria: NDoH, 2011. https://extranet.who.int/nutrition/gina/sites/default/ files/ZAF%202012%20MNCWHstratplan.pdf (accessed 6 December 2017). [ Links ]
5. Tarwa C, de Villiers FPR. The use of the Road to Health Card in monitoring child health. SA Fam Pract 2007;49(1):15-15d. https://doi.org/10.1080/20786204.2007.10873497 [ Links ]
6. Kitenge G, Govender I. Nurses' monitoring of the Road to Health Chart at primary healthcare level in Makhado, Limpopo province. S Afr Fam Pract 2013;55(3):275-280. https://doi.org/10.1080/20786204.2013.10874350 [ Links ]
7. Department of Health. Western Cape Road to Health Booklet Training Package CD; 2010. [ Links ]
8. De Onis M, Onyango A, Borghi E, Siyam A, Pinol A. WHO Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age. Methods and development. Geneva: WHO, 2016. http://www.who.int/childgrowth/standards/Technical_report.pdf (accessed March 2016). [ Links ]
9. WHO Expert Committee. Physical Status: The Use and Interpretation of Anthropometry. Geneva: WHO, 1995. http://www.who.int/childgrowth/publications/physical_status/en/index.html (accessed March 2016). [ Links ]
10. United Nation System. Standing Committee on Nutrition: Task Force on Assessment, Monitoring, and Evaluation. Fact sheets on Food and Nutrition Security Indicators/Measures: Mid-Upper Arm Circumference (MUAC) http:// www.unscn.org/files/Task_Forces/Assessment_Monitoring_and_Evaluation/MUAC.pdf (accessed March 2016). [ Links ]
11. Coulibaly F. Mothers perception of quality of growth monitoring and promotion programs: A qualitative study in Cote d'Ivoire. Ecol Food Nutr 2002;41(6):475-500. [ Links ]
12. Thandrayen K, Saloojee H. Quality of care offered to children attending primary health care clinics in Johannesburg. SA J Child Health 2010;4(3):73-77. [ Links ]
13. Jonker L, Stellenberg EL. Missed opportunities in child healthcare. Afr J Prim Health Care Fam Med 2014;6(1):1-7. https://doi.org/10.4102/phcfm.v6i1.537. [ Links ]
14. Du Plessis LM, Najaar B, Koornhof HE, et al. Evaluation of the implementation of the vitamin A supplementation programme in the Boland/Overberg region of the Western Cape Province. S Afr J Clin Nutr 2007;20(4):126-132. [ Links ]
15. Department of Performance Monitoring and Evaluation. Evaluation of Nutrition Interventions for Children from Conception to Age 5. Department of Health, Department of Social Development & Department of Performance Monitoring and Evaluation. The Presidency, Republic of South Africa, South Africa, Pretoria. 2014. http://www.nutritionsociety.co.za/attachments/article/76/Summary-Evaluation-of-Nutritional-Interventions-for-Children-from-Conception-to-Age-5-.pdf (accessed March 2016) [ Links ]
16. Cloete I, Daniels L, Jordaan J, Derbyshire C, Volmink L, Schubl C. Knowledge and perceptions of nursing staff on the new Road to Health Booklet growth charts in primary healthcare clinics in the Tygerberg subdistrict of the Cape Town metropole district. S Afr J Clin Nutr 2013;26(3):141-146. https://doi.org/10.1080/16070658.2013.11734458 [ Links ]
17. Schoeman SE, Hendricks MK, Hattingh SP, Benadé AJS, Laubscher JA, Dhansay MA. The targeting of nutritionally at-risk children attending a primary health care facility in the Western Cape Province of South Africa. Publ Health Nutr 2006;9(8),1007-1012. https://doi.org/ 10.1017/PHN2006986 [ Links ]
18. Machingaidze S, Wiysonge CS, Hussey GD. Strengthening the Expanded Programme on Immunization in Africa: Looking beyond 2015. PLoS Med 2013;10:e1001405 https://doi.org/10.1371/journal.pmed.1001405 [ Links ]
19. Ndirangu J, Bärnighausen T, Tanser F, Tint K, Newell ML. Levels of childhood vaccination coverage and the impact of maternal HIV status on child vaccination status in rural KwaZulu-Natal, South Africa. Trop Med Int Health 2009;14(11):1383-1393. https://doi.org/10.1111/j.1365-3156.2009.02382.x [ Links ]
20. Wiysonge CS, Ngcobo NJ, Jeena PM, et al. Advances in childhood immunisation in South Africa: Where to now? Programme managers' views and evidence from systematic reviews. BMC Public Health 2012;12(1):578. https://doi.org/10.1186/1471-2458-12-578 [ Links ]
21. National Department of Health (NDoH). National vitamin A supplementation policy guidelines for South Africa. Pretoria: NDoH, 2012. http://www.adsa.org.za/Portals/14/Documents/DOH/Vit%20A%20policy%20guidelines%20OF%20S%20A%20-%20recent_1.pdf (accessed March 2016). [ Links ]
22. Hendricks M, Beardsley J, Bourne L, Mzamo B, Golden B. Are opportunities for vitamin A supplementation being utilised at primary health-care clinics in the Western Cape Province of South Africa? Publ Health Nutr 2007;10(10):1082-1088. https://doi.org/10.1017/S1368980007699522 [ Links ]
23. Stanley CN, Oreh NC, Johnson-Ajinwo RO. Knowledge, attitudes and practices of intermittent deworming in Alakahia community, Rivers State, Nigeria. Int Res J Med Sci 2013;1(7):1-7. [ Links ]
 Correspondence:
Correspondence:
R Blaauw
rb@sun.ac.za
Accepted 12 September 2017














