Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Child Health
versão On-line ISSN 1999-7671
versão impressa ISSN 1994-3032
S. Afr. j. child health vol.10 no.4 Pretoria Dez. 2016
http://dx.doi.org/10.7196/sajch.2016.v10i4.1189
CASE REPORT
Intracardiac and intracerebral thrombosis associated with methylenetetrahydrofolate reductase A1298C homozygote mutation in paediatric steroid-resistant nephrotic syndrome
R RendaI; Ö AydoğII; M BülbülII; E K ÇakıcıII
IMD; Pediatric Nephrology Department, Antalya Education and Research Hospital, Antalya, Turkey
IIMD; Pediatric Nephrology Department, Dr Sami Ulus Maternity and Children's Research and Education Hospital, Ankara, Turkey
ABSTRACT
Thromboembolic complications are a significant cause of morbidity and mortality in cases of nephrotic syndrome. Hereditary thrombophilias are also known to increase vascular thrombosis. We present a case that has been followed up for steroid-resistant nephrotic syndrome (NS) in which intracardiac and intracranial thrombosis subsequently developed. The patient was found to have a homozygote mutation in the methylenetetrahydrofolate reductase (MTHFR) gene as an additional risk factor for recurrent thrombosis. MTHFR mutation with NS was considered to have an important effect on the development of life-threatening thrombosis.
Although thromboembolic events in nephrotic syndrome (NS) are seen less often in children (2 - 5%) than in adults (20 - 30%), these are life-threatening complications.[1] An increase in clotting factors, a decrease in anticoagulant proteins, thrombocytosis and thrombocyte hyperaggregation, abnormal fibrinolysis, an increase in plasma lipids, corticosteroid and diuretic treatment and immobilisation all cause an increased tendency to thrombosis in NS.[2] Although venous thrombosis is more commonly observed, arterial thrombosis may also develop. Despite the rare occurrence of renal vein, sagittal sinus and intracardiac thrombosis, and pulmonary embolism, they are seriously life-threatening when they develop.[3] Early diagnosis, appropriate fibrinolytic treatment and long-term use of protective anticoagulants are extremely important.[4]
Using folic acid as a cofactor, methylenetetrahydrofolate reductase (MTHFR) enzyme converts homocysteine to methionine. In the absence or impairment of this enzyme, hyperhomocysteinaemia occurs, causing atherosclerosis and vascular thrombosis. Mutations most often seen in the MTHFR gene, in particular C677T and A1298C missense mutations, have been found to have a relationship with cerebrovascular diseases.[5]
In the case presented here the patient was diagnosed as having steroid-resistant NS (SRNS) at the age of 2 years. During the follow-up period he first developed intracardiac thrombosis and 5 years later intracranial thrombosis appeared. The patient was determined to have MTHFR A1298C homozygote mutation as an additional risk factor for recurrent thrombosis in NS.
Case report
The patient had previously experienced two NS attacks that responded to steroids, then, as no response was obtained with 8 weeks of steroid treatment in the 3rd attack, he was referred to Dr Sami Ulus Maternity and Children's Research and Education Hospital. There was no consanguinity or familial nephropathy history. The physical examination determined a body temperature of 39°C, tachypnoea, subcostal retraction, crepitant rales on auscultation of the lungs and anasarca-type oedema. The laboratory findings showed leukocytosis, thrombocytosis (831 000/mm3), hypoalbuminemia (13 g/L), massive proteinuria and hyperlipidaemia (cholesterol 280 mg/dL, triglyceride 196 mg/dL). The kidney and liver function tests, and C3 and C4, were normal. Antinuclear antibody, anti-dsDNA, hepatitis serology and Purified Protein Derivative Test were found to be negative. On the abdominal ultrasound there was massive acites. On the pulmonary radiograph the bilateral costophrenic angles were obscured and there was bilateral paracardiac infiltration.
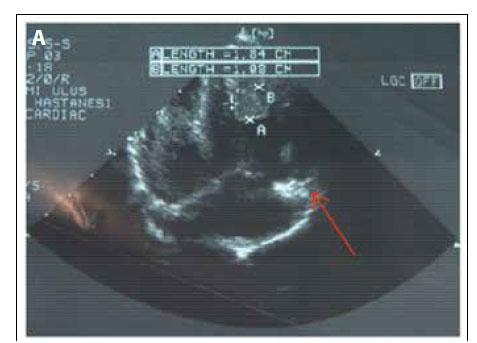
With a diagnosis of pulmonary infection and thrombocytosis, the patient was started on antibiotic therapy and acetylsalicylic acid as antiplatelet treatment. The level of infection reduced within 1 week. However, after 2 weeks, there was a sudden development of tachycardia, tachypnoea, gallop rhythm, 2/6 systolic murmur on the left of the sternum and hepatomegaly. Echocardiograph showed mitral and tricuspid insufficiency and thrombus, located below the anterior wall and tricuspid valve, extending to the apex within the right ventricle (Fig. 1A). Of the coagulation parameters, while prothrombin and partial thromboplastin times, protein S and factors 2, 5, 8, 9, 10 and 11, were determined as normal, antithrombin III (15.8%; normal 75 - 125%) and protein C (62%; normal 70 - 140%) were found to be low. Anticardiolipin and antiphospholipid antibodies and factor 5 Leiden and prothrombin 20210A gene mutations were found to be negative. MTHFR gene mutations could not be assayed at our hospital at that time.
The patient was started on a treatment of low-molecular-weight heparin as an anticoagulant and oral prednisolone 60 mg/m2/day. Antiplatelet treatment was continued. After 2 weeks the thrombus had started to diminish and complete remission in NS was obtained. The patient was discharged with prednisolone in tapering doses and anticoagulant and antiplatelet treatments, and 2 months later, the thrombus had disappeared completely on echocardiograph (Fig. 1b). Antithrombin III and protein C levels returned to normal; therefore, anticoagulant treatment could be stopped.
In the follow-up of the patient, because of the development of secondary steroid resistance, a renal biopsy was obtained. Focal segmental glomerulosclerosis was determined and cyclosporine was added to the treatment. Complete remission was achieved with cyclosporine and low-dose prednisolone (0.25 mg/kg/day) for 2 years and immunosuppressive treatment was stopped 2 years later. In the 5th year of follow-up, owing to an increase in gastrointestinal complaints and with measurable thrombophilic gene mutations being negative, antiplatelet treatment was also terminated.
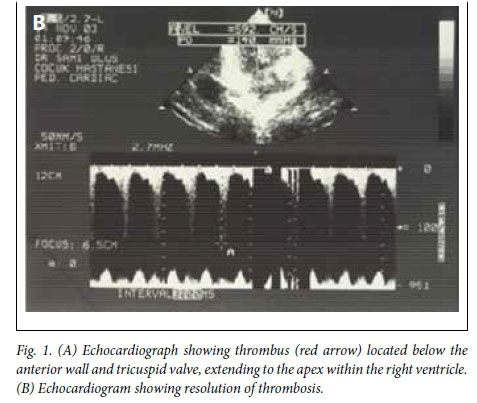
In the 6th year of follow-up, the patient again presented with frequently relapsing NS. Intravenous pulse methylprednisolone (30 mg/kg/day, max. 1 g/day; 3 days) was administered and mycophenolate-mofetil treatment was begun. After 20 days the patient developed severe headache, vomiting and loss of sight in his left eye, and bilateral papillary oedema was observed. Cranial diffusion magnetic resonance (MR) and MR angiography showed brain oedema, the slowing of the blood flow in the left sagittal-transverse sinus and left jugular vein, as well as intravascular thrombus (Fig. 2). Coagulation parameters (factor 2, 5, 8, 9, 10, 11, protein C and S, antithrombin III, active protein C resistance and homocysteine levels (2.38 mmol/L and 12 mmol/L, N 4 - 15)) were found to be normal. Anticardiolipin and antiphospholipid antibodies were also negative. From the MTHFR gene mutations examined, while no mutation was found in C677T, homozygote mutation in A1298C was determined.

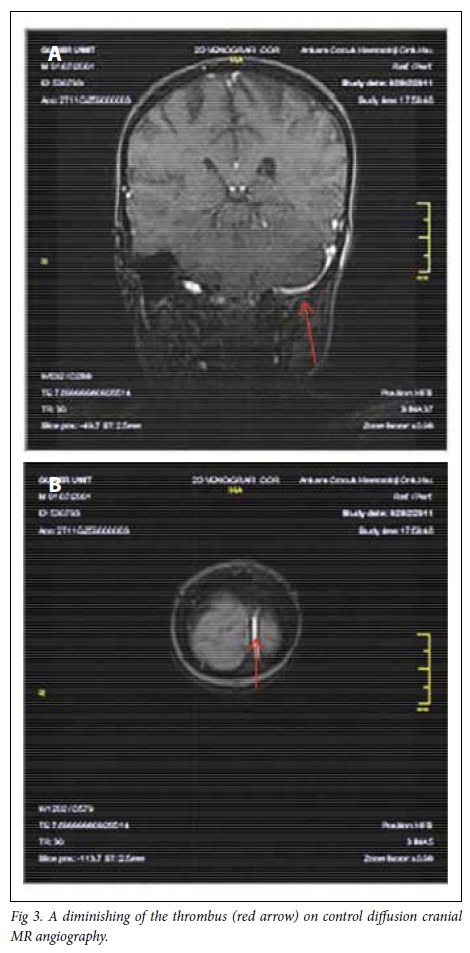
A diminishing of the thrombus was achieved with low-molecular-weight heparin (Fig. 3), and the patient's headache diminished and his sight also recovered.
The patient was discharged with low-dose oral steroid, myco-phenolate mofetil, low-molecular-weight heparin prophylaxis and antiplatelet treatment. Prophylactic anticoagulant therapy was discontinued after 6 months. The patient is still being followed-up by the paediatric nephrology and haematology departments. During the last 4-year follow-up period, with only antiplatelet treatment, no recurrence of thrombus has been observed in spite of a few relapse NS attacks.
Discussion
SRNS patients are at a higher risk of developing thromboembolic complications compared with steroid-sensitive NS patients.[6] Recurrent thrombotic events are seen more often in NS patients if there are additional risk factors for hypercoagulability such as infection, dehydration or hereditary thrombophilic conditions (congenital deficiencies of anticoagulant proteins such as ATIII, protein C and S, or thrombophilic gene mutations such as FV Leiden mutation, prothrombin 20210A mutation, MTHFR mutations or platelet glycoprotein polymorphisms).[7] The potential risk factors for thrombosis in our case were thrombocytosis, hypoalbuminemia, hyperlipidemia and long-term steroid use owing to NS as well as the presence of MTHFR A1298C homozygote mutation.
The MTHFR gene is located on chromosome 1p36.3 locus. Aided by folic acid and vitamin B12, homocysteine is transformed to methionine by remethylation.[5] Hyperhomocysteinemia, forming as a result of a molecular defect in this gene, leads to vascular endothelial damage, venous thrombosis, atherosclerosis, stroke, coronary artery disease, neural tube defects and migraine, owing to vasodilatator nitric oxide deficiency and superoxide formation. [8] Weisberg et al.[9] found that the MTHFR gene mutation has the effect of reducing enzyme activity rather than causing low enzyme levels or hyperhomocysteinemia. Our patient's homocysteine levels were found to be normal, which is consistent with his findings.
In particular, MTHFR A1298C homozygote mutation has been shown to lead to cerebrovascular thrombosis and stroke in children. [7,10] Compound MTHFR heterozygosity (677C→T and 1298A→C) has also been reported to be a risk factor for thrombosis.[11]
Although SRNS patients are at a higher risk of developing thromboembolic complications, sagittal sinus and intracardiac thrombosis are rarely observed. A large intracardiac thrombus in a child with SRNS was previously reported in the Turkish literature.® Divekar et al.[12] found only one case with cerebral sinus thrombosis among 700 children with NS. Clinical presentation of cerebral sinus thrombosis is variable, from headaches and vomiting to seizures, vision loss, hemiparesis and coma.[13]
Although prophylactic treatment of thrombosis in NS is uncertain, some authors suggest anticoagulant treatment in patients with low albumin levels and antiplatelet drugs in patients with severe thrombocytosis.[14]
There are also limited unproven data concerning the treatment of thromboembolic complications in children with NS. Low-molecular-weight heparin is preferred in paediatric patients and the recommended treatment duration is usually between 3 and 6 months. In the literature different anticoagulants have been used in NS patients with intracardiac or intracerebral thrombosis, ensuring full recovery. It is suggested that the positive outcome in these patients is based on the early diagnosis of thrombosis and administration of anticoagulation therapy along with control of NS.[3,13-16]
Conclusion
In our case, the MTHFR mutation, in addition to NS, was considered to have an important effect on the development of cerebral and intracardiac thromboses. Complete recovery of the thrombosis was achieved with early anticoagulant therapy and folic acid support. The patient is still being followed-up by the paediatric nephrology and haematology departments. During the last 4-year follow-up period, with only antiplatelet treatment, no recurrence of thrombus has been observed in spite of occasional relapse NS attacks.
References
1. Lilova MI, Velkovski IG, Topalov IB. Thromboembolic complications in children with nephrotic syndrome in Bulgaria (1974-1996). Pediatr Nephrol 2000;15(1-2):74-78. http://dx.doi.org/10.1007/s004679900253 [ Links ]
2. Niaudet P, Boyer O. Idiopathic nephrotic syndrome in children: Clinical aspects. In: Ellis DA, Harmon WE, Niaudet P, Yoshikawa N, eds. Pediatric Nephrology (6th ed.). Berlin: Springer-Verlag, 2009:667-703. [ Links ]
3. Ekici F, Çakar N. A large intracardiac thrombus in a child with steroid-resistant nephrotic syndrome. Cardiol Young 2013;23(3):440-442. http://dx.doi.org/10.1017/S1047951112000923 [ Links ]
4. Lin CC, Lui CC, Tain YL. Thalamic stroke secondary to straight sinus thrombosis in a nephrotic child. Pediatr Nephrol 2002;17(3):184-186. [ Links ]
5. Fodinger M, Horl WH, Sunder-Plassmann G. Molecular biology of 5,10-methylenetetrahydrofolate reductase. J Nephrol 2000;13(1):20-33. [ Links ]
6. Hoyer PF, Gonda S, Barthels M, Krohn HP, Brodehl J. Thromboembolic complications in children with nephrotic syndrome. Risk and incidence. Acta Paediatr Scand 1986;75(5):804-810. [ Links ]
7. Suri D, Ahluwalia J, Saxena AK, et al. Thromboembolic complications in childhood nephrotic syndrome: A clinical profile. Clin Exp Nephrol 2014;18(5):803-813. http://dx.doi.org/10.1007/s10157-013-0917-2 [ Links ]
8. Boers GH. Hyperhomocysteinemia as a risk factor for arterial and venous disease. A review of evidence and relevance. Thromb Haemost 1997;78(1):520-522. [ Links ]
9. Weisberg I, Tran P, Christensen B, Sibani S, Rozen R. A second genetic polymorphism in methylenetetrahydrofolate reductase (MTHFR) associated with decreased enzyme activity. Mol Genet Metab 1998;64(3):169-172. http://dx.doi.org/10.1006/mgme.1998.2714 [ Links ]
10. Rook JL, Nugent DJ, Young G. Pediatric stroke and methylenetetrahydrofolate reductase polymorphisms: An examination of C677T and A1298C mutations. J Pediatr Hematol Oncol 2005;27(11):590-593. http://dx.doi.org/10.1097/01.mph.0000188119.33452.fd [ Links ]
11. Simsek E, Yesilyurt A, Pinarli F, Eyerci N, Ulus A. Combined genetic mutations have remarkable effect on deep venous thrombosis and/or pulmonary embolism occurrence. Gene 2014:536(1):171-176. http://dx.doi.org/10.1016/j.gene.2013.11.019 [ Links ]
12. Divekar AA, Ali US, Ronghe MD, Singh AR, Dalvi RB. Superior sagittal sinus thrombosis in a child with nephrotic syndrome. Pediatr Nephrol 1996;10(2):206-267. http://dx.doi.org/10.1007/bf00862081 [ Links ]
13. Palcoux JB, Gaspard F, Campagne D. Cerebral sinus thrombosis in a child with steroid-resistant nephrotic syndrome. Pediatr Nephrol 2003;18(6):610-611. http://dx.doi.org/10.1007/s00467-003-1100-x [ Links ]
14. Papachristou FT, Petridou SH, Printza NG, Zafeiriou DI, Gompakis NP. Superior sagittal sinus thrombosis in steroid-resistant nephrotic syndrome. Pediatr Neurol 2005;32(4):282-284. http://dx.doi.org/10.1016/j.pediatrneurol.2004.11.004 [ Links ]
15. Skalova S, Lukes A, Vanicek H, et al. Intracardiac thrombus - a rare complication of the steroid resistant nephrotic syndrome. Bratisl Lek Listy 2008;109(12):573-575. [ Links ]
16. Ueno K, Nagasako H, Ueno M, et al. Large intracardiac thrombus in a child with refractory nephrotic syndrome. Pediatr Int 2010;52(1):e51-e53. http://dx.doi.org/10.1111/j.1442-200X.2009.02991.x [ Links ]
 Correspondence:
Correspondence:
R Renda
rahimeg@yahoo.com
Accepted 29 August 2016