Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Child Health
versión On-line ISSN 1999-7671
versión impresa ISSN 1994-3032
S. Afr. j. child health vol.10 no.4 Pretoria dic. 2016
http://dx.doi.org/10.7196/sajch.2016.v10i4.1096
RESEARCH
Outcome of very-low-birth-weight babies managed with nasal continuous positive airway pressure, with or without surfactant, in a high-care nursery
T Bopape-ChinyangaI; R ThomasII; S VelaphiIII
IMB ChB; Department of Paediatrics, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIMB ChB, FC Paed; Department of Paediatrics, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIIMB ChB, FC Paed, MMed; Department of Paediatrics, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
BACKGROUND. Very-low-birth-weight (VLBW) infants who require nasal continuous positive airway pressure (NCPAP) are managed in neonatal intensive care units (NICUs) in developed countries, while in low-resource settings this is not always possible. The failure rate of NCPAP provided outside NICUs is not well known.
OBJECTIVES. To determine the failure rate, assessed as the need for invasive medical ventilation (iMV) and mortality on NCPAP in VLBW infants managed in a high-care nursery (HCN) within the first 72 hours of life.
METHODS. Records of VLBW infants managed with NCPAP, at Chris Hani Baragwanath Hospital, were reviewed for infant characteristics, need for iMV and mortality on NCPAP. Clinical risk index for babies (CRIB) was calculated for each infant. Comparisons were made between those who needed iMV and those who did not, and between survivors and non-survivors on NCPAP.
RESULTS. A total of 325 VLBW infants were managed with NCPAP in the HCN. Mean (standard deviation) birth weight was 1 120 (184)g, 98.5% were of gestational age (GA) <34 weeks and 14.9% were small for GA (SGA). Thirteen percent died while on NCPAP and 33% of survivors required iMV - an overall failure rate of 43%. Factors associated with iMV were high CRIB score (p<0.001), lower Apgar score (p=0.013), lower PaO2 (p=0.022) and high base deficit (p=0.034). Those who died were more likely to have extremely low birth weight (p<0.001), lower GA (p<0.001), high CRIB score (p<0.001) and base deficit (p<0.001). On multivariate analysis, the predictors for need of iMV were low Apgar score (p=0.033), SGA (p=0.042) and CRIB score (p=0.005), while that of mortality on NCPAP was birth weight.
CONCLUSION. Although failure rate of NCPAP in VLBW infants managed in HCN is high, a significant proportion of VLBW infants benefit from this intervention.
Respiratory distress is a common clinical presentation in newborn infants shortly after birth. Respiratory distress in preterm infants or very-low-birth-weight (VLBW) infants is often due to respiratory distress syndrome (RDS), resulting from insufficient production of surfactant leading to atelectasis. It can also result from chest wall weakness and immature alveoli. One of the management strategies for respiratory distress in VLBW infants is non-invasive mechanical ventilation (MV) using continuous positive airway pressure (CPAP). CPAP was first used as a method of supporting the breathing of preterm infants in 1971.[1] It is considered to be one of the interventions that has contributed significantly to the reduction of neonatal mortality globally.[2] The physiological effects of CPAP include increasing functional residual capacity, hence improving oxygenation and maintaining lung volume, reducing work of breathing, conserving surfactant and reducing obstructive apnoea. Nasal CPAP (NCPAP) is the commonly used form of administering CPAP.[3] Nasal prongs are used as they offer less resistance than an endotracheal tube. NCPAP is widely used for a range of neonatal respiratory conditions and is considered the first-line intervention in the management of preterm or VLBW infants with RDS.[4] In developed countries this intervention is applied in the neonatal intensive care unit (NICU), but in developing or low-resource settings this is not always possible.
The proportion of preterm infants at gestation of 25 - 28 weeks who are managed successfully with NCPAP soon after birth ranges from 45 to 68%, and the proportion of those at gestation 29 - 32 weeks has been reported to be 64 - 76%.[5-7] The use of NCPAP in preterm infants with respiratory distress is associated with lower risk for death or use of assisted ventilation.[8] A number of studies in preterm infants reported that the use of NCPAP soon after birth with or without prior administration of exogenous surfactant was associated with similar or better outcomes than invasive MV (iMV).[9] Although a large number of patients managed with NCPAP do well, a significant proportion of infants managed on NCPAP fail and go on to be intubated for MV. The proportion of preterm or VLBW infants who are initially managed with NCPAP only and subsequently require intubation for iMV is reported to be 45 - 51%.[7] Even with the addition of exogenous surfactant to NCPAP, there is still a failure rate of 25 -38%.[10] The criteria used to define failure of NCPAP varies from study to study, most likely explaining the variations in proportion of infants reported to have failed on NCPAP. Studies have used different parameters and values to define criteria for NCPAP failure. The criteria have included fraction of inspired oxygen (FiO2) ranging from 30 to 60% PaCO2 >60 or 65 mmHg, pH <7.20 or 7.25, pressure on NCPAP and persistent apnoeas.[10,11] Factors that have been found to be associated with CPAP failure have included lower gestational age (GA) and birth weight, amount of supplemental oxygen, male gender, FiO2/PaO2 ratio, PaCO2, pH and presence of apnoeas.[11,12] These factors indirectly reflect on the maturity of the infant and on the severity of the lung disease. A composite parameter that has been used to assess severity of illness in neonates is the clinical risk index for babies (CRIB) score.[13] Factors that are reported to be associated with NCPAP failure are similar to the parameters used in the CRIB score, therefore making it appropriate to use the CRIB score to predict neonates who may fail on NCPAP. The variables used in calculating the CRIB score are GA, birth weight, maximum base excess, congenital abnormalities, and minimum and maximum FiO2 requirements. These variables are assessed in the first 12 hours of life, making them less susceptible to treatment effects. A score of <5 has a smaller risk for mortality when compared with a score of >10.[13] Most of the studies that have looked at NCPAP failure rate were conducted in developed countries; therefore none of the babies was reported to have died on NCPAP as anyone who failed NCPAP was intubated and put on MV. In developing countries or settings where resources are limited, a number of preterm infants might die while receiving NCPAP. A study on outcomes of extremely-low-birth-weight (ELBW) infants managed with CPAP in a developing country, where NICU facilities are limited, reported a mortality rate of 8% on NCPAP.[10] Factors associated with deaths in VLBW infants managed with CPAP in a setting with limited resources are not known. In this study we sought to determine the proportion of VLBW infants managed with NCPAP outside NICU, their outcome as determined by the need for intubation for ventilation or death while on NCPAP and factors associated with these poor outcomes. This study was conducted after approval from the University of the Witwatersrand Human Research Ethics Committee.
Methods
This was a retrospective, descriptive study of VLBW infants weighing 800 - 1 499 g admitted to the high-care nursery (HCN) at Chris Hani Baragwanath Hospital (CHBH) in January to December 2012, managed with NCPAP within first 72 hours of life with or without surfactant. Medical records of VLBW infants weighing 800 g - 1 499 g were retrieved and reviewed for maternal and infant data. Data collection sheets were used to capture all the information required. A CRIB score was calculated for each neonate. CHBH is the referral hospital for all clinics in Soweto and surrounding areas. The protocol on the management of VLBW infants stipulated that those weighing >800 g with respiratory distress are started on NCPAP using flow drivers. Infants are only given surfactant using the intubation, surfactant and extubation (InSurE) technique if they require >40% FiO2 on NCPAP. The NCPAP is started with pressures of 4 - 6 cm H2O, and gradually increased up to a pressure of 8 cm H2O if there is no improvement in saturations on >60% supplemental oxygen. A second dose of surfactant is given 6 hours after the first dose if the FiO2 cannot be weaned below 40%. All patients with respiratory distress had arterial blood gas done by the time they were started on NCPAP. Because of limited resources, infants weighing <800 g were not offered NCPAP during the period of this record review. Patients admitted with respiratory distress had a full blood count and blood cultures done on admission, and a C-reactive protein (CRP) was obtained after 24 - 48 hours of birth. Patients who weighed >900 g were offered MV and transferred to NICU if they failed to maintain saturations above 88% despite NCPAP, a second dose of surfactant and required FiO2 >0.60, or if the arterial blood gas revealed a PaO2 <50 mmHg on an FiO2 >0.60, or a PaCO2 >55 mmHg with pH<7.25 or a PaCO2 >60 mmHg. The protocol on weaning patients off NCPAP was to gradually wean FiO2 to below 40% and then wean pressure on NCPAP to levels of 4 - 6 cm H2O, after which the patient was taken off NCPAP if saturations were maintained above 90%, and the patient was not distressed and had no apnoeas.
Data collected included maternal and infant characteristics, antenatal management, clinical diagnosis, laboratory findings, use of exogenous surfactant and outcome on NCPAP. Outcomes assessed were weaning off NCPAP in high care, need for MV, or death irrespective of cause while on NCPAP. Data were captured onto an Excel 2010 (Microsoft, USA) spreadsheet. The Excel spreadsheet was imported into Statistica version 12.0 (Statsoft Inc., USA) for statistical analysis. Means with standard deviations (SDs) and medians with ranges were used to describe the parametric and non-parametric data, respectively. Frequencies and percentages were used to describe categorical variables. In comparing those who failed on NCPAP and those who weaned off NCPAP, χ2 and Fisher's exact test were used to assess for statistically significant differences between categorical variables, and Student's i-test and Mann-Whitney (7-test for parametric and non-parametric continuous variables, respectively. Differences with p-values <0.05 were considered to be statistically significant. In order to determine predictors of need for MV or death on NCPAP, variables where p<0.1 on univariate analysis were included in the logistic regression model.
Results
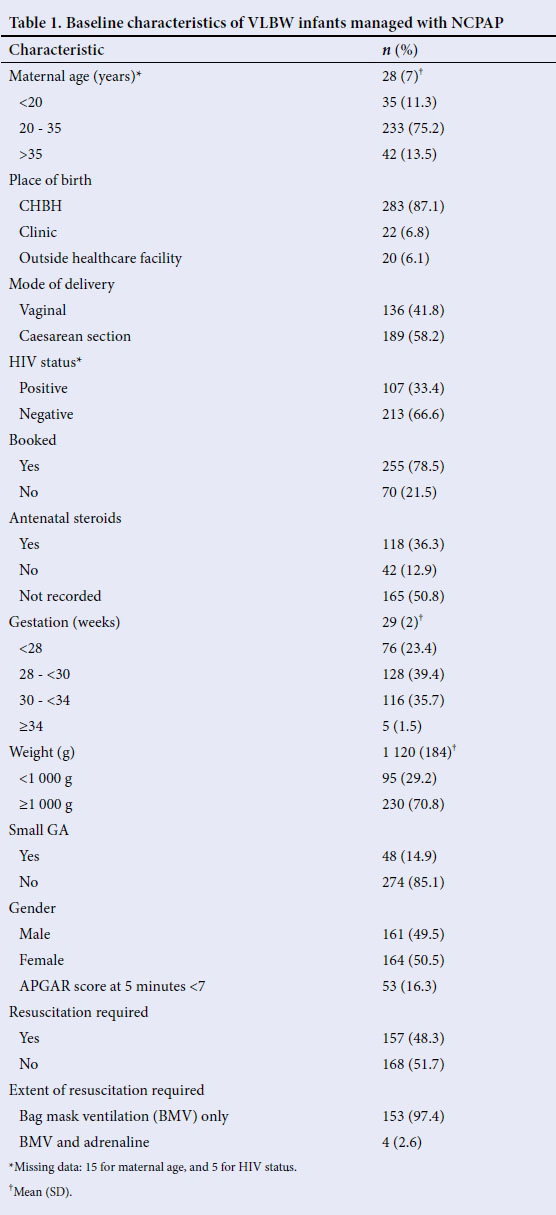
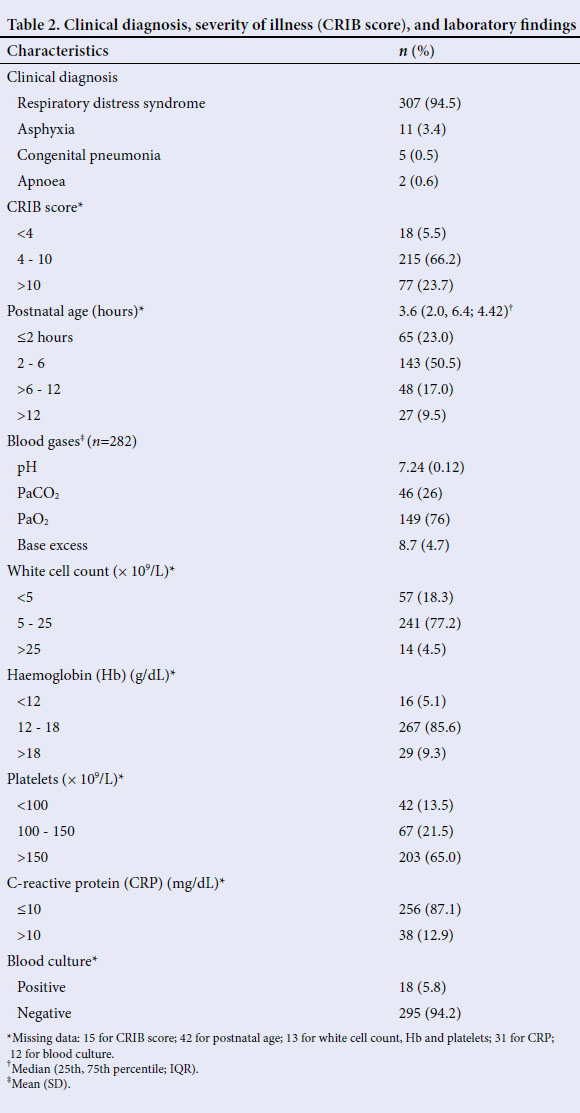
There were 21 601 live births at CHBH in 2012, of whom 806 were VLBW infants, accounting for 3.7% of all live births. Among these 806 VLBW infants, medical records of 635 (78.8%) were retrieved; the rest could not be found. Of these 635 VLBW infants with medical records, 325 (51.2%) patients were managed with NCPAP in the HCN. The majority of mothers (75.2%) were in the age group 20 - 35 years, and a third (33.4%) of VLBW infants were born to HIV-positive mothers. Only 78.5% of mothers attended antenatal care, defined as the mother having attended antenatal care at least once before delivery (Table 1). Antenatal steroids during labour were recorded as being given in only 36.3% of patients and not given in 12.9%, and there were no records of whether or not antenatal steroids were given in 50.8% of cases. Only 29% weighed between 800 and 1 000 g. The GA of most (98.5%) patients was <34 weeks, as determined by Ballard score. Among the 322 patients who had GA recorded, 48 (14.9%) were small for GA (SGA). Numbers of male and female babies were equally distributed. Forty-seven percent required resuscitation, with most of them only requiring bag mask ventilation and 16.3% having an Apgar score <7 at 5 minutes. The common diagnosis on admission was RDS. About two-thirds of patients (66.2%) had a CRIB score of 4 - 10, and 23.7% a CRIB score of >10. Arterial blood gases done before administration of NCPAP showed a mean (SD) pH of 7.24 (0.12), PaCO2 46 (26) mmHg, PaO2 149 (76) mmHg, and base deficit of 8.70 (4.7) mmol/L (Table 2). The full blood count on admission showed that 22.8% had an abnormal white cell count (18.3% with leukopenia and 4.5% with leukocytosis), 5% had anaemia (haemoglobin <12 g/dL) and 25% had thrombocytopenia (platelet count <150 χ 109/L). Only 12.9% had CRP >10 mg/L and 5% had positive blood cultures. The median age when NCPAP was started was 3.6 hours.
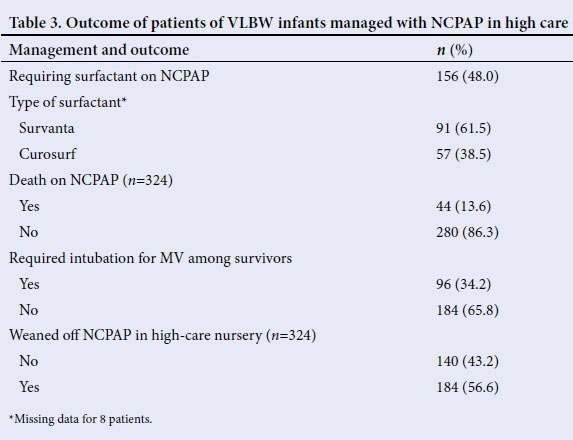
Out of the 325 VLBW infants who received NCPAP, 156 (48%) required surfactants in addition to NCPAP, 44 (13.5%) died while on NCPAP and 96 (34.2%) survivors required intubation for MV (Table 3). Among the 156 who received surfactant, 20 (12.8%) required a second dose. The median postnatal age at time of death among those who died on CPAP was 64 hours (range 3 - 420 hours). Overall, 56.6% of VLBW infants managed with NCPAP were weaned off NCPAP while in HCN, and 43.4% either required intubation for MV or died while on NCPAP, therefore were not weaned off NCPAP within the HCN.
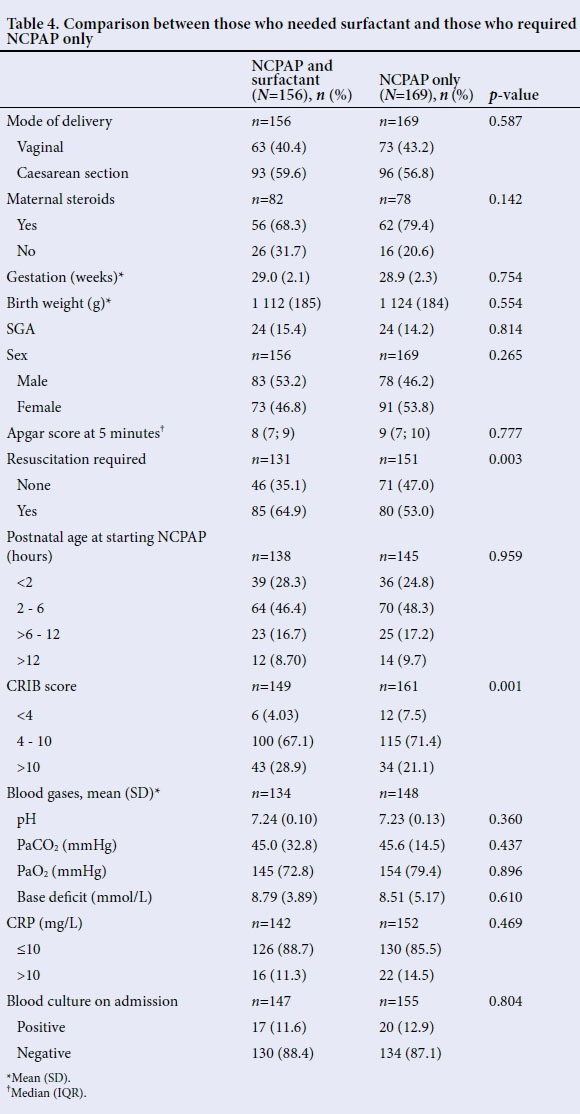
There were more patients who needed resuscitation (64.9 v. 52.7%, £=0.003), and who had a CRIB score >10 (28.9 v. 20.2%, £=0.001) in the VLBW, and who required surfactant in addition to NCPAP compared with those who did not require surfactant (Table 4). There were no statistical significant differences in other variables.
Among the survivors on NCPAP, 96 needed intubation for MV. There were more patients who were SGA (22.1 v. 12.0%, p=0.027), had lower Apgar score at 5 minutes (median 8 v. 9, £=0.013) and a CRIB score >10 (37.4 v. 12.0%, £<0.001) among those who needed MV (Table 5). They also had a lower PaO2 (137 (67) v. 161 (81) mmHg, £=0.022) and higher base deficit (9.0 (4.4) v. 7.8 (4.0) mmol/L, £=0.034) compared with those who did not need ventilation. There were no statistical significant differences in other variables between those who required MV and those who did not require ventilation among the survivors. On multivariate logistic regression analysis, the predictors of need for intubation for MV were SGA (£=0.033), Apgar score at 5 minutes (£=0.042) and CRIB score (£=0.005).
Among all the patients who were managed with NCPAP within the first 72 hours of life, 44 died while on NCPAP and 280 survived, either weaning off NCPAP or requiring intubation for MV (Table 6). There were more patients with a CRIB score >10 among those who died than among those who survived (51.2 v. 20.9%, £<0.001). Patients who died had lower birth weight (944 (142) v. 16 147 (175) g, £<0.001), were of lower GA (27 (2) v. 29 (2) weeks, £<0.001), had a lower pH (7.165 (0.16) v. 7.25 (0.11)), lower PaO2 (120 (62) v. 153 (77), £=0.011) and higher base deficit (11.9 (6.0) v. 8.2 (4.2) mmol/L, £<0.001) than those who survived. There were no statistically significant differences in other variables between those who died and those who survived. On multivariate logistic regression analysis, the only predictor of death on NCPAP was birth weight (£<0.001).
Discussion
VLBW infants account for a significant number of infants who require respiratory support soon after delivery. Providing NCPAP has been reported to reduce mortality and the need for intubation for MV in this group of infants.[14] Success or failure rates of NCPAP are often reported from developed countries, where it is often initiated soon after delivery and offered in a setting where resources are not restricted, typically administered in an NICU setting. In developing countries where resources are limited, NCPAP is often offered outside the NICU setting. Some of the infants may not get access to NICU and therefore die on NCPAP. It is important to assess the success or failure rate of NCPAP in a setting where intubation for MV might not always be accessible to those who fail NCPAP. This study looked at the short-term outcomes of babies who were treated with NCPAP with or without surfactant outside a NICU setting. The short-term outcomes assessed were death on NCPAP or need for intubation for MV, and these were labelled as NCPAP failures.
The main findings in this study were that 51% of VLBW infants weighing between 800 and 1 499 g inclusive required NCPAP within the first 72 hours of life and were managed in a HCN. The median age of starting NCPAP was about 3.5 hours of life. Forty-eight percent of VLBW infants required exogenous surfactant despite NCPAP. Thirteen percent of VLBW infants managed with NCPAP died while receiving NCPAP, and 34% of the survivors required iMV, with an overall CPAP failure rate of 43%. The patients who required iMV had lower median Apgar score at 5 minutes, higher CRIB score, lower PaO2 and higher base deficit, and those who died on NCPAP had a CRIB score >10, were ELBW and lower gestation, had lower pH and PaO2, and had a higher base deficit than survivors.
Among the VLBW infants managed with NCPAP in whom use of antenatal steroids was recorded, <50% had received antenatal steroids. This most likely contributed to these infants having severe disease as shown by high CRIB score, requiring NCPAP and having poor outcomes, as it has been shown that use of antenatal steroids reduces the incidence of RDS and mortality in preterm infants.[15] In the settings where NICU facilities are limited, management of VLBW infants outside NICU is feasible. While 13% died on NCPAP, 66% of survivors weaned off NCPAP without the need for intubation for MV.
There are not many studies that have reported on use of NCPAP in VLBW infants outside NICU. One of the studies from a developing country reported on use of NCPAP outside the NICU and showed that 92% of ELBW infants were managed with NCPAP outside NICU set-up with good outcomes.[10] Recently a report from a district hospital showed that managing patients outside a NICU is possible, improves outcomes and gives an opportunity to offer support while waiting for transport for transfer to a facility with NICU.[16] This suggests that CPAP can be safely used in resource-limited settings as the first line of therapy, with great benefits.
Forty-eight percent of patients who were managed with NCPAP in this report also required exogenous surfactant. This is similar to the 46% reported by Dunn et al.l9] Patients who required exogenous surfactant were smaller and sicker, as reflected by higher CRIB score, and had factors that might have inhibited the production or function of surfactant, namely acidosis, resulting in greater need for surfactant. Randomised trials point towards using early NCPAP as an alternative to surfactant administration in preterm infants with RDS,[17] but in smaller VLBW infants elective administration of surfactant may decrease the need for MV. One-third of patients required intubation for MV despite NCPAP. Other studies have reported higher numbers of 40 - 48% of patients managed with NCPAP requiring intubation for MV.[18,19] The reasons for the lower rates MV need in this study are most likely due to those neonates weighing <1 000 g not being considered for ventilation because of limited NICU beds. Other factors associated with need for intubation for MV in infants managed with NCPAP have been reported to be a high FiO2 (>0.3) requirement in the first hours of life, and moderate-to-severe respiratory distress syndrome.[20] This is similar to the findings in this study that showed that the need for iMV was associated with high CRIB score, which represents severity of illness.
Thirteen percent of patients died on NCPAP. Most of these deaths were babies who were of lower gestation and birth weight. In areas where resources are limited, infants at borders of viability are often not offered iMV in the NICU. Where this study was conducted, the majority (those weighing <900 g) of ELBW infants were not offered iMV. The highest ventilator support they could get was NCPAP. The mortality rate of 13% on NCPAP reported in this study is higher than that reported by Kirsten et al.,[10] who reported a mortality rate of 8%. The explanation for this difference could be due to differences in severity of illness and GA, which are reflected in a CRIB score, but the study by Kirsten et al. did not report on the CRIB score of babies they studied.
There are some limitations in the data collection in this study. The retrospective design of the study meant that not all the files could be retrieved. Some files were missing from the filing room and from the files that were retrieved, and some data were missing or incomplete. This is unlikely to have affected the results, as a significant number (79%) of files of all VLBW infants were retrieved. It is unlikely that the missing data would have affected the findings in this study as the missing data was <20% for most variables except for antenatal steroids.
Conclusion
Use of NCPAP in VLBW infants can be applied outside a NICU setting with reasonable short-term outcomes. It is effective in the management of respiratory distress, as about 87% of patients survive on NCPAP, although about one-third of those who survive on NCPAP end up requiring iMV. The patients who died on NCPAP were those of lower GA and those with severe illness. The ones who died with lower GA were most likely not offered iMV because of limited NICU beds. The high failure rate on NCPAP, which included deaths, is therefore partly related to inadequate resources. There is therefore a need to improve access to iMV to fully appreciate the impact of providing NCPAP, especially to those who are of lower GA and who are critically ill.
References
1. Gregory GA, Kitterman JA, Phibbs RH, Tooley WH, Hamilton WK. Treatment of the idiopathic respiratory-distress syndrome with continuous positive airway pressure. N Engl J Med 1971;284(24):1333-1340. http://dx.doi.org/10.1056/NEJM197106172842401 [ Links ]
2. Verder H. Nasal CPAP has become an indispensable part of the primary treatment of newborns with respiratory distress syndrome. Acta Paediatr 2007;96(4):482-484. http://dx.doi.org/10.1111/j.1651-2227.2007.00263.x [ Links ]
3. De Paoli AG, Morley C, Davis PG. Nasal CPAP for neonates: What we know in 2003? Arch Dis Child Fetal Neonatal Ed 2003;3(88):F168-F172. http://dx.doi.org/10.1136/fn.88.3.F168 [ Links ]
4. De Winter JP, de Vries MA, Zimmermann LJ. Clinical practice: Noninvasive respiratory support in newborns. Eur J Pediatr 2010;169(7):777-782. http://dx.doi.org/10.1007/s00431-010-1159-x [ Links ]
5. Aly H, Massaro AN, Patel K, El-Mohandes AA. Is it safer to intubate premature infants in the delivery room? Pediatrics 2005;115(6):1660-1665. http://dx.doi.org/10.1542/peds.2004-2493 [ Links ]
6. Ammari A, Suri M, Milisavljevic V, et al. Variables associated with the early failure of nasal CPAP in very low birth weight infants. J Pediatr 2005;147(3):341-347. http://dx.doi.org/10.1016/j.jpeds.2005.04.062 [ Links ]
7. Fuchs H, Lindner W, Leiprecht A, Mendler MR, Hummler HD. Predictors of early nasal CPAP failure and effects of various intubation criteria on the rate of mechanical ventilation in preterm infants of <29 weeks' gestational age. Arch Dis Child Fetal Neonatal Ed 2011;96(5):F343-347. http://dx.doi.org/10.1136/adc.2010.205898 [ Links ]
8. Ho JJ, Subramaniam P, Davis PG. Continuous distending pressure for respiratory distress in preterm infants. Cochrane Database Syst Rev 2015;4(7):CD002271.http://dx.doi.org/10.1002/14651858.CD002271.pub2 [ Links ]
9. Dunn MS, Kaempf J, de Klerk A, et al. Randomized trial comparing 3 approaches to the initial respiratory management of preterm neonates. Pediatrics 2011;128(5):e1069-1076. http://dx.doi.org/10.1542/peds.2010-3848 [ Links ]
10. Kirsten GF, Kirsten CL, Henning PA, et al. The outcome of ELBW infants treated with NCPAP and InSurE in a resource-limited institution. Pediatrics 2012;129(4):e952-959. http://dx.doi.org/10.1542/peds.2011-1365 [ Links ]
11. Swietlinski J, Bachman T, Gajewska E, et al. Factors affecting outcomes in very low birth weight infants treated electively with nasal continuous positive airway pressure. J Perinatol 2010;30(2):112-117. http://dx.doi.org/10.1038/jp.2009.135 [ Links ]
12. Rocha G, Flor-de-Lima F, Proenca E, et al. Failure of early nasal continuous positive airway pressure in preterm infants of 26 to 30 weeks' gestation. J Perinatol 2013;33(4):297-301. http://dx.doi.org/10.1038/jp.2012.110 [ Links ]
13. Sarquis AL, Miyaki M, Cat MN. [The use of CRIB score for predicting neonatal mortality risk]. J Pediatr (Rio J) 2002;78(3):225-229. [ Links ]
14. Kambarami R, Chidede O, Chirisa M. Neonatal intensive care in a developing country: Outcome and factors associated with mortality. Cent Afr J Med 2000;46(8):205-207. [ Links ]
15. Mwansa-Kambafwile J, Cousens S, Hansen T, Lawn JE. Antenatal steroids in preterm labour for the prevention of neonatal deaths due to complications of preterm birth. Int J Epidemiol 2010;39(Suppl 1):i122-i133. http://dx.doi.org/10.1093/ije/dyq029 [ Links ]
16. Hendriks H, Kirsten GF, Voss M, Conradie H. Is continuous positive airway pressure a feasible treatment modality for neonates with respiratory distress syndrome in a rural district hospital? J Trop Pediatr 2014;60(5):348-351. http://dx.doi.org/10.1093/tropej/fmu025 [ Links ]
17. Polin RA, Carlo WA, Committee on Fetus and Newborn, American Academy of Pediatrics. Surfactant replacement therapy for preterm and term neonates with respiratory distress. Pediatrics 2014;133(1):156-163. http://dx.doi.org/10.1542/peds.2013-3443 [ Links ]
18. Morley CJ, Davis PG, Doyle LW, et al. Nasal CPAP or intubation at birth for very preterm infants. N Engl J Med 2008;358(7):700-708. http://dx.doi.org/10.1056/NEJMoa072788 [ Links ]
19. Schmolzer GM, Kumar M, Pichler G, Aziz K, O'Reilly M, Cheung PY. Non-invasive versus invasive respiratory support in preterm infants at birth: Systematic review and meta-analysis. BMJ 2013;347:f5980. http://dx.doi.org/10.1136/bmj.f5980 [ Links ]
20. Dargaville PA, Aiyappan A, de Paoli AG, et al. Continuous positive airway pressure failure in preterm infants: Incidence, predictors and consequences. Neonatology 2013;104(1):8-14. http://dx.doi.org/159/000346460 [ Links ]
 Correspondence:
Correspondence:
S Velaphi
sithembiso.velaphi@wits.ac.za
Accepted 29 November 2015.














