Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Child Health
versão On-line ISSN 1999-7671
versão impressa ISSN 1994-3032
S. Afr. j. child health vol.10 no.3 Pretoria Set. 2016
http://dx.doi.org/10.7196/sajch.2016.v10i3.1140
RESEARCH
Characteristic of monosymptomatic and non-monosymptomatic childhood nocturnal enuresis in Benin City, Nigeria
N J IduoriyekemwenI; D U NwaneriII
IMBBS, FWACP. Department of Child Health, University of Benin/University of Benin Teaching Hospital, Benin City, Nigeria
IIMBBS, MPH, FMCPaed. Institute of Child Health, University of Benin/University of Benin Teaching Hospital, Benin City, Nigeria
ABSTRACT
BACKGROUND. In recent years, nocturnal enuresis (NE) has been classified into monosymptomatic nocturnal enuresis (MNE) and non-monosymptomatic nocturnal enuresis (NMNE) on the basis of the absence or presence of daytime voiding symptoms. Identifying clinical features that differentiate MNE from NMNE would aid in quick diagnosis, which would foster the introduction of early and appropriate therapeutic care options.
OBJECTIVE. To identify distinguishing characteristics of MNE and NMNE in Nigerian children.
METHODS. The parents of children in public primary and secondary schools in Egor local government area, Edo State, were interviewed using a semi-structured questionnaire.
RESULTS. The total studied population included 1 221 parent/child pairs. Of the children studied, 228 were enuretic. There were 149 (65.4%) MNE and 79 (34.6%) NMNE children. Enuretic children with a history of multiple wetting per night or whose parents observed difficulty awakening them from sleep were significantly more likely to be in the NMNE group.
CONCLUSION. MNE is twice as common as NMNE and the main distinguishing features between the two groups of enuretic children are multiple wetting at night and difficulty awakening the child from sleep. These were significantly more commonly observed among the NMNE group of children.
Nocturnal enuresis (NE), also known as bed-wetting, is the intermittent involuntary passage of urine during sleep in a child 5 years and older.[1] It is a very common problem of childhood, affecting children of all races worldwide.[2] Although bed-wetting does not cause any physical harm to the child, it is a cause of great psychological distress to the family and to the enuretic child.[3,4] Several studies worldwide have classified children with either primary or secondary NE based on whether the child has never been dry at night (primary NE (PNE)) or has been dry for at least 6 months (secondary NE (SNE)).[5-7] The majority of studies on enuresis have been on PNE, which has been reported as the most common type of NE.[5-9] However, recently NE has also been further classified into monosymptomatic NE (MNE) and non-monosymptomatic NE (NMNE) on the basis of the absence or presence of daytime voiding symptoms.[1,10] This classification of NE is essential because children with NE who have daytime voiding or lower urinary tract symptoms are pathogenetically and clinically different from those who bed-wet at night only. In addition, children with MNE and NMNE require different modalities for management.
Most of the studies in Nigeria on NE have been on the determination of the prevalence of NE in primary school children.[11-14] There is no study that has classified enuretic children using the recent classification (MNE and NMNE), indicating that children with daytime voiding and/or lower urinary tract symptoms are usually missed both in terms of diagnosis and treatment modalities.
This study was conducted in order to identify distinguishing characteristics of MNE and NMNE enuresis in Nigerian children using children residing in Egor local government area (LGA), Benin City.
Methods
This descriptive, cross-sectional survey was carried out from April to August 2014 during the third-term of the school year. The study location was Egor LGA in Edo State, which is one of the five LGAs in Benin City, a predominantly urban setting with nine political wards, of which two are rural. The main occupation of the inhabitants includes farming, trading and the civil service. There are 17 public primary and 12 secondary schools (government-owned schools). Subjects were parent/child pairs of the public primary and secondary schools in Egor (LGA), Edo State. The population was chosen because children in public schools derive from different social classes, ensuring a good representation of all social classes.
A pre-tested, self-administered questionnaire was used. It was distributed to all the parents by their children. The completed questionnaires were returned the following day. The information captured included parent demography (mother's age, mother's level of education and occupation, father's level of education and occupation, marital status and family size). Social class of the child's family was determined by the method described by Olusanya et al.[15] Information on the child's demographic characteristics was also obtained (age, gender and birth order). In addition, information was sought regarding the child's enuretic characteristics, namely:
• the presence of NE
• onset of NE
• presence of daytime voiding symptoms
• frequency of enuresis
• history of multiple voidings per night
• predominant night period when wetting usually occurs
• family history of enuresis
• relationship of the individual with a positive history of enuresis to the child.
Only children with a history of bed-wetting since birth were recruited. Children were classified as NMNE when there was no history of daytime symptoms (voiding frequency, voiding urgency or daytime wetting). If they had daytime symptoms and nocturnal wetting, they were classified as NMNE. The severity of bed-wetting was based on the frequency of nocturnal bed-wetting. If a child bed-wet only once a week or one to two times a month, she or he was classified as having mild NE; if bed-wetting occurred twice or more in a week, it was classified as moderate NE; and if the child wet every night it was classified as severe NE. Family size was defined as small if the number of children residing in the home was equal to or less than five and large if the number was greater than five.
Data obtained were entered into IBM Statistical Package for Social Sciences (SPSS) version 20.0 (USA) and were analysed using the same software. Quantitative variables were summarised using means and standard deviations (SDs), and comparisons of proportions were done accordingly. The significance of association between variables was tested using χ2 and Fisher's exact tests where appropriate, while independent t-test was used for comparison of means. The level of significance of each test was set at p<0.05.
Ethical considerations
An ethical certificate for this study was obtained from the Research and Ethics Committee of the College of Medical Science, University of Benin, and permission was sought from the Ministry of Education and the headpersons of each primary school and the principal of each secondary school. Written informed consent forms were given to each child to deliver to their parents at the first visit to the schools. Parents who returned a signed informed consent were recruited in the study. All the children of both the primary and secondary schools in the LGA whose parents gave written informed consent were recruited for this study.
Results
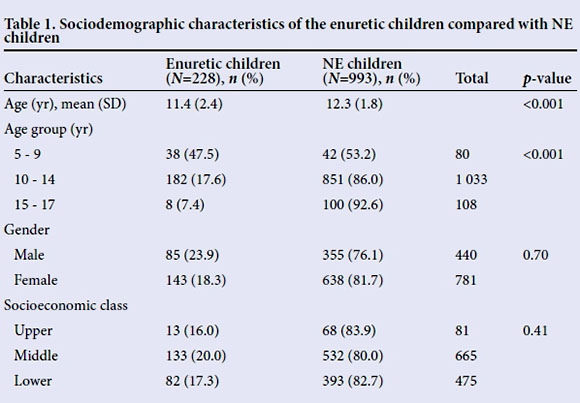
A total of 1 800 questionnaires were distributed to the parents of the students, of which 1 574 were returned, giving a response rate 87.4%. However, only 1 221 questionnaire were correctly completed; therefore the total studied population was 1 221 parent/child pairs. The mean (SD) age of the 1 221 children analysed was 12.1 (1.9) years, median 12 (range 5 - 17) years. Most of the children (84.6%) were under 10 years of age and were female (64.0%). Of the 1 221 children analysed in the study, 228 were enuretic. The mean age of these children was 11.4 (2.4) years and the modal age was 14 years. The mean age of the enuretic children was significantly younger than that of non-enuretic children (p<0.0001). The proportion of children with enuresis (47%) was highest in the 5 - 9-year-old age group, falling to 7% in the 15 - 17-year-olds. Age was significantly associated with enuresis (p<0.001). There were slightly more enuretic male children (23.9%) than enuretic female children (18.3%), however this was not statistically significant (p=0.70). The prevalence of enuresis was no different between the three socioeconomic classes (Table 1).
A total of 149 (65.4%) of the 228 enuretic children were MNE, while 79 (34.6%) were NMNE. Therefore, the proportion of MNE to NMNE children was 1.8:1. There was no significant difference between the two groups of enuretic children in terms of their age (p=0.39), gender (p=0.20) and socioeconomic class (p=0.07) (Table 2). The proportion of male and female children with MNE and NMNE was similar, and there was no statistical difference in proportions of children with the two types of NE between the socioeconomic classes.
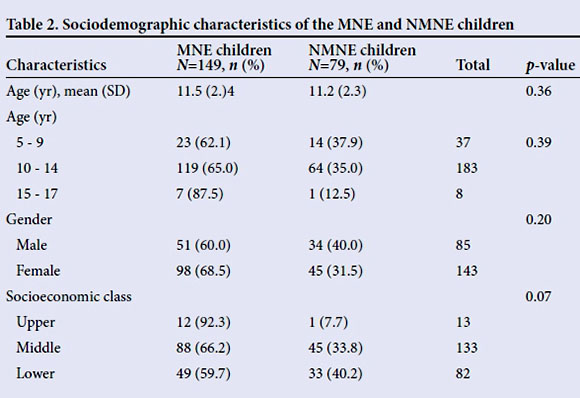
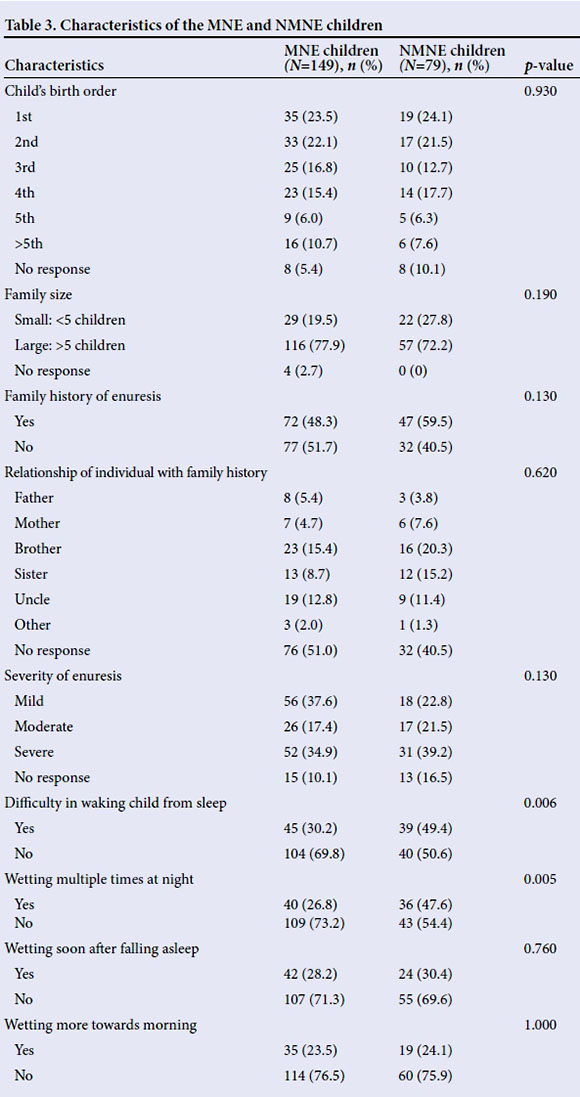
Table 3 shows the characteristics of the MNE and NMNE children. Children whose parents observed difficulty waking their children from sleep were significantly more likely to have NMNE than the MNE (p=0.006). Similarly, enuretic children with history of multiple wetting per night were significantly more likely to have NMNE than MNE (p=0.005). However, there was no statistical significant difference between MNE and NMNE children in terms of the child's birth order, family size, family history of enuresis, severity of enuresis and predominant period of the night that wetting occurs (e.g. wetting soon after falling asleep or wetting occurring more towards morning).
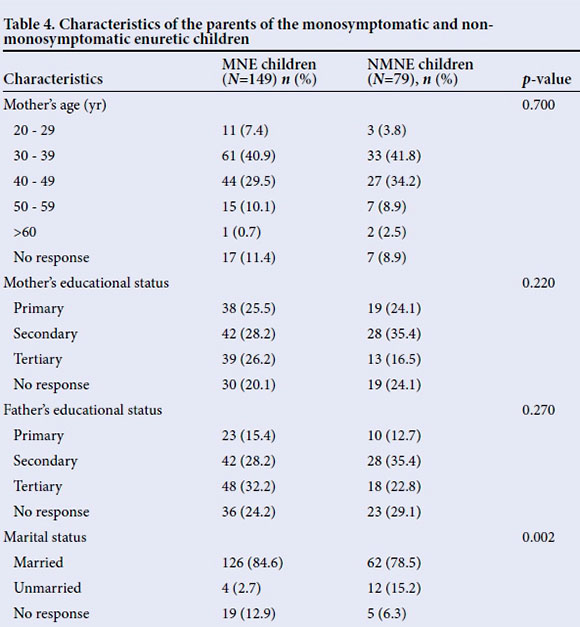
Parental sociodemographic characteristics were also not significantly different in the two groups of enuretic children (Table 4) except for marital status of the parents. The proportions of unmarried parents were significantly greater in the NMNE group of children, compared with MNE children (p=0.002).
The association between the child's age group and other characteristics was determined for each of the groups of enuretic children. Among the MNE children, the child's age group was significantly associated with severity of bed-wetting (p=0.013), family history of enuresis (p=0.04), father's educational level (p=0.014) and marital status of parents (p=0.028). However, among the NME children, no association was observed between child's age group and other characteristics.
Discussion
Although NE has been extensively studied in relation to the onset of bed-wetting (primary and secondary bed-wetting),[5-9] very few studies have been conducted in terms of the absence or presence of daytime voiding symptoms,[16,17] which means there is a dearth of data for comparison. In a large population study on MNE and NMNE by Butler and Heron,[16] the proportion of MNE children to NMNE children was documented as 2:1, a figure similar to that found in the present study. This observation, therefore, supports the notion that MNE is twice as common as NMNE. The main distinguishing features between children with MNE and NMNE observed in this study were that children with NMNE were more likely to bed-wet multiple times per night and were more difficult to rouse from sleep. There is a dearth of studies on distinguishing MNE from NMNE, therefore precluding comparison. The presence of lower urinary tract dysfunction in children with NMNE may explain why they tend to bed-wet multiple times per night compared with children with MNE. In a study by Naseri and Hiradfar,[17] bladder dysfunctions -overactive bladder, detrusor hyperactivity conditions which predispose to multiple wetting - were detected by urodynamic studies, and they were reported to be more common in children with NMNE. Difficulty in rousing child from sleep, which is one of the three well-established pathophysiological factors of MNE,[2,18] was not observed in our study to be exclusive to the MNE group of children. This, therefore, justifies the need for extensive interview of any child with NE to reveal if they have daytime voiding symptoms or lower urinary tract symptoms, as investigative evaluation for the children with NMNE is mandatory. Parental marital status was the only other distinguishing factor observed in this study. The observation that in the homes where the parents were unmarried (divorced, separated, etc.) NMNE was more common compared with MNE, may imply that family dysfunction is an important associated factor in NMNE and in secondary enuresis. Dysfunctional or split families are an identifiable stressful environmental factor, which predisposes children to greater risk of developmental and behavioural problems.[19] The import of this is the inclusion of psychotherapy for both child and family as relevant adjuvant therapeutic option in management of children with NMNE.
Although there were no observed differences between the two enuretic groups of children in terms of sociodemographic characteristics, the following trends were observed in this study.
The mean ages of children with MNE and NMNE were similar. This finding is in consonance with the works of Naseri and Hiradfar,[17] who also studied a similar age range as in this study. Of note, however, is that the mean (SD) ages of the children in the study by Naseri and Hiradfar[17] were lower in both groups of children (8.66 (2.2) years in those with MNE and 8.2 (2.5) years in those with NMNE) when compared with 11.5 (2.4) years for the children with MNE and 11.2 (2.3) years for those with NMNE observed in the present study. These differences may be explained by the fact that a larger proportion of children in this study were >10 years, while in the study by Naseri and Hiradfar[17] the majority of the children were <10 years old.
The observed trend from several other studies that the prevalence of NE decreases with increasing age[5-9,20-22] was also observed in this study, even among the NMNE group of children. The reason why the MNE group of children did not show this trend is difficult to explain. The widely documented finding that NE is more common in males than females[5-9,20-22] was also observed in this study; however, when comparing the MNE and NMNE group of enuretic children, this difference in gender was not observed. This is in contrast to the works of Naseri and Hiradfar[17] and Bakker et al.,[23] who reported that among the MNE group, males were recorded more than females but the reverse was observed among the NMNE group. The difference is difficult to explain, because even in a study on lower urinary tract symptoms in children who do not bed-wet, the daytime voiding symptoms were also reported to be more common in girls than boys.[19] Of note is that some studies on MNE reported that the sex difference is only observed until the age of 10 years, and thereafter the frequency is the same for both boys and girls.[24] This may be the reason for the findings in this study, as the majority of the children were older than 10 years.
The limitation of this study was that the children could not be evaluated radiologically owing to financial constraints. Radiological assessment would have aided in diagnosing the specific lower urinary tract dysfunction the children with NMNE had. In addition, daytime voiding symptoms used to define NMNE were only ascertained by history; a 48-hour frequency and volume chart was not used to confirm.
Conclusions
MNE is twice as common as NMNE, and the main distinguishing features between the two groups of enuretic children are multiple wetting at night and difficulty in waking up a child from sleep, which was significantly observed among the NMNE group of children. We therefore recommend that while evaluating patients, the presence of these factors (multiple wetting at night and difficult sleep arousal) should alert the physician to probe for the presence of lower urinary symptoms or daytime voiding symptoms. This would help reduce missed opportunities in the diagnosis of children with NMNE.
Acknowledgements. The authors thank Mr Moses Adekunle Abiodun who assisted in data collection, Miss Itohan Ibhawa for data entry into Microsoft Excel and the management of the selected schools for providing the enabling environment for this study.
References
1. Austin PF, Bauer SB, Bower W, et al. The standardization of terminology of lower tract function in children and adolescent: Update report from the Standardization Committee of the International Children's Continence Society. J Urol 2014;191(6):1863-1865. DOI:10.1016/j.juro.2014.0U10 [ Links ]
2. Wright A. Evidence-based assessment and management of childhood enuresis. Paediatr Child Health 2008;18(12):561-567. DOI:10.1016/j.paed.2008.09.006 [ Links ]
3. Fritz G, Rockney R, Bernet W, et al. Practice parameter for the assessment and treatment of children and adolescents with enuresis. J Am Acad Child Adolesc Psychiatry 2004;43:(12):1540-1550. DOI:10.1097/01.chi.0000142196.41215.cc [ Links ]
4. Joinson C, Heron J, Emond A, Butler R. Psychological problems in children with bed-wetting and combined (day and night) wetting: A UK population-based study. J Paediatr Psychol 2007;32(5):605-616. DOI:10.1093/jpepsy/jsl039 [ Links ]
5. Chang P, Chen WJ, Tsai WY, Chiu YN. An epidemiological study of nocturnal enuresis in Taiwanese children. BJU Int 2001;87(7):678-681. DOI:10.1046/j.1464-410x.2001.02161.x [ Links ]
6. Hazza I, Tarawneh H. Primary nocturnal enuresis among school children in Jordan. Saudi J Kidney Dis Transpl 2002;13(4):478-480. [ Links ]
7. Kanaheswari Y. Epidemiology of children nocturnal enuresis in Malaysia. J Paediatr Child Health 2003;39(2):118-123. DOI:10.1046/j.1440-1754.2003.00105.x [ Links ]
8. Yeung CK, Sreedhar B, Sihoe JD, Sit FK, Lau J. Differences in characteristics of nocturnal enuresis between children and adolescents: A critical appraisal from a large epidemiological study. BJU Int 2006;97(5):1069-1073. DOI:10.1111/j.1464-410X.2006.06074.X [ Links ]
9. Ozden C, Ozdal O, Altinova S, Oguzulgen I, Urgancioglu G, Memis A. Prevalence and associated factors of enuresis in Turkish children. Int Braz J Urol 2007;33(2):216-222. [ Links ]
10. Djurhuus JC. Definitions of subtypes of enuresis. Scand J Urol Nephrol Suppl 1999;202:5-7. [ Links ]
11. Osungbade KO, Oshiname FO. Prevalence and perception of nocturnal enuresis in children of a rural community in southwestern Nigeria. Trop Doct 2003;33(4):234-236. [ Links ]
12. Etuk IS, Ikpeme O, Essiet GA. Nocturnal enuresis and its treatment among primary school children in Calabar Nigeria. Niger J Paediatr 2011;38(2):78-81. [ Links ]
13. Paul NI, Alikor EA, Anochie IC. Prevalence of enuresis among primary school children in Port Harcourt. Niger J Paediatr 2012;39(1):18-21. [ Links ]
14. Chinawa JM, Obu HA, Manyike PC, Odetunde OI. Nocturnal enuresis among school-age children in south-eastern Nigeria: A concealed social malaise. Int J Trop Dis Health 2014;4(6):683-695. [ Links ]
15. Olusanya O, Okpere E, Ezimokai M. The importance of social class in voluntary fertility control in a developing country. West Afr J Med 1985;4:205-212. [ Links ]
16. Butler R, Heron J. Exploring the difference between mono- and polysymptomatic nocturnal enuresis. Scand J Urol Nephrol 2006;40(4):313-319. [ Links ]
17. Naseri M, Hiradfar M. Monosymptomatic and non-monosymptomatic nocturnal enuresis: A clinical evaluation. Arch Iran Med 2012;15(11):702-706. [ Links ]
18. Tryggve N. Nocturnal enuresis - theoretical background and practical guidelines. Pediatr Nephrol 2011;26(8):1207-1214. DOI:10.1007/s00467-011-1762-8 [ Links ]
19. Vaz GT, Vasconcelos MM, Oliveira EA, et al. Prevalence of lower urinary tract symptoms in school children. Pediatr Nephrol 2012;27(4):597-603. DOI:10.1007/s00467-011-2028-1 [ Links ]
20. Shan S, Ahmed A, Rehman SU, Rehman G. Prevalence and risk factors of monosymptomatic nocturnal enuresis in Pakistani children. Khyber J Med Sci 2011;3(1):16-20. [ Links ]
21. Abu Merhi B, Hammoud A, Ziade F, Kamel R, Rajab M. Mono-symptomatic nocturnal enuresis in Lebanese children: Prevalence, relation with obesity, and psychological effect. Clin Med Insights Pediatr 2014;8:5-9. DOI:10.4137/CMPed.S13068 [ Links ]
22. Iduoriyekemwen NJ, Ibadin MO, Abiodun PO. Survey of childhood enuresis in the Ehor community, the Edo State, Nigeria. Saudi J Kidney Dis Transpl 2006;17(2):177-182. [ Links ]
23. Bakker E, van Sprundel M, van der Auwera JC, van Gool JD, Wyndaele JJ. Voiding habits and wetting in a population of 4 332 Belgian school children aged between 10-14 years. Scand J Urol Nephrol 2002;36(5):354-362. [ Links ]
24. Meneses R. Monosymptomatic nocturnal enuresis. J Pediatr (Rio J) 2001;77(3):161-168. [ Links ]
 Correspondence:
Correspondence:
N J Iduoriyekemwen
nosaiduos2006@yahoo.com














