Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Child Health
versão On-line ISSN 1999-7671
versão impressa ISSN 1994-3032
S. Afr. j. child health vol.10 no.2 Pretoria Jul. 2016
http://dx.doi.org/10.7196/sajch.2016.v10i2.1054
RESEARCH
The impact of a change in referral pathway on a paediatric short-stay ward in Cape Town, South Africa
H FinlaysonI; L SmitII; T M EsterhuizenIII; M KrugerIV
IFCPaed (SA), Cert Id (SA) (Paed). Tygerberg Hospital and Department of Paediatrics and Child Health, Stellenbosch University, Cape Town, South Africa
IIMMed (Paed), FCPaed (SA), MPhil. Tygerberg Hospital and Department of Paediatrics and Child Health, Stellenbosch University, Cape Town, South Africa
IIIMSc (Epidemiology). Biostatistics Unit, Centre for Evidence-Based Health Care, Community Health Division, Stellenbosch University, Cape Town, South Africa
IVMMed (Paed), MPhil, PhD.Tygerberg Hospital and Department of Paediatrics and Child Health, Stellenbosch University, Cape Town, South Africa
ABSTRACT
BACKGROUND: The opening of the new Khayelitsha District Hospital in April 2012 coincided with a change in referral pathway to Tygerberg Hospital (TBH) for children requiring specialist care.
OBJECTIVE: To determine the disease burden impact of the referral pathway change on paediatric short-stay ward admissions at TBH.
METHODS: A retrospective cohort study, analysing routine health information as captured in ward admissions registers over two similar seasonal periods: 1 April - 30 September 2011 (prior to referral change) and 1 April - 30 September 2012 (post referral change).
RESULTS: Paediatric short-stay ward admissions remained similar, but a statistically significant increase in the number of admissions from Khayelitsha sub-district (SD) (p<0.001) was seen. The median age was 13 months over the two time periods. Children from Khayelitsha (median age 9.49 months for 2011 and 5.2 months for 2012) were, however, significantly younger than those from other SDs (median age 26.31 months in 2011 and 26.44 months in 2012) (p=0.001). Khayelitsha children were more likely to require admission to a TBH paediatric ward (p<0.001, adjusted odds ratio (aOR) 0.57), while children from other SDs were more likely to be discharged home or transferred to a district hospital (p<0.001, aOR 1.75). Respiratory illnesses accounted for the majority of admissions during both time periods (54% in 2011 and 51% in 2012.
CONCLUSION: Children from Khayelitsha were significantly younger and more likely to be admitted to a TBH inpatient ward compared with other SDs. These findings necessitate a review of current health service resource allocation.
South Africa (SA) has made major progress towards improving the social circumstances of its children since democracy in 1994 with the ratification of the United Nationa (UN) Convention on the Rights of the Child,1 the unconditional inclusion of basic socioeconomic rights for children in the SA Constitution,2 free healthcare for children under 6 years and pregnant women,3 the adoption of the Millennium Developmental Goals4 and the revision of the Child Care Act.5 Yet, SA is one of the few countries globally where under-5 mortality has increased rather than decreased, comparing poorly with other low-and middle-income countries. This increase in mortality has coincided with the HIV/AIDS epidemic, the increase in tuberculosis and weak healthcare systems in certain regions of SA.6 Preventable or treatable diseases such as HIV/AIDS, diarrhoea, lower respiratory infections, malnutrition and perinatal complications account for more than three-quarters of under-5 deaths in SA,7 highlighting the need for the urgent escalation of public health interventions to limit morbidity and mortality in children.8 Malnutrition contributes substantially to the burden of childhood disease as both a direct cause for mortality and as an underlying synergistic factor in other major causes of death such as pneumonia, diarrhoea and HIV/AIDS.9 The Western Cape Province has the lowest under-5 mortality rate in SA, but is one of the most inequitable provinces, with young child mortality varying by a factor of three between the worst and the best areas.10 The dominant pattern of childhood mortality and morbidity, similar to the rest of the country, remains one of nutritional deficiency and communicable diseases.7
In 2003 the Cape Metropolitan Region (Cape Metro) was divided into two districts, namely Metro East and Metro West. Metro East is subdivided further into four sub-districts (SDs): Khayelitsha, Tygerberg, Northern and Eastern, with specific referral pathways from primary to secondary and tertiary care facilities for each SD. Khayelitsha is one of the largest SDs, but it is the poorest.11 It has a young population, with 12% (n=46 773) under-5 years of age in 2011, the highest proportion in Metro East.12,13 It was found to have the highest levels of mortality in all main cause groups of premature mortality in Cape Town,14 with the 2009 reported infant mortality rate of 35/1 000 the highest in Cape Town. The 2010 under-5 mortality rate was 45% higher in Khayelitsha compared with other SDs. A new 230-bed Khayelitsha District Hospital (KDH) was opened in April 2012, providing support to the surrounding primary healthcare facilities to ensure that patients receive care at the lowest level of entry into the healthcare system. A change in the Khayelitsha SD referral pathway was simultaneously implemented. Before, most children requiring acute care were sent directly from primary health clinics to Red Cross War Memorial Children's Hospital (RCWMCH), and a smaller number living east of Spine Road were referred to Karl Bremer Hospital, if they required primary or secondary care. A small number of patients were referred to Tygerberg Hospital Paediatric Emergency and Ambulatory Care Unit owing to incorrect use of referral pathways or during patient diversions, as a result of bed pressure across the Cape Metro. From 2008, a paediatric ward looking after children from Khayelitsha needing level 1 care was opened at Tygerberg Hospital (TBH), but was administered and staffed independently. This was a transition period before the opening of the new hospital. Patients accessed this ward by down-referral from RCWMCH (or TBH should they have been admitted there). All patients requiring more advanced levels of care were to be referred to TBH from April 2012. TBH serves as the primary care referral centre for the Tygerberg SD, and the secondary and tertiary care referral centre for all Metro East SDs. The paediatric ambulatory unit at TBH accepts and manages all patients from primary health clinics, district hospital emergency centres, as well as patients arriving from home. The service includes a 24-bed short-stay ward where patients requiring ongoing observation and treatment due to their medical condition are admitted.15 With the anticipated increase in paediatric referrals to TBH, health service planning calculations identified the need for additional resources. Due to budget constraints, limited resources were added to the TBH service platform.
The aim of this study was to determine the impact of the referral pathway change on the admission profile of children admitted to the TBH short-stay ward, both in terms of patient outcome and service demands; specifically whether Khayelitsha patients had a higher burden of disease compared with children from other SDs.
Methods
The study was conducted in the paediatric ambulatory unit at TBH and was approved by the Stellenbosch University Faculty of Health Sciences Health Research Ethics Committee (N12/06/032). This was a retrospective cohort study, analysing the routine health information as captured in the ward admissions register over two similar seasonal periods: 1 April - 30 September 2011 (prior to the referral pathway change) and 1 April -30 September 2012 (after the referral pathway change). Cases with a surgical diagnosis admitted to surgical wards via the emergency and short-stay ward were excluded. Data collected were entered directly from the ward admission registers into an Excel (Microsoft Corp., USA) spreadsheet. Each patient was given a unique identifier and all identifying variables including patient names, hospital numbers and physical addresses were removed from the data set to ensure anonymity during data analysis. The hospital administrative system was used to find any incomplete data. Readmissions were included in the data collection. The data collected included the demographic data (date of birth, sex and residential suburb), date of admission, diagnosis, date of discharge or inpatient admission, weight, outcome (discharge, admission or death) and International Classification of Diseases (ICD)-10 diagnosis. For the purpose of the study, the following definitions were used:
• Children: all children <18 years of age
• SD: the Cape Metro SD in which the patient resides
• Underweight for age: World Health Organization's weight-for-age z-scores (WAZ) <-2
• Level 1 facility: a district hospital children's ward staffed by a medical officer
• Level 2 facility: a secondary-level ward with general paediatric care on site
• Level 3 facility: a tertiary-level ward with highly specialised paediatric care on site, such as TBH subspecialty wards
• PICU: the paediatric intensive care unit at TBH, or RCWMCH if no space was available at TBH
• Diagnosis: International Classification of Diseases (ICD)-10 coding of disease at discharge, transfer or death. If no discharge diagnosis was entered, the admission diagnosis was used. For simplification, diagnoses were grouped into disease categories according to systems affected such as respiratory, neurological or gastrointestinal
• Length of stay: duration in days from date of admission to date of discharge from the short-stay ward.
Statistical analysis
Data were analysed using STATA version 12 (StataCorp, USA). Comparisons between the two cohorts were based on χ2 statistical tests in the case of categorical outcomes, and Mann-Whitney U-tests in the case of non-parametric numerical outcomes. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated to assess impact. Descriptive statistics were used to analyse diagnoses at discharge, mortality rates, age group burdens, referral rates to secondary and tertiary hospital beds, and length of stay. Multivariate binary logistic regression analysis was used to identify differences between outcomes of children from Khayelitsha SD compared with the other SDs.
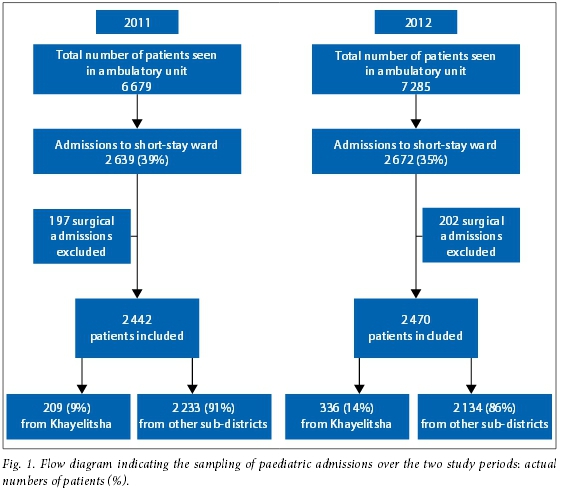
Results
Of the 6 679 and 7 285 patients seen in the ambulatory unit in 2011 and 2012, respectively, 39% (n=2 639) were admitted to the short-stay ward in 2011 compared with 35% (n=2 672) in 2012. A total of 399 surgical admissions were excluded over the two time periods, as complete clinical and outcome data were not available. The remaining total of 4 912 admissions were included for data analysis. Fig. 1 shows the admissions over the two time periods. While numbers for each year remained similar, there was an increase in the number of admissions from Khayelitsha SD in 2012 (p<0.001). The majority of admissions came from the Tygerberg SD: 66% (n=1 625/2 442) in 2011 and 61% (n=1 517/2 470) in 2012. In 2011, 60% (n=1 459/2 442) of children were referred from primary care clinics, and in 2012, 59% (n=1 461/2 470). In 2011, 13% (n=327/2 470) arrived as walk-ins from home, increasing to 12% (n=301/2 470) in 2012. Patterns of referral from each SD are shown in Figs 2 and 3.


Patient characteristics over the two time periods are shown in Table 1. Children admitted to the ward were young, with 48% under 1 year. The median age for all SDs did not change over the two time periods (p=0.084), except for children admitted from Khayelitsha, who were younger in both time periods, with a significant decrease in median age in 2012 (median age 5 months, interquartile range (IQR) 2-23 months) v. 2011 (median age 10 months, IQR 4 -21 months) (p=0.001).

The most common diagnoses were respiratory illnesses, which accounted for approximately half of admissions in both time periods (54% in 2011 and 51% in 2012), followed by gastrointestinal infections, including gastroenteritis (22% in 2011 and 19% in 2012), and neurological conditions, including tuberculous meningitis (12% in 2011 and 17% in 2012). A fifth (20%) of children were underweight for their age. Although the WAZ score for children from Khayelitsha was significantly lower in 2012, at -0.99 (IQR -2.4 - 0.1) compared with 2011 at -0.5 (IQR -2.3 - 0.8) (p=0.029), the proportion of children underweight for age did not significantly change between the two time periods in both Khayelitsha (22% and 24%, p=0.588) and the other SDs (20% and 21%, p=0.574).
Outcomes for the children admitted to the emergency and short-stay wards are shown in Table 2; the majority of children were discharged directly home. However, the number of children requiring admission as an inpatient was significantly higher in 2012 (n=1 008; 41%) compared with 2011 (n=871; 34%) (p<0.001). Admissions to district hospitals increased overall, but this was only significant for SDs other than Khayelitsha (p<0.001). Admissions to TBH significantly increased during the two time periods (n=742 v. n=835; p=0.001), while children being discharged home or transferred to a primary care hospital had decreased (n=1672 v. n=1624; p=0.04). The increase in admissions from Khayelitsha occurred across all levels of care at TBH, but was only significant for highly specialised (tertiary) admissions (p<0.001). Only admissions to the PICU had a significant increase (p=0.04) between the two time periods for the other SDs. There was no change in length of stay between the two time periods or mortality in the emergency and short-stay wards (p=0.064).
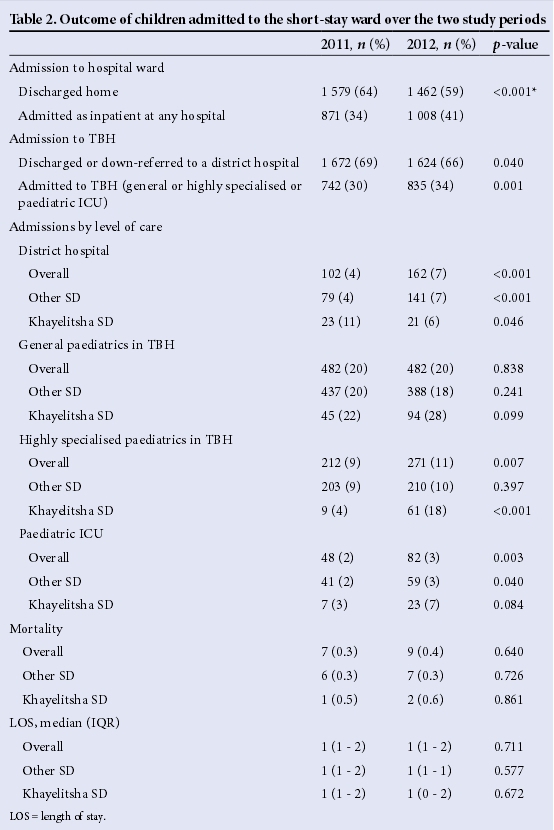
There was no difference between malnutrition and mortality rates across the SDs (Table 2). However, children from Khayelitsha were less likely to be admitted to a district hospital or be discharged from the TBH short-stay ward (p<0.001, OR=0.57) and more likely to be admitted to a TBH ward (general, highly specialised or ICU) (p<0.001, OR=1.75) after adjusting for the differences between 2012 and 2011 (Table 3).

Discussion
Audits have a role in identifying and targeting gaps in the provision of healthcare in terms of coverage, quality and equity.16 Audits are, however, only effective if there is accountability for action, resulting in quality improvement. Although individual healthcare workers play a role in local processes, the availability of human resources, health facility infrastructure, supply systems and shifts in health systems also have a fundamental impact on the quality of healthcare provided at the population level.
During the reporting period in our study, 35% (2012) and 39% (2011) of all attendances to the paediatric ambulatory unit were admitted to the short-stay ward. This is higher than the reported 4 - 10% in studies from developed countries,17,18and may be due to the unit functioning as an emergency referral centre for primary and district hospitals rather than a walkin service. During our study, 13% (2011) and 12% (2012) were walk-ins from home.
Therefore, ~90% of patients had already been assessed by a healthcare provider in the community who thought the acuity or complexity of illness required referral to our unit for further management. The high admission rate may also indirectly reflect the lack of a primary care hospital in the Tygerberg SD, from where the majority of our patients are referred.
The benefit of short-stay wards is that they may reduce the rate of admission to inpatient units, with reduced length of stay in hospital for patients.19,20 Our study, however, reports higher admission rates to inpatient wards from the short-stay ward compared with other units, with our admission rate of 34% (2011) and 39% (2012) higher than the 15 - 25% reported in other studies.15,18,21Similar to other units, respiratory illnesses, gastroenteritis and infectious diseases were the most common diagnoses.21,22 Reported clinical features predicting inpatient admission vary, and include acuity level, age under 3 months, bronchiolitis or other respiratory illnesses requiring oxygen therapy, need for intravenous fluids and medication, and sub-specialty consultation.22,23 The high percentage of young infants seen, the high percentage of respiratory illness, and the higher acuity level of referred patients probably contribute to our unit's higher admission rates. Even though malnutrition accounts for more than 10% of SA's under-5 mortality rate, with 60% of children dying being underweight for age and a third severely malnourished,4 underweight for age in our study, while high, did not increase over the two time periods and there was not a significant difference between Khayelitsha and other SDs. As expected, there was a significant increase in the number of patients being referred from Khayelitsha SD after the change in referral pathways. These children were younger and more likely to be admitted to TBH inpatient wards, compared with children from other SDs, confirming the use of appropriate referral pathways and the higher morbidity described in children from this area, as patients are admitted according to level of care required.14 There was also significant decline in the age of children referred from Khayelitsha between the two time periods. The majority of children were referred from community clinics in 2011, while in 2012 the majority were from the new hospital. This would suggest that older children were effectively managed and treated at the hospital while only the younger and sicker children were referred, thus lowering the median age of children seen at TBH. Our study clearly shows the increasing need for highly specialised and ICU care for children from Metro East. While the number of patients admitted to the short-stay ward has not increased, the level of acuity has, as demonstrated by the increased number of admissions to the highly specialised wards and almost doubling of admissions to the ICU. Of note is that the significant increase of inpatient admissions was seen in both the Khayelitsha and other SD groups. This identifies severity of disease in Metro East as a whole, and a potential need to strengthen the primary, secondary and tertiary healthcare systems in Metro East.
Study limitations
Being a retrospective study, it was reliant on routine, real-time record keeping. This can be incomplete at times, but we were able to capture most incomplete data from the hospital data system. While some data may have been incomplete, the data collection was unlikely to have changed over the 2-year period and thus comparison would be appropriate. Our study started soon after the opening of KDH and change in the referral pathway, when systems and staffing were still in the introductory phase. Therefore, there may have been incorrect referral along the old pathway as well as new inexperienced doctors more likely to refer to a higher level of care. This did not seem the case in our study, as fewer patients were referred back to KDH compared with other primary care facilities. Finally, our study looked at acute admissions only, but did not evaluate direct ward or paediatric ICU admissions. It also did not evaluate bed occupancy rates in these wards, which may have identified additional burden of disease, needing additional resources.
Conclusion
Understanding burden of disease is fundamental to evidence-based health planning. It identifies health needs and allows for monitoring of the implementation of programmes and health services. Although a significant increase in the overall number of patients referred was not identified after the change in referral pathway, an increase in severity of disease with increasing paediatric ICU and highly specialised admissions across all SDs was observed. Children from Khayelitsha were significantly younger and more likely to be admitted to a TBH ward compared with other SDs. These findings necessitate a review of current health service resource allocation.
Sources of funding. This research was supported by the Desmond Tutu TB Centre, Department of Paediatrics, Faculty of Medicine and Health Sciences, Stellenbosch University, South Africa; and funded by the US Agency for International Development (USAID) Cooperative Agreement (TREAT TB - Agreement No. GHN-A-00-800004). The contents are the responsibility of the authors and do not necessarily reflect the views of USAID.
References
1. Goldhagen J. Children's rights and the United Nations Convention on the Rights of the Child. Pediatrics 2003;112(3 Part 2):742-745. [ Links ]
2. Annas GJ. The right to health and the nevirapine case in South Africa. N Engl J Med 2003;348(8):750-754. DOI:10.1056/NEJMlim022737 [ Links ]
3. Wilkinson D, Sach ME, Abdool Karim SS. Examination of attendance patterns before and after introduction of South Africa's policy of free health care for children aged under 6 years and pregnant women. BMJ 1997;314(7085):940-941. DOI:10.1136/bmj.3114.7085.940 [ Links ]
4. Kleinert S, Horton R. South Africa's health: Departing for a better future? Lancet 2009;374(9693):750-760. DOI:10.1016/S0140-6736(09)61306-4 [ Links ]
5. Jamieson L, Lake L. Children's Act Guide for Health Professionals, 2013. 5th ed. Cape Town: Children's Institute, University of Cape Town, 2013. [ Links ]
6. Chopra M, Daviaad E, Pattinson R, Fonn S, Lawn JE. Saving the lives of South Africa's mothers, babies, and children: Can the health system deliver? Lancet 2009;374(9692):835-846. DOI:10.1016/S0149-6736(09)61123-5 [ Links ]
7. Bradshaw D, Bourne D, Nannan N. What are the leading causes of death among South African children? MRC Policy Brief No. 3, December 2003. Burden of Disease. Research Unit, Medical Research Council. http://www.mrc.ac.za/policybriefs/childmortality.pdf (accessed 15 May 2012). [ Links ]
8. Mayosi BM, Lawn JE, van Niekerk A, Bradshaw D, Karim SSA, Coovadia HM. Health in South Africa: Changes and challenges since 2009. Lancet 2012;380(9858):2029-2043. DOI:10.1016/S0140-6736(12)61814-5 [ Links ]
9. Heikens GT, Bunn J, Amadi B, et al. Case management of HIV-infected severely malnourished children: Challenges in the area of highest prevalence. Lancet 2008:371(9620):1305-1307. DOI:10.1016/S0140-6736(08)60565-6 [ Links ]
10. City of Cape Town. http://capetown.gov.za/clusters/health.asp?IDPathString=1123-1374-3256&clusid=245&catparent=3256 (accessed 30 December 2015). [ Links ]
11. City of Cape Town. www.capetown.gov.za/en/stats/2011CensusHealthDistrictProfiles/KhayelitshaHealth District.pdf (accessed 30 December 2015). [ Links ]
12. City of Cape Town. A Population Profile of Khayelitsha: Socio-economicInformation from the 2001 Census. 2005. http://www.capetown.gov.za/en/stats/CityReports/Documents/Population%20Profiles/ A_Population_Profile_of_Khayelitsha_1052006142120_359.pdf (accessed 30 December 2015). [ Links ]
13. Western Cape Provincial Treasury, Local Government Budget Office. Regional Development Profile of City of Cape Town. 2012. https://www.westerncape.gov.za/assets/departments/treasury/dc0_city_of_cape_ town_sep-lg_profile_02_2013.pdf#page=11&zoom=auto,-133,769 (accessed 30 December 2015) [ Links ]
14. Groenewald P, Bradshaw D, Daniels J, et al. Local-level mortality surveillance in resource-limited settings: A case study of Cape Town highlights disparities in health. Bull World Health Organ 2010;88(6):444-451. DOI:10.2471/BLT.09.069435 [ Links ]
15. Crocetti MT, Barone MA, Amin DD, Walker MD. Pediatric observation status beds on an inpatient unit: An integrated care model. Pediatr Emerg Care 2004;20(1):17-21. DOI:10.1097/01.pec.0000106238.72265.5f [ Links ]
16. Kinney MV, Kerber KJ, Black RE, et al. Sub-Saharan Africa's mothers, newborns and children: Where and why do they die? PLoSMed 2010;7(6):e1000294. DOI:10.1371/journal.pmed.1000294 [ Links ]
17. Scribano PV, Wiley JF, Platt K. Use of an observation unit by a pediatric emergency department for common pediatric illnesses. Pediatr Emerg Care 2001;17(5):321-323. DOI:10.1097/00006565-200110000-00001 [ Links ]
18. Levett I, Berry K, Wacogne I. Review of a paediatric emergency department observation unit. Emerg Med J 2006;23(8):612-613. DOI:10.1136/emj.2005.029470 [ Links ]
19. Coon JT, Martin A, Abdul-Rahman A, et al. Interventions to reduce acute paediatric hospital admissions: A systematic review. Arch Dis Child 2012;97(4):304-311. DOI:10.1136/archdischild-2011-301214 [ Links ]
20. Ogilvie D. Hospital based alternatives to acute paediatric admission: A systematic review. Arch Dis Child 2005;90(2):138-142. DOI:10.1136/adc.2003.035543 [ Links ]
21. Macy ML, Kim CS, Sasson C, Lozon MM, Davis MM. Pediatric observation units in the United States: A systematic review. J Hosp Med 2010;5(3):172-182. DOI:10.1002/jhm.592 [ Links ]
22. Xie J, Lin Y, Kissoon N. Factors associated with prolonged stay in a pediatric emergency unit of an urban tertiary children's hospital in China. Pediatr Emerg Care 2013;29(2):183-190. DOI:10.1097/PEC.0b013e3182809b64 [ Links ]
23. Alpern ER, Calello DP, Windreich R, Osterhoudt K, Shaw KN. Utilization, and unexpected hospitalization rates of a pediatric emergency department 23 hour observation unit. Pediatr Emerg Care 2008;24(9):589-594. DOI:10.1097/PEC.0b013e3181850c80 [ Links ]
24. Patrick M, Stephen C, eds. Saving Children 2005: A survey of child healthcare in South Africa. Pretoria: Child PIP group and MRC Unit for Maternal and Infant Health Care Strategies; 2007. MRC Unit for Maternal and Infant Health Care Strategies, 2007. [ Links ]
 Correspondence:
Correspondence:
H Finlayson
finlayson@sun.ac.za














