Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Child Health
On-line version ISSN 1999-7671
Print version ISSN 1994-3032
S. Afr. j. child health vol.9 n.4 Pretoria Nov. 2015
http://dx.doi.org/10.7196/sajch.2015.v9i4.895
REVIEW
Audit of feeding practices in the neonatal wards at the Charlotte Maxeke Johannesburg Academic Hospital
L SepengI; D E BallotII
IMB ChB; Department of Paediatrics and Child Health, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIMB BCh, FCPaed (SA), PhD; Department of Paediatrics and Child Health, Charlotte Maxeke Johannesburg Academic Hospital, Johannesburg, South Africa
ABSTRACT
BACKGROUND: Breastfeeding is the preferred choice of infant feeding. The Baby-Friendly Hospital Initiative (BFHI) is a ten-step plan to help establish successful breastfeeding and is adapted by public sector hospitals in Gauteng. Despite this, rates of breastfeeding in sick and preterm neonates remain low.
OBJECTIVE: To determine feeding practices of neonates in the neonatal wards of the Charlotte Maxeke Johannesburg Academic Hospital (CMJAH) on discharge
METHODS: A retrospective review of the CMJAH neonatal database of feeding choices of neonates discharged from the CMJAH neonatal unit between 1 January 2013 and 30 April 2013 was conducted.
RESULTS: The records of 404 neonates were studied. A total of 98 (24%) were very low birth weight (VLBW) (<1 500 g), while 306 (75.7%) were >1 500 g or more. Only 94 (23.2%) were discharged on exclusive breastmilk, 232 (57.4%) were discharged on exclusive formula milk and 78 (19.3%) babies were discharged on mixed feeds (both formula milk and breastmilk). Significant variables associated with feeding choices were HIV exposure, perinatal asphyxia and resuscitation at birth and, particularly in the VLBW group, necrotising enterocolitis was found to be statistically significant.
CONCLUSION: Despite the fact that the CMJAH was involved in the BFHI, rates of exclusive breastfeeding were still low. This needs to be urgently addressed with employment of lactation consultants and improved counselling of mothers exposed to HIV on the importance and benefits of breastfeeding.
Human milk is uniquely composed to meet the needs of the human infant, and has been established as the 'optimal form' of nutrition for neonates.[1] It contains 0.8 - 0.9% protein, 4.5% fat, 7.15% carbohydrates and 0.2% ash (minerals). There is a high concentration of lactose, which is an excellent source of carbohydrates, and the fat fraction contains specific triglycerides of palmitic and oleic acid (O-P-O triglycerides) and a large quantity of lipids with trans bonds, which are considered to have health benefits. The principal proteins are casein, α-lactalbumin, lactferrin, IgA, lysozyme and serum albumin.[2] Breastfeeding delivers immunological advantages to the infant: bifido and lactobacillus bacteria in the breastfed neonate's gastrointestinal system produces lactate and acetate, which lowers pH. The low pH and other substances excreted by these bacteria inhibit the growth of some Gram-positive and Gram-negative bacteria. Bacteria found in breastmilk also detoxify ammonia and other amines; they activate the immune system and thus help fight bacteria that cause disease. Breastfeeding is a significant protector against diarrhoeal disease, respiratory disease and other infections. It tends to result in better nutritional outcomes, including protecting against obesity in overfed populations and against wasting in underfed populations. It has beneficial effects on cognitive functioning and psychosocial development.[2] Breastfeeding has also been shown to reduce the incidence of necrotising enterocolitis (NEC) in preterm infants.[1]
The Baby-Friendly Hospital Initiative[3] (BFHI) is a 10-step plan to help establish successful breastfeeding, and has been adapted by public sector hospitals in Gauteng. Despite this, rates of breastfeeding in the neonatal unit at the Charlotte Maxeke Johannesburg Academic Hospital (CMJAH) are unacceptably low. Possible reasons for this may include reluctance among the staff to promote breastfeeding to HIV-positive mothers, lack of dedicated lactation counsellors and a lack of facilities for breastfeeding mothers to live in the hospital.
A number of studies have been done on infant feeding in South Africa (SA), the majority conducted in the KwaZulu-Natal (KZN)[4-9] and Western Cape[10-11] provinces. In the Gauteng province,[11] the study on feeding was done with relation to prevention of mother-to-child transmission (PMTCT) in the preterm infant.
Several studies in KZN have looked at the beneficial effects of human milk on decreasing rates of paediatric infections such as NEC and sepsis.[4-8] The objective was to look at the feasibility of providing donor breastmilk to neonates in a resource-limited neonatal premature unit. It was found that staff attitudes influenced the uptake of donor breastmilk.[4,6,7] Studies in HIV-positive mothers showed that those neonates who were exclusively breastfed showed significantly lower rates of diarrhoeal diseases and had lower rates of hospitalisation. In addition, there was an association with better developmental scores and growth parameters during long-term follow-up, and mothers who exclusively breastfed had lower rates of postnatal depression.[8]
In the Western Cape, Goga et al.[9,10]conducted a prospective observation study between HIV-exposed neonates and unexposed neonates between the ages of 6 and 9 months. They concluded that HIV-positive mothers were more diligent with good feeding practices and this was mainly owing to good PMTCT counselling sites, emphasising the importance of the presence of an encouraging health worker.
Goga et al.[10] also looked at three districts that were part of a trial and which reflected different socioeconomic conditions: rural-urban prevalence and HIV prevalence rates were considered. They found that there were still barriers to exclusive breastfeeding and that measures should be put into place to reduce or even break these barriers.
The objective of the current study was to audit feeding choices in babies discharged from the neonatal unit at CMJAH.
Methods
The CMJAH neonatal unit prospectively collects information upon discharge of neonates for clinical audit. The data are entered into a database managed by Research Electronic Data Capture (REDCAP), hosted by the University of the Witwatersrand.[12] The current study is a review of the neonatal database. Babies who had been admitted to the CMJAH neonatal unit within 72 hours of birth and who were discharged from hospital between 1 January and 30 April 2014 were enrolled; those who died or were transferred to other hospitals were excluded.
Babies who were admitted to the neonatal intensive care unit (NICU) were excluded from the study as these were the sickest neonates and this may have negatively affected mothers' ability to establish breastfeeding. There was no sleep-in facility available for breastfeeding mothers with sick newborn or preterm neonates.
The only such facility was the Kangaroo Mother Care (KMC) unit, which has 15 beds, where mothers of preterm neonates approaching discharge could do continuous KMC. Mothers were counselled as to the benefits of breastfeeding by attending staff, but formula milk was provided to those neonates whose mothers chose not to breastfeed.
There was no donor breastmilk available and no dedicated lactation counsellors in the neonatal ward during the study period. The variables found to be statistically significant were defined as follows: resuscitation - all neonates who received bag-mask ventilation, chest compressions, resuscitative drugs or intubation; and NEC - Bell stages 2 and 3.
Statistical analysis
Data were described using standard statistical methods using SPSS version 21 (IBM, USA). Continuous variables were normally distributed, so mean and standard deviation (SD) were used as measures of central tendency. Categorical data were described using frequencies and percentages.
Babies were divided into groups according to feeding choice: breastmilk only; formula milk only; or mixed feeds. They were also grouped by birth weight: <1 500 g and >1 500 g. These groups (feeding choice and birth weight) were compared using χ2 analysis for categorical variables and unpaired tests for continuous variables. Logistic regression was also done using the method of feeds as the multinomial variable against the various demographic and clinical characteristics as input variables. Those variables with a p-value <0.1 on univariate analysis were included.
If the infant required non-invasive ventilation by means of continuous positive airway pressure, the date of initiation and date of being weaned off were recorded, as during this time initiation of feeds would be delayed. Variables which were similar in nature were grouped together to facilitate analysis (e.g. hyaline membrane disease and transient tachypnoea of the newborn were classified as respiratory illness).
Results
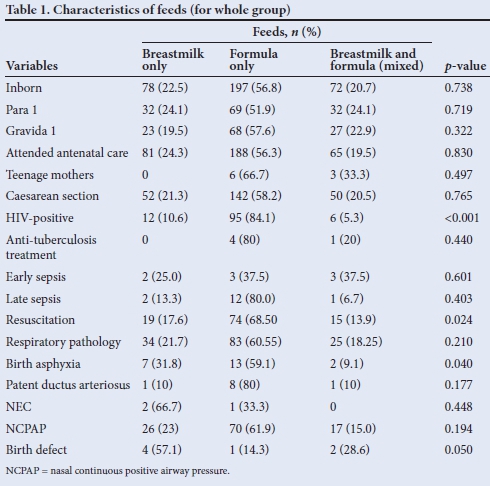
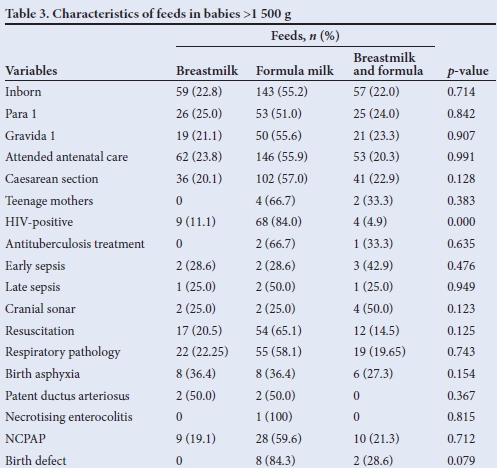
A total of 404 neonates were enrolled. Out of the group, 197 (48.8%) were female and 207 (51.2%) were male. The mean birth weight was 3 372 g. Of the 404 infants studied, 98 (24.0%) were very low birth weight (VLBW) and 306 (75.7%) were >1 500 g at birth. Only 94/404 (23.2%) of the total group were discharged on exclusive breastmilk, 78 (19.3%) were discharged on mixed feeding (both formula and breastmilk) and 232 (57.4%) neonates were discharged on exclusive formula milk. Various factors postulated to affect feeding choice are compared in Table 1. Significant factors found were HIV-exposed neonates, neonates who had birth asphyxia post delivery and required resuscitation, and in the VLBW group, NEC was also found to be statistically significant (Table 2).

Discussion
Breastfeeding rates in the CMJAH neonatal unit remain unacceptably low: 42.5% of all babies discharged from the unit received breastmilk, but only 23.2% of neonates were discharged on exclusive breastmilk. Irrespective of birth weight, the preferred method of feed was still formula feeds (57.4%).
The most significant factors associated with feeding choice in the whole group were: birth asphyxia (p<0.040), maternal HIV status (p<0.001) and resuscitation (p<0.024). In the VLBW group, NEC was found be significant (p<0.024). It is surprising that the lack of breastfeeding was not different between VLBW and bigger neonates (Table 3), as establishing breastfeeding in sick preterm neonates is more challenging than in bigger, healthier neonates.
The reasons for the very low rate of breastfeeding were not evaluated in the present study, but may relate to the fact that there was no dedicated lactation counsellor assigned to the neonatal ward and no donor breastmilk available during the study period. Establishing breastfeeding in sick and preterm neonates in a busy, understaffed neonatal unit is more effort than formula feeding, and adequate support in terms of education, dedicated staff and donor breastmilk is essential. There was also no sleep-in facility for breastfeeding mothers with sick neonates. Many of the mothers live far away and transport is expensive.
CMJAH is a tertiary obstetric referral centre and many of the mothers are ill at the time of delivery. The majority of babies requiring admission are delivered by emergency caesarean section, most often owing to pregnancy-induced hypertension. Establishing breastfeeding is more difficult in these circumstances.
It is more challenging to latch a newborn within an hour of birth and discuss feeding choices with an ill mother. The strong association with maternal HIV exposure and lack of breastfeeding may reflect reluctance on the part of health workers to promote breast-feeding in HIV-infected mothers. It may also reflect a lag in implementing a change in the feeding policy (HIV-infected mothers were provided with formula in Gauteng until early 2012). Ongoing education and training of health workers in the BFHI and provincial feeding policies is crucial.
Study limitations
This was a retrospective study confined to evaluating the type of feeding on discharge from the CMJAH neonatal unit. Feeding choice is a complex, multifactorial issue, and many of the possible factors involved could not be investigated (as outlined above). A prospective study including various staff and maternal factors that influence feeding choice should be conducted in the unit, therefore further prospective research study is needed.
Conclusion
Despite the fact that CMJAH is involved in the BFHI, the rates of exclusive breastfeeding were still low. Reasons for this were not studied but could include inadequate education of healthcare workers, lack of lactation counsellors, maternal illness, lack of sleep-in facilities and no donor breastmilk. Maternal factors, including previous breast-feeding experience, socioeconomic status, attendance at antenatal clinics and level of education, would also influence feeding choices, but these were beyond the scope of this study. Establishing breastfeeding in sick neonates requires a team approach with dedicated counsellors and ongoing training of healthcare workers.
References
1. Kuhn L, Aldrovandi G. Survival and health benefits versus artificial feeding in neonates of HIV-infected women: Developing versus developed world. Clin Perinatol 2010;37(4):843-862. [http://dx.doi.org/10.1016/j.clp.2010.08.011] [ Links ]
2. Precht D, Molkentin J. C18:1, C18:2 and C8:3 trans and cis fatty acid isomers including conjugated cis delta 9, trans delta 11 linoleic acid (CLA) as well as total fat composition of German human milk lipids. Nahrung 1999;43(4):233-244. [http://dx.doi.org/10.1002/(SICI)1521-3803(19990801)43:4lt;233::AID-FOOD233>3.0.CO;2-B] [ Links ]
3. Merewood A, Phillip BL, Chawla N, Cimo S. The Baby-Friendly Hospital Initiative increases breastfeeding rates in a US neonatal intensive care unit. J Hum Lact 2003;19(2):166-171. [ Links ]
4. Coutscoudis I, Adhikari M, Nair N, Coutscoudis A. Feasibility and safety of setting up a donor breastmilk bank in a neonatal prem unit in a resource limited setting: An observational, longitudinal cohort study. BMC Public Health 2011;11:356. [http://dx.doi.org/10.1186/1471-2458-11-356] [ Links ]
5. Coutscoudis I, Petrites A, Coutscoudis A. Acceptability of donated breastmilk in a resource limited South Africa setting. Int Breastfeed J 2011;6:3-4358-6-3. [http://dx.doi.org/10.1186/1746-4358-6-3] [ Links ]
6. Bland RM, Little KE, Coovadia HM, Coutscoudis A, Rollins NC, Newell ML. Intervention to promote exclusive breast-feeding for the first 6 months of life in a high HIV prevalence area. AIDS 2008;22(7):883-891. [http://dx.doi.org/10.1097/QAD.0b013e3282f768de] [ Links ]
7. Bobat R, Moodley D, Coutscoudis A, Coovadia HM. Breastfeeding by HIV-1-infected women and outcome in their neonates: A cohort study from Durban, South Africa. AIDS 1997;11(13):1627-1633. [ Links ]
8. Kindra G, Coutscoudis A, Esposito F, Esterhuzen T. Breastfeeding in HIV exposed neonates significantly improves child health: A prospective study. Matern Child Health J 2012;16(3):632-640. [http://dx.doi.org/10.1007/s10995-011-0795-8] [ Links ]
9. Goga AE, van Wyk B, Doherty T, et al. Infant feeding practices at routine PMTCT sites, South Africa: Results of a prospective observational study amongst HIV exposed and unexposed neonates: Birth to 9 months. Int Breastfeed J 2012;7:4. [http://dx.doi.org/10.1186/1746-4358-7-4] [ Links ]
10. Goga AE, van Wyk B, Doherty T, et al. Operational effectiveness of guidelines on complete breast-feeding cessation to reduce mother-to-child transmission of HIV: Results from a prospective observational cohort study at routine prevention of mother-to-child transmission sites, South Africa. J Acquir Immune Defic Syndr 2009;50(5):521-528. [ Links ]
11. Saloojee H, Cooper PA. Feeding of infants of HIV-positive mothers. Curr Opin Clin Nutr Metab Care 2010;13(3):336-343. '[http://dx.doi.org/10.1097/MCO.0b013e328337321a] [ Links ]
12. Harris PA, Taylor R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap): A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2008;42(2):377-381. [http://dx.doi.org/10.1016/j.jbi.2008.08.010] [ Links ]
 Correspondence:
Correspondence:
L Sepeng
mntungwasazy@gmail.com














