Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Child Health
versão On-line ISSN 1999-7671
versão impressa ISSN 1994-3032
S. Afr. j. child health vol.9 no.2 Pretoria Jan./Abr. 2015
http://dx.doi.org/10.7196/SAJCH.869
OPINION
Apartheid and healthcare access for paediatric systemic lupus erythematosus patients in South Africa
L B LewandowskiI; C ScottII
IMD; Duke University Medical Center, Duke Global Health Institute, Pediatric Rheumatology, Global Health, Durham, USA
IIMB ChB, FCPaed; Head of Paediatric Rheumatology, Red Cross War Memorial Children's Hospital, University of Cape Town, South Africa
South Africa (SA) still faces the legacy of apartheid: the history, politics and economics have a lasting, indelible effect on the health of its people. Here, we discuss the challenges of caring for patients with chronic disease, focusing on paediatric systemic lupus erythematosus (SLE), as a framework for evaluating the structural challenges to accessing care in SA. Prior reports have demonstrated numerous factors influencing access for SA patients with chronic disease.[1] This article explores the economic, social and political vestiges of apartheid as it affects the healthcare system and subsequently, our patients.
SLE is a life-threatening autoimmune disease, which we will use to highlight the challenges of identifying and treating chronic diseases in SA. Paediatric SLE (pSLE) is more severe than the adult disease, and children with SLE in Africa are potentially at high risk for poor outcomes based on race and age.[2-4] We have initiated a study of the pSLE population in SA. Over half of the cohort presented with severe manifestations, such as renal failure or stroke, at time of diagnosis, leading to serious and irreversible organ damage in many of our patients. We propose that postapartheid and related economic obstacles may delay the diagnosis of pSLE and other chronic diseases, leading to advanced disease burden and poor outcomes.
Access to care in SA is a complex outcome with many facets. This analysis borrows a model from the world of economics: the theory of transaction costs used to explain market failures.[5] The transaction cost of travel (including risk of travel, time and expense) often creates a barrier to market participation. Utilising this theory of transaction costs, we describe the personal and economic pressures that drive medical access decisions in postapartheid SA. Through this model, we will attempt to understand the factors that limit access to care.
SA is a low-to-middle-income country, yet the income disparities are vast. The Gini coefficient (a measure of income inequality ranging from 0 to 1) grew in postapartheid SA from 0.56 in 1995 to 0.76 in 2005, although it did decrease slightly to 0.7 in the most recent report.[6,7] Other studies have highlighted the effects of poverty on health, and the detrimental effects of income disparity on the health of SA.[8] During apartheid, laws and policies were put in place that targeted the marginalisation of black African and coloured people.*[6,9] Through a series of legislative acts, including pass laws and the Land Act, black African families were relocated to rural areas.[10] The infrastructure of roads and these laws combined to limit access and mobility for people of colour. This has led to a fragmentation of land, services and access, often according to racial and socioeconomic status. The vestiges of that system have continued consequences for the poor of those areas today.[11]
Previous studies have linked the length of travel time and access to care. Limited availability of ambulances creates a travel barrier, as emergency care may be unable or unwilling to enter informal settlements. Roads and addresses in these areas can be poorly marked or nonexistent. Maternity studies highlight this problem:
most women who delivered outside of a facility did so while waiting for emergency transport. Interviews revealed that ambulances can or will not attempt to enter their settlements.[12] A study of patients with chronic disease revealed that ambulance disrepair and poor staff availability are also causes for lack of emergency transport options.[1] There is no reliable system of centralised public transportation in SA. Public transportation safety is a serious concern.[13] One study revealed that 64% of South Africans were dissatisfied with personal security on the walk to train stations and on the trains themselves.[14] In 2011, there were over 5 000 deaths in SA from traffic accidents.[15] Minibus taxi users were the most unsatisfied about safety from accidents (67%), lack of facilities (64%), and lack of vehicle roadworthiness (60%).[16] Poor people living in rural areas are least likely to have access to a private car, yet may not have emergency vehicle or public transport options available in times of illness.
Cost for transport further compounds this matter. Minibus taxis are expensive relative to income and are not subsidised by the state. In almost half of the poorest households (monthly income <ZAR500, ~USD50 equivalent), it is shown that members spend more than 20% of their income on public transportation at baseline.[15]
In addition to fees, time is often an underappreciated cost. In one study, if transportation time exceeded 1 hour, there was a marked decline in a patient's likelihood to seek care.[12] Travel time is often underestimated, as many roadmaps are inaccurate, and variations in the rainy season and other hindrances can turn a 5-km walk into a 10-hour trip. Studies have shown that in SA, the average wait time in clinics is 150 - 160 minutes.[12,17] This time is additive with the travel time to the clinic.
A final invisible cost to consider is job security. SA has a high number of migrant workers and day labourers. The time spent waiting for transport and care can translate into a day of missed work. Without job security, this may mean loss of livelihood. Current estimates of the unemployment rate are 27%,[14] therefore a lost job is unlikely to be restored.
Transportation cost may be a more prominent obstacle in seeking healthcare for initial symptoms of chronic conditions. These first, milder symptoms can continue unchecked until they develop into an emergency.[18] When patients present with advanced disease, it may have caused irreversible damage, leading to anger and frustration. This can result in a cycle of distrust between the patient and providers (Fig. 1).
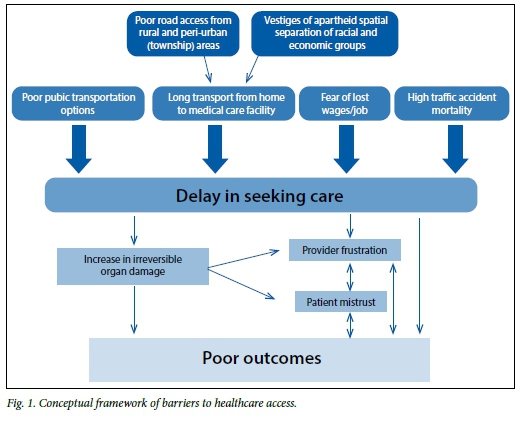
Reflecting on all the major costs listed above, it is remarkable that families under these circumstances ever access healthcare. In our study, the majority of children have severe damage, such as blindness or renal failure. We recognise that the costs of transportation, both visible and unseen, may be just one component of delay in care. Based on the evidence presented in this article, it seems likely that the cost of transport will prove to create a barrier to care, and addressing this impediment could improve the care of chronic disease in SA.
*Note: All categories of race described in this article are utilised according the scheme used by Statistics SA, and include the following groups: black African, coloured, Indian/ Asian, white and other.
Acknowledgements. This work was funded by Duke Immunology/Rheumatology under T32 Training grant award number 3020466 and the Fogarty International Center of the National Institute of Health under award number R25TW009337. This study was approved by the University of Cape Town ethics committee and the Duke University Institutional review board. We would like to acknowledge Dr N Thielman for thoughtful manuscript review.
References
1. Goudge J, Gilson L, Russell S, Gumede T, Mills A. Affordability, availability and acceptability barriers to health care for the chronically ill: Longitudinal case studies from South Africa. BMC Health Serv Res 2009;9:75. [http://dx.doi.org/10.1186/1472-6963-9-75] [ Links ]
2. Brunner HI, Gladman DD, Ibanez D, Urowitz MD, Silverman ED. Difference in disease features between childhood-onset and adult-onset systemic lupus erythematosus. Arthritis Rheum 2008;58(2):556-562. [http://dx.doi.org/10.1002/art.23204] [ Links ]
3. Ardoin SP, Schanberg LE. Paediatric rheumatic disease: Lessons from SLE: Children are not little adults. Nat Rev Rheumatol 2012;8(8):444-445. [http://dx.doi.org/10.1038/nrrheum.2012.109] [ Links ]
4. Uribe AG, McGwin G Jr, Reveille JD, Alarcón GS. What have we learned from a 10-year experience with the LUMINA (Lupus in Minorities; Nature vs. nurture) cohort? Where are we heading? Autoimmun Rev 2004;3(4):321-329. [http://dx.doi.org/10.1016/j.autrev.2003.11.005] [ Links ]
5. De Janvry A, Fafchamps M, Sadoulet E. Peasant household behaviour with missing markets: Some paradoxes explained. Econ J 1991;101(409):1400-1417. [ Links ]
6. Coovadia H, Jewkes R, Barron P, Sanders D, McIntyre D. The health and health system of South Africa: Historical roots of current public health challenges. Lancet 2009;5;374(9692):817-834. [http://dx.doi.org/10.1016/S0140-6736(09)60951-X] [ Links ]
7. Statistics South Africa. Living conditions of households in South Africa, 2008/2009. http://beta2.statssa.gov.za/?page_id=739&id=1(accessed October 2014). [ Links ]
8. Mayosi BM, Benatar SR. Health and health care in South Africa: 20 years after Mandela. N Engl J Med 2014;371(14):1344-1353. [http://dx.doi.org/10.1056/NEJMsr1405012] [ Links ]
9. Posel D. Race as common sense: Racial classification in twentieth-century South Africa. Afr Stud Rev 2001;44(2):87-113. [ Links ]
10. Marks S, Andersson N. Issues in the political economy of health in Southern Africa. J South Afr Stud 1987;13(2):177-186. [http://dx.doi.org/10.1080/03057078708708140] [ Links ]
11. Mayosi BM, Lawn JE, van Niekerk A, Bradshaw D, Abdool Karim SS, Coovadia HM. Health in South Africa: Changes and challenges since 2009. Lancet 2012;380(9858):2029-2043. [http://dx.doi.org/10.1016/S0140-6736(12)61814-5] [ Links ]
12. Silal S, Penn-Kekana L, Harris B, Birch S, McIntyre D. Exploring inequalities in access to and use of maternal health services in South Africa. BMC Health Serv Res 2012;12(1):120. [http://dx.doi.org/10.1186/1472-6963-12-120] [ Links ]
13. Czeglédy AP. Getting around town: Transportation and the built environment in post-apartheid South Africa. City Soc 2004;16(2):63-92. [http://dx.doi.org/10.1525/city.2004.16.2.63] [ Links ]
14. Walters J. Overview of public transport policy developments in South Africa. Res Transportation Economics 2008;22(1):98-108. [http://dx.doi.org/10.1016/j.retrec.2012.05.021] [ Links ]
15. Statistics South Africa. P0309.3: Mortality and causes of death in South Africa, 2011: Findings from death notification. http://beta2.statssa.gov.za/publications/P03093/P030932011.pdf (accessed October 2014). [ Links ]
16. Meel BL. Trends in fatal motor vehicle accidents in Transkei region of South Africa. Med Sci Law 2007;47(1):64-68. [ Links ]
17. Tanser F, Gijsbertsen B, Herbst K. Modelling and understanding primary health care accessibility and utilisation in rural South Africa: An exploration using a geographical information system. Soc Sci Med 2006;63(3):691-705. [http://dx.doi.org/10.1016/j.socscimed.2006.01.015] [ Links ]
18. Goudge J, Gilson L, Russell S, Gumede T, Mills A. The household costs of health care in rural South Africa with free public primary care and hospital exemptions for the poor. Trop Med Int Health 2009;14(4):458-467. [http://dx.doi.org/10.1111/j.1365-3156.2009.02256.x] [ Links ]
 Correspondence:
Correspondence:
L B Lewandowski
laura.lewandowski@dm.duke.edu














