Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Child Health
versão On-line ISSN 1999-7671
versão impressa ISSN 1994-3032
S. Afr. j. child health vol.9 no.1 Pretoria Jan. 2015
CASE REPORT
Acute fulminant myocarditis complicated by complete atrioventricular block with favourable outcome in a resource-limited setting
Q MerchantI; B S HasanII; S AkhtarIII
IMBBS; Department of Pediatrics and Child Health, Aga Khan University, Karachi, Pakistan
IIMD, FAAP; Department of Pediatrics and Child Health, Aga Khan University, Karachi, Pakistan
IIIMBBS, FCPS (Paed), FCPS; Department of Pediatrics and Child Health, Aga Khan University, Karachi, Pakistan
ABSTRACT
Complete heart block in paediatric acute fulminant myocarditis (AFM) is rare and carries a grave prognosis. Aggressive haemodynamic support, especially mechanical support, i.e. with an extracorporeal membrane oxygenator during the initial presentation, improves the outcome in such patients. Unavailability of mechanical support in developing countries warrants aggressive rhythm management to achieve haemodynamic stability. We report a case of a 5-month-old who presented with AFM complicated with complete heart block. Quick recognition, aggressive cardiopulmonary management and transcatheter placement of a temporary pacemaker as soon as possible resulted in complete recovery in this patient. Aggressive management with rhythm control can lead to a favourable outcome in paediatric patients with AFM complicated by complete heart block, even in a resource-limited set-up.
Myocarditis has an estimated incidence of 10 in 100 000 and is the most common acquired cause of cardiac failure requiring heart transplant in children.[1,2] Viruses form the main aetiological basis, with Coxsackie B virus being responsible for the majority of viral myocarditis cases.[2] The clinical presentation of myocarditis varies from mild fever, flu-like symptoms and malaise to complete cardiovascular collapse, being acute fulminant myocarditis (AFM).[3] AFM is characterised by sudden onset of severe and extensive haemodynamic compromise.[4] Complete atrioventricular heart block (CAVB) is a rare complication of myocarditis and contributes to further haemodynamic compromise.[5] Although more dramatic in its presentation, if it is managed aggressively with mechanical circulatory support, affected patients may have full recovery and less risk of developing dilated cardiomyopathy.[4] In a limited-resource setting where mechanical cardiac support is not available, immediate recognition, management and rhythm control may be the only hope for a favourable outcome.
This case report presents a 5-month-old boy with AFM complicated with CAVB and cardiogenic shock to emphasise the value of early recognition of the disease and the associated rhythm disturbances, timely interventions and aggressive protocol-based management.
Case report
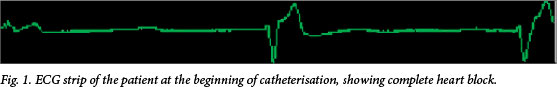
A 5-month-old, previously healthy male presented to the emergency room (ER) of a tertiary care hospital with a 5-day history of high-grade, intermittent fever with associated cough and decreased appetite. He had developed significant respiratory distress 12 - 14 hours prior to his arrival at the ER. The child appeared drowsy and pale, with mottled, cool, clammy skin. Moreover, he was in acute respiratory distress. He was afebrile (36.8°C) but was found to be hypotensive, tachypneic and bradycardic (40 beats per minute (bpm)). His peripheral pulses were irregular and feeble, while peripheral perfusion was poor (>3 s). Abdominal examination revealed a palpable liver edge, 4 - 5 cm below the costal margin. The 12-lead electrocardiogram (ECG) findings were consistent with CAVB. Emergent echocardiogram (ECHO) revealed a structurally normal heart, but with moderate to severe biventricular systolic dysfunction with an ejection fraction of 30%. Initial laboratory work-up revealed raised troponin I levels of 44.5 ng/ mL. Serum electrolytes showed serum creatinine 0.8 mg/dL, blood urea nitrogen (BUN) 31 mg/dL, bicarbonate 15.8 mmol/L, serum glutamic pyruvic transaminase 2 695 IU/L, serum glutamic oxaloacetic transaminase 7 559 IU/L and serum creatine phosphokinase 1 967 IU/L. Provisional diagnosis was AFM with cardiogenic shock. He was started on aggressive supportive therapy with fluids, oxygen and inotropes. Owing to CAVB and haemodynamic instability, emergent temporary pacemaker insertion was planned. A catheterisation laboratory was available and thus intravenous (IV) pacemaker insertion was planned rather than transcutaneous pacing. While in the ER, the patient went into asystole. Immediate cardiopulmonary resuscitation was initiated and the patient revived in 4 - 5 minutes. He was immediately rushed to the catheterisation laboratory where the temporary transvenous pacing catheter was inserted into the right ventricle at midseptal level (pacing rate: 120 bpm; output: 1 mA; sensitivity: 2; mode: Demand). The ECG at the beginning of catheterisation is shown in Fig. 1. ER presentation to pacemaker placement time ('door to pacemaker' time) was <60 minutes. After the successful procedure, he was moved to the cardiac intensive care unit (CICU). Over the course of his CICU admission, he had persistent hypotension, which was adequately managed by inotropic support with dopamine and milrinone. Treatment with IV immunoglobulin (IVIG) and methyl prednisolone (for inotrope resistant shock) was initiated.
The patient did not develop any subsequent rhythm disturbances and no changes were made to the pacemaker setting over the course of his CICU stay. There was a pacer check every day to see if the patient returned back to sinus rhythm (>80 bpm). According to the CICU treatment protocol and based on the patient's clinical status and haemodynamic stability, support was weaned accordingly (the patient was extubated before pacemaker removal and the inotropes were subsequently weaned off as tolerated by the patient). Intermittent and eventually sustained atrioventricular conduction returned on the 4th day after admission. The convalescent rhythm was sinus with heart rate at 139 bpm (Fig. 2). Following the improvement in his clinical and cardiac functioning status, the child was finally extubated on the 6th day after admission. IV inotropic support was gradually weaned and the transvenous pacemaker was removed on 7th day after admission. The child gradually improved and the subsequent echocardiograms done on the 8th day after admission showed normal biventricular function with an improved ejection fraction of 70%. The patient was eventually discharged on the 12th day after admission. At latest follow-up he had made a full recovery. An extensive work-up to determine the etiology of myocarditis could not be done owing to financial constraints. The mother of the patient was not screened for subclinical lupus.

Discussion
AFM complicated by CAVB carries a grave prognosis if not managed aggressively. Early recognition, rhythm control and institution of mechanical cardiac support improves the outcome.[6] Unfortunately, owing to financial constraints and dearth of resources in the developing world, mechanical circulatory devices are not available to be used in all cases of AFM. However, as shown by this case report, aggressive protocol-based management including adequate inotropic support, ventilation and respiratory support, and timely interventions such as pacemaker insertion, can bear satisfactory results and be lifesaving (Fig. 3).
It is important to understand that CAVB in myocarditis, though dramatic in presentation, has the potential for full recovery the majority of the time. A systematic review identified a total of 40 patients <20 years of age.[5] Of these, 27 (67%) returned to atrioventricular conduction within 7 days of admission, 11 (28%) required permanent pacing owing to persistent atrioventricular blockage, while 2 (5%) passed away. Similarly, Chien et al.[7] identified 9 children with AFM complicated with CAVB, of whom 6 regained normal sinus rhythm, 2 developed persistent CAVB, 1 received permanent pacemaker implantation and 1 died due to persistent low cardiac output and ventricular tachycardia (VT). Our case demonstrated complete recovery by the 8th day after admission.
Early recognition of CAVB rhythm in children with AFM and timely intervention with prompt pacemaker insertion is crucial in these instances, and can be lifesaving as demonstrated by this case report. Any delay in the treatment can lead to further complications such as VT and irreversible cardiogenic shock. The literature has reported deaths in cases of myocarditis complicated with CAVB attributed to ventricular arrest.[8] Short periods of VT remain a possibility even after pacemaker insertion, and the risk is greatest during the first 2 days after pacemaker insertion. Thus, careful close monitoring and immediate treatment is recommended, as VT can lead to severe haemodynamic compromise. Periods of VT can be a marker of ongoing or exacerbated myocardial damage and should be aggressively treated to avoid death.[9]
A protocol-driven management of such patients can help to streamline care with the intention of improving the outcome. The crux of these protocols should be early recognition and timely (hour-by-hour) management as done in patients presenting with septic shock. Eventually, a decreased cardiac output despite pacemaker insertion and the need for excessive inotropic support is a sign of a poor prognosis. In such instances, early establishment of extracorporeal membrane oxygenation to optimise cardiac output gives the best chance of survival, which unfortunately is not available in limited-resource settings.[8]
In conclusion, outcome can be improved with early recognition and aggressive management of CAVB in patients with myocarditis. Protocol-based management in the ER can significantly improve the outcomes for these patients (Fig. 4).
References
1. Stiller B. Management of myocarditis in children: The current situation. Adv Exp Med Biol 2008;609:196-215. [http://dx.doi.org/10.1007/978-0-387-73960-1_15] [ Links ]
2. Dancea AB. Myocarditis in infants and children: A review for the paediatrician. Paediatr Child Health 2001; 6(8):543-545. [ Links ]
3. Amabile N, Fraisse A, Bouvenot J, Chetaille P, Ovaert C. Outcome of acute fulminant myocarditis in children. Heart 2006;92(9):1269-1273. [http://dx.doi.org/10.1136/hrt.2005.078402] [ Links ]
4. McCarthy RE, Boehmer JP, Hruban RH, et al. Long-term outcome of fulminant myocarditis as compared with acute (nonfulminant) myocarditis. N Engl J Med 2000;342(10):690-695. [http://dx.doi.org/10.1056/NEJM200003093421003] [ Links ]
5. Batra AS, Epstein D, Silka MJ. The clinical course of acquired complete heart block in children with acute myocarditis. Pediatr Cardiol 2003;24(5):495-497. [http://dx.doi.org/10.1007/s00246-002-0402-2] [ Links ]
6. Heitink-Pollé KM, Rammeloo L, Hruda J, Plötz FB. Rapid and full recovery after life-threatening complete atrioventricular block: An isolated feature of myocarditis? Eur J Pediatr 2004;163(7):410-411. [http://dx.doi.org/10.1007/s00431-004-1455-4] [ Links ]
7. Chien SJ, Liang CD, Lin IC, Lin YJ, Huang CF. Myocarditis complicated by complete atrioventricular block: Nine years' experience in a medical center. Pediatr Neonatol 2008;49(6):218-222. [http://dx.doi.org/10.1016/S1875-9572(09)60014-0] [ Links ]
8. Duncan BW, Bohn Dj, Atz AM, French JW, Laussen PC, Wessel DL. Mechanical circulatory support for the treatment of children with acute fulminant myocarditis. J Thorac Cardiovasc Surg 2001;122(3):440-448.[http://dx.doi.org/10.1067/mtc.2001.115243] [ Links ]
9. Kato S, Morimoto S, Hiramitsu S, et al. Risk factors for patients developing a fulminant course with acute myocarditis. Circ J 2004;68(8):734-739. [ Links ]
 Correspondence:
Correspondence:
S Akhtar
saleem.sadqani@aku.edu














