Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Child Health
On-line version ISSN 1999-7671
Print version ISSN 1994-3032
S. Afr. j. child health vol.9 n.1 Pretoria Jan. 2015
SHORT REPORT
Adherence to phototherapy guidelines in term neonates: Study at a private tertiary-level neonatal unit
T EkramI; B SinghII; D KumarII; S K MittalII; S KumariII
IMD; School of Medical Science and Research, and Sharda Hospital, Sharda University, Greater Noida, Uttar Pradesh, India
IIMD; Department of Paediatrics, Pusphanjali Crosslay Hospital, Ghaziabad, Uttar Pradesh, India
ABSTRACT
Guidelines for starting phototherapy for neonatal jaundice in term neonates have been published by the American Academy of Pediatrics (AAP) and others, such as the National Institute for Health and Clinical Excellence (NICE), but the practical implementation of such guidelines and factors associated with possible non-adherence have not been studied. We report our experience at a self-paying tertiary-care hospital. Of the 155 term babies given phototherapy in our hospital between August 2012 and August 2013, 65 (41.9%) babies were found to have received phototherapy at serum bilirubin values lower than recommended AAP guidelines. Factors found responsible for non-adherence to guidelines were: (i) parents' request for early discharge, with unwillingness to come the next day for follow-up despite borderline serum bilirubin level noted in 25 (38.5%); (ii) clinical assessment of bilirubin was higher than reported laboratory value in 16 (24.6%); and (iii) babies were given phototherapy as parents had been counselled regarding the need for phototherapy by a referring paediatrician in 12 (18.5%).
Guidelines for giving phototherapy for jaundice in babies born beyond 35 weeks of gestation have been published by various organisations, including the American Academy of Pediatrics (AAP)[1] and others, such as the National Institute for Health and Clinical Excellence (NICE).[2] The practical implementation of such guidelines and factors associated with possible non-adherence have not been studied, especially in self-paying tertiary-care centres of the developing world, such as India. This prompted us to review our data concerning adherence to published phototherapy guidelines, and to determine the reasons, if any, for non-adherence.
Methods
In this retrospective study, the case records of neonates admitted between August 2012 and August 2013 in a self-paying, tertiary-level neonatal intensive care unit (NICU) of northern India were reviewed. The following were recorded: baby's and mother's blood group, gestational age, serum bilirubin level with age in hours, duration of phototherapy, risk factors associated with hyperbilirubinaemia, e.g. history of birth asphyxia,[1] glucose-6-phosphate dehydrogenase (G6PD) status, thyroid profile and sepsis screen (if done). The study protocol received institutional ethics committee approval. Data were analysed using statistical software SPSS version 17 (IBM, USA).
Results
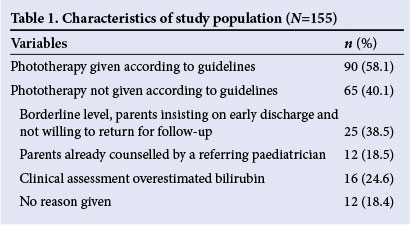
Of 571 admissions, 319 were term babies (including 3 babies who required an exchange transfusion), and 155 infants received phototherapy. Only 90/155 (58.1%) received phototherapy according to the AAP 2004 guidelines (Table 1).[1] In 65 (41.9%) babies, phototherapy was initiated below the recommended serum bilirubin level. In 25/65 (38.5%), phototherapy was initiated because the parents insisted on early discharge and were unlikely to be available for further follow-up. In 12 (18.4%), early phototherapy was initiated because a local paediatrician had referred the baby after counselling. In 16 (24.6%), clinical assessment of serum bilirubin was considered to be higher than was reported by the laboratory, and among these, 10 babies had risk factors for hyperbilirubinaemia and received phototherapy as a precautionary measure. The median duration of phototherapy was 36 hours in the case of those babies who received phototherapy according to the guidelines, and 24 hours in the case of babies receiving phototherapy below the recommended bilirubin level.
Discussion
In this study, we found that the guidelines for starting phototherapy in term neonates were ignored in more than 40% of babies in this particular hospital. Early intended discharge with reluctance to return for follow-up (most common reason), inappropriate counselling by a referring paediatrician, and discordance between laboratory value and clinical assessment were the key factors that led to non-adherence to available guidelines for the initiation of phototherapy. As phototherapy causes disruption of mother-and-baby bonding and also has cost implications, its empirical use should be minimised. Babies with high-risk factors have more chances of receiving phototherapy despite having a bilirubin level below the recommended level.
Conclusion
Phototherapy guidelines are not always adhered to. Similar studies from other centres are required in order to confirm reasons for nonadherence and to minimise deviation from guidelines.
References
1. American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics 2004;114(1):297-316. [http://dx.doi.org/10.1542/peds.114.L297] [ Links ]
2. National Collaborating Centre for Womens and Children's Health, for the National Institute for Health and Clinical Excellence (NICE). Neonatal jaundice: Clinical guidelines. London: Royal College of Obstetricians and Gynaecologists, 2010. [ Links ]
 Correspondence:
Correspondence:
T Ekram
tarique2k3@yahoo.co.in














