Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Child Health
versión On-line ISSN 1999-7671
versión impresa ISSN 1994-3032
S. Afr. j. child health vol.9 no.1 Pretoria ene. 2015
RESEARCH
Sleep duration and its effect on nutritional status in adolescents of Aligarh, India
N FaiziI; Z KhanII; A AmirIII; S A AzmiIV
IMBBS, MD, MPH; JN Medical College and Hospital, Aligarh Muslim University, Aligarh, India
IIMBBS, DCH, MD; JN Medical College and Hospital, Aligarh Muslim University, Aligarh, India
IIIMBBS, MD; JN Medical College and Hospital, Aligarh Muslim University, Aligarh, India
IVMBBS, MD; JN Medical College and Hospital, Aligarh Muslim University, Aligarh, India
ABSTRACT
BACKGROUND: The World Health Organization describes obesity as one of today's most blatantly visible - yet most neglected - public health problems. Sleep duration has been found to have an association with overweight and obesity in many studies, most of which have been conducted outside India. The prevalence of chronic partial sleep deprivation has increased dramatically in the past half century, in parallel with the rising epidemics of overweight and obesity. In addition, sleep per se has a special relevance in obesity
OBJECTIVE: This study was part of a larger study based on the Global School Health Survey, and was conducted in the 13 - 15-year-old age group. The study had two objectives: first, it enquired into sleep duration in the aforementioned adolescents and assessed whether this was adequate or inadequate; and second, it sought to evaluate and assess the relationship between sleep duration and the nutritional status of these adolescents, whether overweight or obese
METHODS: A cross-sectional study was conducted in all three schools affiliated to the Aligarh Muslim University Board of Examination. A pretested and prevalidated questionnaire was used to assess sleep duration, and anthropometry was done on all the students of these schools who fulfilled the inclusion criteria. AnthroPlus (World Health Organization, Switzerland) and SPSS (IBM, USA) version 20 were used for z-score and other statistical calculations, respectively
RESULTS: A total of1 416 students were studied, of which 23.6% reported inadequate sleep duration. It was found that those with inadequate sleep had significantly higher odds of being overweight or obese, with an odds ratio of 1.56 (confidence interval 1.12 - 2.15). The inadequacy of sleep duration was also associated with a higher body mass index for age z-score (0.77 (standard deviation 0.57)), compared with those with adequate sleep duration (-0.31 (0.08)), which was found to be significant (t=22.59, df=1, p<0.001
CONCLUSION: Inadequate sleep is an obesogenic factor, even in developing countries. It is a cause of concern, as the habits developed/ strengthened at this stage may be lifelong
The World Health Organization (WHO) describes obesity as one of today's most blatantly visible - yet most neglected - public health problems.[1] The prevalence of overweight and obesity has been gradually increasing, becoming a public health problem, not only in developed countries but also in developing countries such as India.[2] The 'New World syndrome', which is likely to create an enormous socioeconomic and public health burden of non-communicable diseases, states obesity as one of the first cluster of diseases.[3]
Lifestyle factors are cited as one of the reasons for an increase in the prevalence of overweight or obesity. Significant studies have been conducted to identify the relationship between lifestyle factors and obesity. Prior research has examined factors such as nutrition transition, junk food and soft drink intake frequency and physical activity profiles for their association with the prevalence of overweight or obesity. An optimal public health outcome is achievable if the factors causing obesity, besides the conventional ones of diet and physical activity, can be scientifically found, and corresponding remedial measures implemented.[4] Among these other factors, sleep duration has been found to have an association with overweight and obesity in many studies, most of which have been conducted outside India.[5-7] The prevalence of chronic partial sleep deprivation has increased dramatically in the past half century, in parallel with the rising epidemics of overweight and obesity.[8]
According to Dahl and Lewin,[9] sleep duration per se has a special relevance in adolescence, as: (i) there are substantial biological and psychosocial changes in sleep, and circadian regulation exists across pubertal development; (ii) interactions between physical and psychosocial domains during adolescence can lead to dramatic alterations in sleep patterns and habits; (iii) increasing evidence indicates that many adolescents frequently obtain insufficient sleep.[9] Therefore, it is becoming increasingly important to study the prevalence of inadequate sleep duration (IASD) in adolescents and its plausible association with their nutritional status.
Adolescence is considered a period of transition, and the habits that are developed during this period usually continue for life. Environmental and habitual factors for various diseases, if identified during this period, can be corrected by taking preventive actions before they become incurable for life. IASD or sleep loss due to voluntary bedtime restriction has become a hallmark of modern societies, such as those in the USA and others.[10] Such lifestyle patterns are now increasingly being imported to developing countries such as India. Timely research and effective intervention can help in restraining this from becoming a pervasive problem, which can potentially affect a significant 22% of the aggregate Indian population, comprising adolescents. A school-based intervention is likely to be more successful in this regard, as adolescence is also considered as a unique phase in life that presents the greatest opportunities for sustained health and wellbeing through education and preventive efforts.[11]
Driven by the aforementioned intent and reasons, this study, as a part of a larger study based on the Global School Health Survey, was conducted in the 13 - 15-year-old age group with two objectives: first, the study made an enquiry into the sleep duration in Indian adolescents, and assessed whether this was adequate or inadequate; and second, it sought to evaluate and assess the relationship between sleep duration and the nutritional status of these adolescents, whether overweight/obese.
Methods
This research was a cross-sectional, one-time assessment of nutritional status and selfreported sleep duration at night. The study was conducted over a period of 6 months, from November 2011 to April 2012.
The study was conducted in three different Aligarh schools, all of which are affiliated to the Aligarh Muslim University Board of Examination, and rank among the largest schools in the district of Aligarh. Prior permission was obtained from the school authorities.
The inclusion criterion was all students aged between 13 and 15 years, enrolled in the aforementioned schools, who were present and gave their consent for the study.
The students were weighed with minimal clothing and standing height was used.
The proforma comprised questions on the particulars of the participants and the usual duration of sleep. Concurrently, anthropometry was conducted and recorded. Assessment of average sleep duration was based on the answers to two specific questions: (i) On a usual working day (weekday), what is the time that you go to bed and what is the time that you wake up? (ii) On Saturday nights, what time do you go to bed? and (iii) At what time do you wake up on Sundays? While these questions were drawn from previous published research, there were a few minor adaptations,[12] because these schools are open 6 days a week. The questionnaire was pilot tested and validated before the actual research was conducted.
From the answers to the questions mentioned above, average sleep duration was found to be equal to:
(weekday sleep duration x 6/7) + (weekend sleep duration x 1/7).
Sleep duration <7 hours/day was qualified as IASD, and ≥ 7 hours/day as adequate sleep duration (ASD), based on previous studies.[13]
Any adolescent with a body mass for age z-score of ≥ 1 standard deviation (SD) (equivalent to 85th percentile) was considered overweight, as per the WHO Reference Standards 2007 (WHO AnthroPlus). Any adolescent with a body mass for age z-score of ≥2 SD (equivalent to 97th percentile), was considered obese, as per the WHO Reference Standards 2007 (WHO AnthroPlus).[14]
The nutritional status/anthropometric records were assessed against the WHO multicentric growth reference standards (WHO Multicentric Growth Reference Standards (MGRS)), as the WHO AnthroPlus software was used in this study.[14]
Anthropometric measurements of weight and standing height were recorded using standard techniques as prescribed.[15] Weight was measured with minimal possible clothing in the upright position to the nearest 0.1 kg using calibrated instruments, and height was measured without shoes to the nearest 0.1 cm. Body mass index (BMI) for age z-scores were used to define overweight and obese. Other precautions taken during the study were regular calibration of instruments and recording date of birth from written records (school register). Those students whose BMI-for-age z-score values were flagged by WHO AnthroPlus during the data entry or who were found to have extreme values were revisited within 2 days, and anthropometry was repeated.
The multidisciplinary Institutional Board of Studies ethically approved the study. Appropriate counselling, health education, and balanced diet and nutrition advice were offered to all the participants. Those who were in need of referral were referred to the JN Medical College, Aligarh.
Data management and processing
All the students of the three schools who fulfilled the inclusion criteria (N=1 416) were included in the study. Weight and height were entered in WHO AnthroPlus on the day of visit. AnthroPlus was used to find the z-scores (based on the WHO MGRS 2007)[14] for that age and gender. SPSS (IBM, USA) version 20 was used to derive the relationship between sleep duration and overweight/obesity, and for other relevant statistical calculations. Chi-square tests were applied to determine the differences between sleep duration in males and females, and to examine the association between overweight/obesity and inadequacy of sleep duration, if any. BMI z-scores of those with IASD were compared with those who had ASD by i-test.
Results
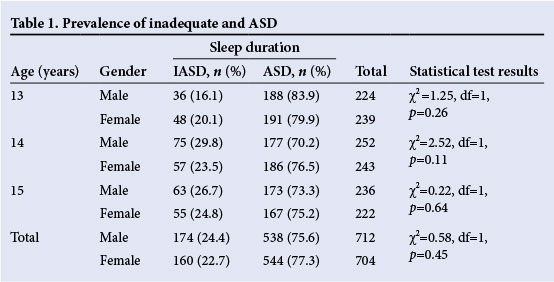
A total of1 416 students were sampled for the study, including 712 males and 704 females. Among the study population, 23.6% (n=334) reported IASD, and 76.4% (n=1 082) reported ASD. There was no significant difference between the sleep duration prevalence in males and females (Table 1). The prevalence of overweight and obesity was found to be 12.3% (n=174) and 2.33% (n=33), respectively, without any significant difference between genders.
Among those with IASD, 19.2% (64/334) were found to be either overweight or obese, significantly higher than 13.2% overweight/ obese in those with ASD. Further analysis revealed that the probability of being either overweight or obese was significantly higher in those who reported IASD (odds ratio (OR)=1.56, 95% confidence interval (CI) 1.12 - 2.15) (Table 2).
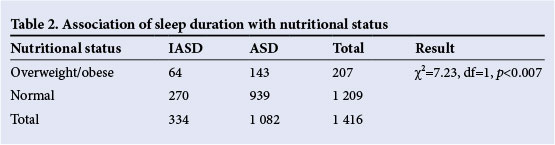
The mean (SD) BMI was found to be different in the IASD (22.2 (2.3)) and ASD groups (19.1 (2.3)). The mean BMI-for-age z-score for the IASD group was found to be 0.77 (0.57) compared with the ASD group (-0.31 (0.08)), and these values were significantly different on i-testing (i=22.54, df=1; p<0.001). Thus, IASD had a higher OR of being overweight or obese and was also associated with a higher BMI-for-age z-score and with overall BMI.
Discussion
This study found that sleep duration was inadequate in 23.6% of the adolescents, and those with IASD had a higher chance of developing overweight or obesity and tended to have a higher BMI-for-age z-score than their ASD counterparts. A similar association between a high BMI and obesity has been reported for comparable age groups in Germany,[7] the USA,[4,16] Vietnam,[17[ Taiwan[18] and the UK,[19] among others.
In India, Gujarati adolescents of 16 - 19 years old were found to have a significant relationship between IASD at night and body fat percentage and total body fat mass.[13] In south India, in individuals of 6 - 16 years old who visited the hospital for minor complaints or routine checkups, inadequacy of sleep was found to be associated with being overweight, based on International Obesity Task Force[20] standards. In contrast, a report from south India by the National Institute of Nutrition[21] in Hyderabad found no significant difference between the sleep duration of normal and overweight adolescents in south India. To our knowledge, this is the first community-based study in north India with a large sample size that employs the recently recommended WHO MGRS 2007 standards and examines the effect of sleep duration inadequacy.
There are various plausible mechanisms for the association between IASD and obesity. Sleep restriction reduces the secretion of adipocyte and appetite-regulating hormone leptin, and consequently increases one's appetite.[22] Loss of adequate sleep also results in higher production of ghrelin; the resultant leptin-ghrelin interaction leads to increased appetite. In addition, sleep inadequacy affects basic metabolic rate and also provides more opportunity to eat. Together with the thermic effect of food,[23] these factors cause tiredness and lead to low physical activity. It is now well-known that regardless of whether sleep deprivation is acute or chronic, both lead to appetite dysregulation and weight gain. These, in turn, lead to insulin resistance, causing an increased risk of diabetes mellitus type 2.[10]
Some studies have also found gender differences in the association between sleep inadequacy and obesity; some found the association to be significant only in boys[19,23,24] and some found a higher probability of association in boys.[25] Our study did not find any such differences either in existence or in the degree of association. IASD was found to have an association with both genders, and there was no significant difference between the degree of association in boys or girls.
Study limitations
The main limitation of this study was that the measurement of sleep duration was based on self-reporting, which may not be the most reliable of the methods. However, there is no reason to believe that the non-obese or non-overweight adolescents could have been the only ones misreporting their sleep duration. Therefore, the authors believe that this limitation may not have a significant effect on the accuracy and generalisability of results. Another important limitation is the issue of temporality, which has been present in many such studies, including the meta-analysis by Cappuccio et al.[6] Without the temporality, that is whether an adolescent had inadequate sleep therefore she/he is obese or vice versa, it is difficult to confirm causality by this study alone.
Conclusions
There is significant epidemiological evidence that points towards the inadequacy of sleep being an obesogenic factor, even in developing countries such as India. With non-communicable diseases accounting for nearly 56% of the total mortality in South-East Asia,[26] in which India has a major share, a variable such as sleep, which may lead to both obesity and/or diabetes mellitus type 2, cannot and should not be ignored.
It should be stressed that for a healthy mind and body, an adequate duration of optimum sleep is important, especially during school education years. Adolescence is a transition phase in human development; sleep deprivation as a habit often develops during this phase because of changes in biological timing of sleep, for example adolescents going to bed later but waking up on time for school.[27] Therefore, specific advice should be given to students at schools. Boarding schools should lay down and enforce strict rules regarding the time to go to bed. Studying late at night should be discouraged, and healthier alternatives should be provided. Because of the vulnerable nature of these ages, advice should also be enforced through primary healthcare centres and adolescent clinics, as the habits developed or strengthened during adolescence often tend to stay for life.
Other important advice suggested by experts includes sleep hygiene, such as a regular bedtime routine, ensuring a suitable bedroom environment with a comfortable bed that should be used only for sleeping (and not reading or listening to music), not indulging in active physical activity within a couple of hours before sleeping, and removal of televisions, computers or other gadgets from the bedroom. It is also important to restrict the intake of caffeinated drinks in the evening or night, and to avoid stimulating activities during bedtime, including but not limited to heavy study, playing computer games, or active debating and discussions.[28] In particular, a key piece of advice is not to have a television in the room in which the adolescent sleeps.[29] Although these suggestions have been researched in other settings, an important opportunity for research exists in developing countries such as India, where these suggestions should be tested further to assess their effectiveness.
References
1. World Health Organization. Nutrition: Controlling the Global Obesity Epidemic. Geneva: World Health Organization, 2013. http://www.who.int/nutrition/topics/obesity/en/ (accessed 28 September 2013). [ Links ]
2. Gupta DK, Shah P, Misra A, et al. Secular trends in prevalence of overweight and obesity from 2006 to 2009 in urban Asian Indian adolescents aged 1417 years. PLoS One 2011;6(2):e17221. [http://dx.doi.org/10.1371/journal.pone.0017221] [ Links ]
3. World Health Organization. Obesity: Preventing and Managing a Global Epidemic. Report of a WHO Consultation. WHO Technical Report Series No. 894. Geneva: World Health Organization, 2000. [ Links ]
4. Gupta NK, Mueller WH, Chan W, Meininger JC. Is obesity associated with poor sleep quality in adolescents? Am J Hum Biol 2002;14(6):762-768. [http://dx.doi.org/10.1002/ajhb.10093] [ Links ]
5. Lumeng JC, Somashekar D, Appugliese D, Kaciroti N, Corwyn RF, Bradley RH. Shorter sleep duration is associated with increased risk for being overweight at ages 9 to 12 years. Pediatrics 2007;120(5):1020-1029. [http://dx.doi.org/10.1542/peds.2006-3295] [ Links ]
6. Cappuccio FP, Taggart FM, Kandala NB, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep 2008;31(5):619-626. [ Links ]
7. Kleiser C, Rosario AS, Mensink GBM, Prinz-Langenohl R, Kurth BM. Potential determinants of obesity among children and adolescents in Germany: Results from the cross-sectional KiGGS study. BMC Public Health 2009;9:46. [http://dx.doi.org/10.1186/1471-2458-9-46] [ Links ]
8. Knutson KL, van Cauter E, Rathouz PJ, DeLeire T, Lauderdale DS. Trends in the prevalence of short sleepers in the USA: 1975-2006. Sleep 2010;33(1):37-45. [ Links ]
9. Dahl RE, Lewin DS. Pathways to adolescent health sleep regulation and behavior. J Adolesc Health 2002;31(6 Suppl):175-184. [ Links ]
10. Spiegel K, Knutson K, Leproult R, Tasali E, Cauter EV. Sleep loss: A novel risk factor for insulin resistance and type 2 diabetes. J Appl Physiol 2005;99(5):2008-2019. [http://dx.doi.org/10.1152/japplphysiol.00660.2005] [ Links ]
11. Kleinert S. Adolescent health: An opportunity not to be missed. Lancet 2007;369(9567):1057-1058. [http://dx.doi.org/10.1016/S0140-6736(07)60374-2] [ Links ]
12. Lytle LA, Pasch KE, Farbaksh K. The relationship between sleep and weight in a sample of adolescents. Obesity (Silver Spring) 2011;19(2):324-331. [http://dx.doi.org/10.1038/oby.2010.242] [ Links ]
13. Shaikh WA, Patel M, Singh S. Sleep deprivation predisposes Gujarati Indian adolescents to obesity. Indian J Community Med 2009;34(3):192-194. [http://dx.doi.org/10.4103/0970-0218.55282] [ Links ]
14. Blössner M, Siyam A, Borghi E, Onyango A, de Onis M. WHO AnthroPlus for Personal Computers Manual Software for Assessing Growth of the World's Children. Geneva: World Health Organization, 2009. [ Links ]
15. World Health Organization. Physical Status: The Use and Interpretation of Anthropometry. WHO Technical Report Series No. 854. Geneva: World Health Organization, 1995:439. [ Links ]
16. Snell EK, Adam EK, Duncan GJ. Sleep and the body mass index and overweight status of children and adolescents. Child Dev 2007;78( 1):309-323. [http://dx.doi.org/10.1111/j.1467-8624.2007.00999.x] [ Links ]
17. Dieu HT, Dibley MJ, Sibbritt D, Hanh TT. Prevalence of overweight and obesity in preschool children and associated socio-demographic factors in Ho Chi Minh City, Vietnam. Int J Pediatr Obes 2007;2(1):40-50. [http://dx.doi.org/10.1080/17477160601103922] [ Links ]
18. Chen MY, Wang EK, Jeng YJ. Adequate sleep among adolescents is positively associated with health status and health-related behaviors. BMC Public Health 2006;6:59. [http://dx.doi.org/10.1186/1471-2458-6-59] [ Links ]
19. Gibson S, Lambert J, Neate D. Associations between weight status, physical activity, and consumption of biscuits, cakes and confectionery among young people in Britain. Nutr Bull 2004;29(4):301-309. [http://dx.doi.org/10.1111/j.1467-3010.2004.00445.x] [ Links ]
20. Cole TJ, Bellizzi NC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000;320(7244):1240-1246. [http://dx.doi.org/10.1136/bmj.320.7244.1240] [ Links ]
21. National Institute of Nutrition. Adolescent Obesity: Andhra Pradesh. Hyderabad: National Institute of Nutrition, 2007. [ Links ]
22. Mullington JM, Chan JL, van Dongen HP, et al. Sleep loss reduces diurnal rhythm amplitude of leptin in healthy men. J Neuroendocrinol 2003;15(9):851-854. [ Links ]
23. Knutson KL. The association between pubertal status and sleep duration and quality among a nationally representative sample of US adolescents. Am J Hum Biol 2005;17(4):418-424. [http://dx.doi.org/10.1002/ajhb.20405] [ Links ]
24. Eisenmann JC, Ekkekakis P, Holmes M. Sleep duration and overweight among Australian children and adolescents. Acta Paediatr 2006;95(8):956-963. [http://dx.doi.org/10.1080/08035250600731965] [ Links ]
25. Sekine M, Yamagami T, Handa K, et al. A dose response relationship between short sleeping hours and childhood obesity: Results of the Toyama Birth Cohort Study. Child Care Health Dev 2002;28(2):163-170. [ Links ]
26. World Health Organization. Global burden of disease: Updated projections. Geneva: World Health Organization, 2008. http://www.who.int/healthinfo/global_burden_disease/estimates_regional/en/index.html (accessed 2 March 2013). [ Links ]
27. Carskadon MA, Acebo C, Jenni OG. Regulation of adolescent sleep: Implications for behavior. Ann N Y Acad Sci 2004;1021:276-291. [http://dx.doi.org/10.1196/annals.1308.032] [ Links ]
28. Taheri S. The link between short sleep duration and obesity: We should recommend more sleep to prevent obesity. Arch Dis Child 2006;91(11):881-884. [http://dx.doi.org/10.1136/adc.2005.093013] [ Links ]
29. Spear BA, Barlow SE, Ervin C, et al. Recommendations for treatment of child and adolescent overweight and obesity. Pediatrics 2007;120(Suppl 4):S254-S288. [http://dx.doi.org/10.1542/peds.2007-2329F] [ Links ]
 Correspondence:
Correspondence:
N Faizi
nafisfaizi@gmail.com














