Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Child Health
On-line version ISSN 1999-7671
Print version ISSN 1994-3032
S. Afr. j. child health vol.8 n.2 Pretoria May. 2014
RESEARCH
The practice of breastfeeding by healthcare workers in the Federal Teaching Hospital, Abakaliki, southeastern Nigeria
O U AnyanwuI; C T EzeonuII; O B EzeanosikeIII; C O OkikeIV
IMBBS, MNPMC, MWACP; Federal Teaching Hospital, Abakaliki, Ebonyi State, Nigeria
IIMBBS, FNPMC; Federal Teaching Hospital, Abakaliki, Ebonyi State, Nigeria; Ebonyi State University, Abakaliki, Ebonyi State, Nigeria
IIIMBBS, FWACP; Federal Teaching Hospital, Abakaliki, Ebonyi State, Nigeria; Ebonyi State University, Abakaliki, Ebonyi State, Nigeria
IVMBBS, FWACP; Federal Teaching Hospital, Abakaliki, Ebonyi State, Nigeria; Ebonyi State University, Abakaliki, Ebonyi State, Nigeria
ABSTRACT
BACKGROUND: Optimal breastfeeding practices include exclusive breastfeeding (EBF) for the first 6 months of life, followed by continued breastfeeding with adequate complementary foods on to at least 2 years of age. This is expected to be well known and practised by healthcare workers (HCWs) who are in the position to educate the community.
OBJECTIVE: To determine the actual breastfeeding practices of HCWs in a tertiary hospital in south-eastern Nigeria.
METHODS: We conducted a cross-sectional, descriptive study among female HCWs at the Federal Teaching Hospital, Abakaliki, southeastern Nigeria, using a self-administered, semi-structured questionnaire.
RESULTS: One hundred HCWs were recruited, including doctors, nurses, pharmacists and other HCWs. Only 3% practised EBF with all their children, their cited reasons being a busy work schedule (61.8%), EBF being too stressful (18.4%), ignorance of benefits of EBF (13.2%) and lack of family support (3.9%). Only 1% breastfed their babies up to 2 years. The reasons for failing to do so included refusal of the child to breastfeed (32.6%), another pregnancy (30.4%), feeling it was shameful (10.9%) and feeling that the baby was too old (8.7%).
CONCLUSION: There are obvious shortcomings in breastfeeding practices among HCWs. They need to be empowered and supported to promote and support breastfeeding among their patients in particular and society in general.
Breastfeeding is a way of providing ideal nutrition for the healthy growth and development of infants.[1]-The importance of breastfeeding to child health has been documented repeatedly. The United Nations Children's Fund (UNICEF) included breastfeeding as one of the child survival strategies during the World Health Organization (WHO) WHO/UNICEF policymakers' meeting on 'Breastfeeding in the 1990s: A Global Initiative', held in Italy on 30 July - 1 August 1990.[2] The Innocenti declaration was then produced and adopted, calling on nations and international organisations to draw up action strategies for the protection, promotion and support of breastfeeding.[2]
Healthcare workers (HCWs) have a great influence on infant feeding practices,[3,4] because the importance of healthy nutrition to the normal growth and development of children is well known to them.[4] It is expected that they impart their knowledge of the advantages of breastfeeding to the baby, the mother and society, to their clients. Based on this, we postulate that female HCWs would practise and promote what is ideal for their own babies. In a study of paediatricians and the promotion/support of breastfeeding, it was reported that respondents who had personal experience with breastfeeding were 2.3 times more likely to report supportive policies.[4] It is therefore our expectation that HCWs who have good breastfeeding practices will most likely promote what they believe in and practise.
Optimal breastfeeding practices include exclusive breastfeeding (EBF) for 6 months and continuing thereafter with adequate complementary feeds until 2 years of age and beyond.[5] However, despite the many known benefits of optimal breastfeeding, many barriers to breastfeeding exist. Some of these barriers are lack of support for the breastfeeding mother, advertisements of infant formula and early return to employment.[6,7]
Working women have identified their return to work as a major barrier to breastfeeding,[8-11] proving that facilities to support breastfeeding at the workplace should be encouraged.
The female HCW is at the helm of the campaign and support for breastfeeding, and because the role of HCWs in getting breastfeeding off to a good start and maintaining it can be decisive, it is critically important that their attitudes and personal experiences with its practice are described. It is for this reason that the authors decided to describe the experience and the actual practice of breastfeeding by HCWs in a tertiary hospital in southeastern Nigeria.
Methods
We carried out a hospital-based, cross-sectional, descriptive study among female HCWs of the Federal Teaching Hospital Abakaliki (FETHA), south-eastern Nigeria, which is a designated baby-friendly institution and the major tertiary health institution in its state, Ebonyi.
A consecutive convenience sample of 100 female HCWs met the inclusion criteria of being in practise within a baby-friendly tertiary hospital setting for at least 2 years, having one or more children and willingness to participate after due information. Those who were unwilling (20 participants), did not have a child (5 participants) or had not worked for 2 years in a tertiary hospital (7 participants) were excluded. Data were collected using a self-administered, semi-structured questionnaire. The questionnaire surveyed information on demographic characteristics such as occupation, age, religion, tribe and the number of children the participant had. Structured questions about EBF practice and continued breastfeeding until 2 years were included. EBF was defined as giving the baby breastmilk only for 6 months with no prelacteal feeds and no other fluids. Questions on reasons for not practising correct breastfeeding were left open so that respondents responded in their own words. Their responses were subsequently categorised.
Analysis was done using SPSS (version 17) and Epi Info (version 12.1). Descriptive statistics were used to summarise the data. Differences between groups were tested using the Pearson χ2 test or Fisher's exact test where the frequency was <5. The level of significance was set at p-value <0.05.
Ethical approval for the study was obtained from the FETHA research and ethics committee. Written consent was sought from every participant.
Results
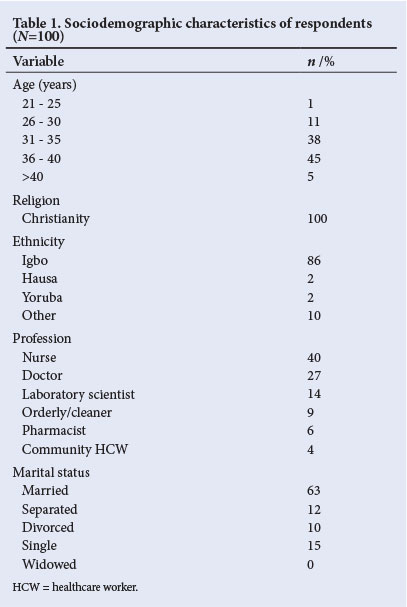
Participant sociodemographics are presented in Table 1. Most (45%) belonged to the 36 - 40-year age group; 38% were aged 31 - 35 years; and the mean±standard deviation age was 35±6.2 years (range 21 - 42). The majority were nurses (40%) and doctors (27%). All participants were Christians, mostly Roman Catholic (42%). Most were of the Igbo tribe (86%), 2% each were of the Hausa and Yoruba tribes while the remaining 10% consisted of one individual each from 10 other tribes. Sixty-eight per cent of the respondents had three or more children with a mode of 3. Married respondents accounted for 63%, 12% were separated, 15% had never married (single mothers) while 10% were divorced. There were no widows.
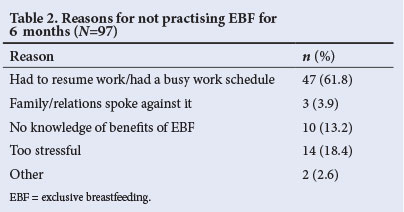
Twenty-five per cent had exclusively breastfed at least one of their children for 6 months, while only 3% had practised EBF for all their children. The majority (75%) of those who had breastfed at least one baby exclusively for 6 months had done so for their first child. Most (61.8%) of those who had not practised EBF for 6 months at all attributed this to having had to resume a busy work schedule, 18.4% said it was too stressful, while 13.2% (mostly orderlies/cleaners) had no knowledge of the benefits of EBF for 6 months (Table 2). Another 3.9% did not practise EBF because they lacked family support as their families spoke against it (one doctor, one nurse and one laboratory scientist).
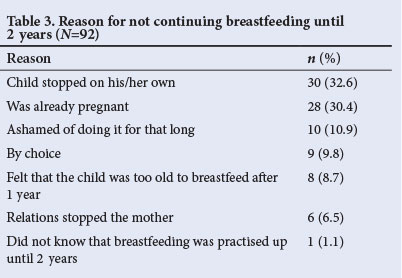
Eight per cent of the respondents had breastfed at least one of their babies for up to 2 years, while only 1% had done so for all their babies. Those who could not gave reasons such as: the babies stopped on their own (32.6%), they were expecting another baby (30.4%), the baby was too old to suckle after 1 year (8.7%) or they were ashamed of breastfeeding up until 2 years (10.9%) (Table 3). The mean age of the children when stopping breastfeeding entirely was 14 months.
Doctors stopped breastfeeding earlier (mean child age 10 months) than other HCWs (mean 14 months; p<0.05), and older mothers breastfed longer than younger ones (p<0.05) as shown in Tables 4 and 5. There was no significant relationship between profession, age of the HCW and having practised EBF for 6 months (p>0.05).
Discussion
This study represents breastfeeding practices of non-nulliparous female HCWs who were mostly within childbearing age. The prevalence (25%) of EBF reported in the current study is within the range of 20 - 43%[12,13] reported for developing countries, and is comparable with the 27% prevalence reported as Nigeria's average.[14] However, it is higher than the 11.1% prevalence found in a previous study among resident doctors in Benin, Nigeria, probably because the current study included other HCWs and not just doctors as was the case in the study by Sadoh et al.[5] Furthermore, the prevalence is markedly below the 90% level recommended by the WHO[16,17] as a level that must be reached for this cost-effective intervention to save infant's lives. This emphasises the need to intensify awareness and hospital-based interventions that promote EBF among HCWs. In addition, only 3% of these HCWs breastfed all their babies, the majority practising EBF for their first babies only, probably because as only children, first babies enjoyed more maternal attention than subsequent siblings.
In this study, the reasons for having not practised EBF were busy work schedule (61.8%) and that EBF was too stressful (18.4%), which were similar to reports of deterrents of EBF previously reported in SA[6] and Nigeria.[7] A notable finding was that ignorance of the benefits of EBF was a reason for having not practised EBF among 13.2% of the respondents, reported exclusively among the lower cadre of HCWs (community health extension workers (CHEWs) and orderlies), showing that training on the benefits, support and protection of breastfeeding may have eluded this group and instead been concentrated on the senior HCWs (doctors and nurses). It may erroneously be assumed that the junior HCWs are not the primary HCWs that educate patients. However, mothers who consider HCWs as role models may not be able to differentiate orderlies and CHEWs from nurses and hence may seek and subsequently obtain wrong information concerning breastfeeding from those who have poor knowledge of the benefits of EBF. This may give rise to low rates of EBF in the community.
Although only 3.9% attributed not breastfeeding exclusively to a lack of family support, this finding agrees with previous reports[7,8] that a lack of family support affects a mother's ability to breastfeed exclusively since women struggle to withstand family pressures. This indicates that substantial interventions have to be put in place to empower HCWs to practise EBF, for their own children's sake, and to encourage the imparting of the correct message to their community.
The current study shows that only 8% of HCWs breastfeed at least one child for up to 2 years with only 1% doing so for all their children; primary reasons being that the babies stopped on their own (32.6%) and that the mothers were expecting another baby (30.4%). Other reasons were that the baby was too old to suckle after 1 year (8.7%) and 10.9% were ashamed of breastfeeding to 2 years. These reasons reflect these mothers' knowledge of breastfeeding practices and show that many may still be ignorant of correct practices and the benefits of breastfeeding. A remarkable number were ashamed of breastfeeding for 2 years, showing low self-esteem when it comes to breastfeeding their infants. If HCWs cannot proudly breastfeed their babies, who then would support and promote the WHO guidelines of continuing breastfeeding until 2 years?
The mean duration of breastfeeding entirely was 14 months, with the shortest duration of breastfeeding (mean 10 months) recorded among doctors and younger mothers. There was no significant influence of religion and tribe on breastfeeding practice, probably because the participants were predominantly Christians and of the Igbo tribe, and very few were of other other religions and tribes.
The major limitation of this study might have been recall bias: the HCWs were aged 21 - 42 years, and they were asked about the feeding practices of their infants when they were <2 years of age, without considering the age of their last child; a long recall period was involved and some mothers may have forgotten their exact practice and have given wrong accounts, altering the actual prevalence of EBF. HIV status may be an important factor affecting the practice of breastfeeding of mothers; however, the researchers did not access the HIV status of the HCWs. In addition, measuring EBF prevalence with a cross-sectional study using recall since birth is difficult. A better design that would have given a reliable estimate would have been a longitudinal study, where a cohort of infants is followed from birth with frequent recordings of breastfeeding. However, a longitudinal study is expensive, takes a long time to conduct and is associated with attrition of the mother-child pairs with time.
Conclusion
There are obvious shortcomings in breastfeeding practices among HCWs attributable to work schedule, poor family support and lack of knowledge. HCWs need to be empowered and supported to practise breastfeeding and in turn promote and support breastfeeding among their patients in particular, and society in general. Training and retraining should be conducted periodically to improve their breastfeeding practices and knowledge of correct breastfeeding.
References
1. Egbuonu I, Ojukwu JU. Infant feeding. In: Azubuike JC, Nkanginieme KEO, editors. Pediatrics and Child Health in a Tropical Region. 2nd ed. Owerri: African Educational Services, 2007:224-239. [ Links ]
2. Afzal MF, Saleemi MA, Asghar MF, Manzoor M, Fatima M, Fazal M. A study of knowledge, attitude and practice of mothers about breast feeding in children. Ann King Edward Med Uni 2002;8:28-29. [ Links ]
3. Leviniene G, Petrauskiene A, Tamilevicience E, Kudzyte J, Labanauskes L. The evaluation of knowledge and activities of primary health care professionals on promoting breast-feeding. Medicina (Kaunas) 2009;45(3):238-247. [ Links ]
4. Feldman-Winter LB, Schanler RJ, O'Connor KG, Lawrence RA. Pediatricians and the promotion and support of breastfeeding. Arch Pediatr Adolesc Med 2008;162:1142-1149. [http://dx.doi.org/10.1001/archpedi.162.12.1142] [ Links ]
5. World Health Organization. Global Strategy for Infant and Young Child Feeding. Geneva: WHO, 2003. http://www.who.int/nutrition/publications/gs_infant_feeding_text_eng.pdf (accessed on 21st June 2013). [ Links ]
6. Shah S, Rollins NC, Bland R. Breastfeeding knowledge among health workers in rural South Africa. J Trop Pediatr 2005;51(1):33-38. [http://dx.doi.org/10.1093/tropej/fmh071] [ Links ]
7. Agbo HA, Envuladu EA, Adams HS, et al. Barriers and facilitators of the practise of exclusive breastfeeding among working class mothers: A study of female resident doctors in tertiary health institutions in Plateau State. E3 J Med Research 2013;2(1):112-116. [ Links ]
8. Sinniah D, Chon FM, Arokiasamy J. Infant feeding practices among nursing personnel in Malaysia. Acta Paediatr Scand 1980;69:525-529. [http://dx.doi.org/10.1111/j.1651-2227.1980.tb07125.x] [ Links ]
9. Stewart-Glenn J. Knowledge, perception and attitude of managers, co-workers and employed breastfeeding mothers. AAOHN J 2009;56:423-429. [ Links ]
10. Haider R, Begum S. Working women, maternity entitlements and breastfeeding: A report from Bangladesh. J Hum Lact 1995;11:273-277. [http://dx.doi.org/10.1177/089033449501100413] [ Links ]
11. Agunbiade MO, Ogunleye VO. Constraints to exclusive breastfeeding practice among breastfeeding mothers in Southwest Nigeria: Implications for scaling up. Int Breastfeeding J 2012;7:5-7. [http://dx.doi.org/10.1186/1746-4358-7-5] [ Links ]
12. Tiras EN, Sia EM. Prevalence and predictors of exclusive breastfeeding among women in Kigoma region, Western Tanzania: A community based cross-sectional study. Int Breastfeeding J 2011;6:17-18. [http://dx.doi.org/10.1186/1746-4358-6-17] [ Links ]
13. World Health Organization. The State of Breastfeeding in 33 Countries. Geneva: WHO, 2010. http://www.worldbreastfeedingtrends.org (accessed 16 June 2013). [ Links ]
14. Salami LI. Factors influencing breastfeeding practice in Edo State, Nigeria. AJFAND 2006;6(2):1-12. [http://dx.doi.org/10.4314/ajfand.v6i2.71755] [ Links ]
15. Sadoh AE, Sadoh WE, Oniyelu P. Breast feeding practice among medical women in Nigeria. Niger Med J 2011;52(1):7-12. [ Links ]
16. World Health Organization. Infant and Young Child Feeding: Model Chapter for Textbooks for Medical Students and Allied Health Professionals. Geneva: WHO, 2009. http://www.whqlibdoc.who.int/publications/2009/9789241597494_eng.pdf (accessed 21 June 2013). [ Links ]
17. Jones G, Steketee RW, Black RE, Bhutta ZA, Morris SS, Bellagio Child Survival Study Group. How many child deaths can we prevent this year? Lancet 2003;362:65-71. [http://dx.doi.org/10.1016/S0140-6736(03)13811-1] [ Links ]
 Correspondence:
Correspondence:
O U Anyanwu
(onyinyeanyanwugc@gmail.com)














