Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Child Health
On-line version ISSN 1999-7671
Print version ISSN 1994-3032
S. Afr. j. child health vol.8 n.2 Pretoria May. 2014
RESEARCH
Infant feeding practices during the first 6 months of life in a low-income area of the Western Cape Province
C GoosenI; M H McLachlanII; C SchüblIII
IM Nutrition, BSc Dietetics; Division of Human Nutrition, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
IIMA, PhD; Division of Human Nutrition, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
IIIDivision of Human Nutrition, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
ABSTRACT
BACKGROUND: Exclusive breastfeeding during the first 6 months of life protects against infant morbidity and mortality. Few studies describe the infant feeding practices of mothers living in low-income areas of the Western Cape Province of South Africa (SA).
OBJECTIVE: To describe the infant feeding practices of mothers of infants younger than 6 months in two low-income communities of SA.
METHODS: A cross-sectional community-based study using a structured questionnaire, and seven focus group discussions were conducted from February to August 2011 in Avian Park and Zwelethemba in Worcester, an urban area in the Western Cape.
RESULTS: Seventy-seven per cent of participants (n=108) had initiated breastfeeding. At the time of the study, 6% (n=8) breastfed exclusively. Ninety-four per cent (n=132) applied suboptimal breastfeeding practices: 36% (n=51) breastfed predominantly, 27% (n=38) breastfed partially and 31% (n=43) did not breastfeed. Ninety per cent (n=126) of the mothers had introduced water, of whom 83% (n=104) had done so before their infants were 1 month old. Forty-four per cent (n=61) of the mothers had introduced food or formula milk, of whom 75% (n=46) had done so before their infants were 3 months old. Qualitative findings indicated that gripe water, Lennon's Behoedmiddel and herbal medicines were also given to infants. Nutritive liquids and/or food most commonly given as supplementary feeds were formula milk and commercial infant cereal.
CONCLUSION: Exclusive breastfeeding (EBF) during the first 6 months of life was a rare practice in these low-income communities. Water, non-prescription medicines and formula milk and/or food were introduced at an early age.
Methods
The study was conducted from February to August 2011 in Avian Park and Zwelethemba in Worcester, an urban town in the Western Cape. Worcester is situated roughly 100 km east of Cape Town. Both communities are low-income settings and have formal and informal housing sections.[17] This study was conducted according to the Declaration of Helsinki guidelines and all procedures involving human participants were approved by the Committee for Human Research, Stellenbosch University, Cape Town. Written informed consent was obtained from all participants.
Quantitative component
A cross-sectional community-based study was performed with simple randomly selected households. Streets were numbered and selected using a computer-generated random selection table. An equal number of houses (n=6) from every randomly selected street (n=34) was included. Avian Park and Zwelethemba both had one informal area. These informal areas were divided into blocks to represent streets. If not enough households within a street or block qualified, another street or block was randomly selected and the process was repeated. Participants were included if they were the primary caregivers of infants <6 months old, spoke one of the three languages of the area (isiXhosa, Afrikaans and English), and had lived in the area for at least 5 years. A trained fieldworker conducted the interview in a private room or section of the participant's house using a structured questionnaire. The questionnaire was adapted by the researcher from questionnaires used in Africa by the Linkages Project.[18,19] It included sections on sociodemographic characteristics, infant feeding practices, infant feeding knowledge and support, and self-reported HIV status. Questions were close-ended and based on the participant's answer, prompts guided the fieldworker to the next relevant question. Content validity was reviewed by a panel of experienced nutrition professionals and face validity was tested during a pilot study prior to the study. Data were analysed with Statistica (version 10). Distributions of variables were presented with histograms. Medians or means were used as the measure of centre location for ordinal and continuous responses and standard deviations (SDs) as indicators of spread. The relation between two nominal variables was investigated with a x2 test and differences were considered to be significant at JK0.05. A 95% confidence interval was used to describe the estimation of unknown parameters.
Breastfeeding improves child survival by protecting against morbidities while providing nutritional and psychosocial benefits.[1,2] The promotion of exclusive breastfeeding (EBF) for the first 6 months of life is estimated to be the most effective measure to save infants from morbidity and mortality in low-income settings.[2] Optimal infant feeding practices during the first 6 months of life are described as initiation of breastfeeding within the first hour after giving birth[3] and EBF for 6 months.[4] Complementary feeding should be introduced at the age of 6 months.[4,5]
Different feeding practices have been defined by the World Health Organization (WHO) (Table 1). Predominant, partial or no breastfeeding increase the risk for pneumonia and diarrhoea-related mortality when compared with EBF during the first 6 months of life. The absence of breastfeeding carries the highest risk.[6] Mixed feeding is also associated with an increased risk of HIV transmission through breastfeeding.[7] Despite its benefits, EBF remains a rare practice in South Africa (SA) and national rates are estimated at 6.8 - 8.3%.[8,9] Concurrently, infant and child mortality rates remain high.[10]

Giving only breastmilk and no water or food has been described as an alien concept,[11] counterintuitive and impractical[12,13] in African societies. In SA, fluids and food are introduced to infants as early as 2 - 4 weeks after birth.[12,14,15] Maize meal porridge is the most common type of food introduced in rural areas,[14-16] whereas commercial infant cereal is commonly introduced in urban areas.[12,15] Very few studies describe the infant feeding practices of mothers living in low-income areas of the Western Cape Province of SA, which handicaps proper planning of tailored intervention strategies. The objective of the study was to provide a detailed description of the infant feeding practices in a low-income community of the province during the first 6 months of life.
Qualitative component
Separate focus group discussions were held with mothers who breastfed exclusively or predominantly; mothers who breastfed partially; and those who did not breastfeed. Participants were purposively recruited by fieldworkers who went from door to door in different areas of the two communities. Focus group discussions were conducted according to the procedures outlined in the United States Department of Agriculture's (USDA) Community Food Security Assessment Toolkit.[20] Focus group guides with a written list of questions and probes were compiled by the researcher. These guides were available in isiXhosa, Afrikaans and English. Trained fieldworkers transcribed focus group discussions and translated the discussions to English where necessary. Fieldworkers worked in pairs and all transcriptions and translations were checked by the partner and rechecked by a senior fieldworker who managed the group. The researcher analysed and interpreted the final transcripts and notes. The information from each focus group was summarised into categories. Findings from focus groups with the same participant profiles were grouped into a cluster, e.g. mothers who breastfed partially. Similarities and differences within and between clusters were investigated.
Results
Sociodemographic results
One hundred and forty primary caregivers were interviewed using the structured questionnaire. All were female and the biological mother of the infant. Mothers had a mean±SD age of 26.4±6.8 years (range 15 -45). The infants' ages ranged from <1 month to 5 months (median 2.0; mean±SD 2.0±1.5). Two-thirds (66%; n=93) of the infants were younger than 3 months old. IsiXhosa (54%, n=75) and Afrikaans (35%; n=54) were the two main languages spoken with a significant difference (p<0.001) in first language between Avian Park (74% Afrikaans speaking) and Zwelethemba (82% isiXhosa speaking). Eighty-one per cent (n=112) of the participants were unmarried and 60% (n=84) lived without a male partner or husband. Ninety-one per cent (n=127) had attained a high school education level or higher and 73% (n=102) were unemployed. Most mothers had given birth at a government facility (96%; n=135). Focus group discussions were held with 65 mothers of infants younger than 6 months. The sociodemographic profiles of the participants are summarised in Table 2.
Breastfeeding initiation
Seventy-seven per cent (n=108) of the mothers had initiated breastfeeding and all but 5% (n=5) of these had done so within the first hour after giving birth. Maternal HIV infection exerted a significant influence on infant feeding choice (p<0.001). Nineteen (14%) mothers reported that they were HIV-positive and none of them breastfed. At the time of the interview, 10% (n=11) of the mothers who initiated breastfeeding had discontinued breastfeeding. Ten of these mothers had discontinued breastfeeding before their infants were 3 months old.
Breastfeeding practices
Six per cent (n=8) of the mothers breastfed exclusively at the time of the interview. Ninety-four per cent (n=132) applied suboptimal breastfeeding practices: 36% (n=51) breastfed predominantly, 27% (n=38) breastfed partially, and 31% (n=43) did not breastfeed. Mothers from Zwelethemba were more likely to breastfeed partially while mothers from Avian Park were more likely to breastfeed predominantly (p=0.001). There was also a correlation between first language and breastfeeding practices, with isiXhosa-speaking mothers more likely to give their infants food than Afrikaans-speaking mothers (p<0.001).
Fig. 1 illustrates the breastfeeding practice by infant age. The highest proportion of exclusively and predominantly breastfed infants were <1 month old and the highest proportion of partially breastfed infants were 2 months old.

Replacement feeding
All mothers who never initiated breastfeeding or who discontinued breastfeeding (31%, n=43) gave formula milk as replacement feed. These mothers all reportedly boiled the water before mixing the formula milk and used the scoop in the tin to measure level scoops of formula milk powder. According to their reports of how they reconstituted the formula milk, 45% (n=19) diluted the formula milk correctly, while 45% (n=19) overdiluted and 10% ( n =4) underdiluted the formula milk. Focus group discussions revealed that mothers overdiluted formula milk since they could only afford a limited number of tins per month and often relied on grants or other people for financial support. Some added cooked porridge or meelbol to the reconstituted formula milk to save milk. Meelbol is cake or bread flour that is scorched brown and cooked like soft porridge.
'That is why I say I mix it with the meelbol when we make it half, to come out with the tin of milk.' (Formula-feeding mother.)
Water, infant cereal or rooibos tea (indigenous, caffeine-free tea) was also given to infants if not enough formula milk was available.
'Since he doesn't drink the breast, he only drinks bottle and he doesn't get full from the bottle and there is not that much milk to give a bottle the whole day, then I found out that I must give him porridge and he got calmer because his stomach is now full.' (Formula-feeding mother.)
Some mothers reported that they prepared a flask of formula milk for the night. They advised those mothers who did not have a flask to prepare a big bottle of milk and to wrap a warm napkin around it to keep the milk warm. Others disagreed and alluded to the fact that formula milk should be drunk immediately.
Supplementation of non-nutritive liquids
Fig. 2 summarises the introduction of non-nutritive liquids. Ninety-one per cent (n=88) of the breastfeeding mothers reported that they gave their infants water, of whom 85% ( n=75) had started before their infants were 1 month old. Eighty-eight per cent (n=38) of the formula-feeding mothers reported that they gave their infants water, of whom 76% (n=29) had started before their infants were 1 month old. There was no significant difference between breastfeeding and formula-feeding mothers and the practice of giving water (p=0.673) or having done so before 1 month of age (p=0.359). Opinions on the practice of giving non-prescription medicines varied. In Zwelethemba, gripe water and herbal medicines were given by some mothers, while in Avian Park, giving gripe water and Lennon's Behoedmiddel (antacid) were reported more frequently. Gripe water and Lennon's Behoedmiddel are over-the-counter products marketed for treating wind, stomach ache, colic and diarrhoea in children.

Supplementation of nutritive liquids and/or food
Fig. 3 summarises the introduction of nutritive liquids and/or food. Thirty-nine per cent (n=38) of the breastfeeding mothers reported that they gave their infants nutritive liquids (including formula milk) and/or food, of whom 79% (n=30) had started before their infants were 3 months old. Fifty-three per cent (n=23) of the formula-feeding mothers reported that they gave their infants nutritive liquids (excluding formula milk) and/or food, of whom 70% (n=16) had started before their infants were 3 months of age. There was no significant difference between breastfeeding and formula-feeding mothers and the practice of giving nutritive liquids and/or food (p)=0.116) or having done so before 3 months of age (p=0.413).
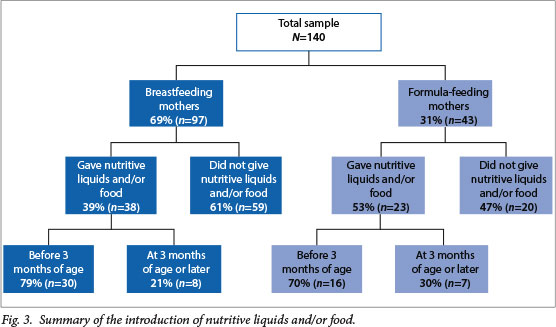
Commercial infant cereal and formula milk outweighed the use of any other supplementary nutritive liquids or food (Fig. 4). The 38 breastfeeding mothers and 23 formula-feeding mothers who gave supplementary nutritive liquids and/or food were allowed to report all products given. Sixty-two reports were received from breastfeeding mothers, with commercial infant cereal (n=28) and formula milk (n=27) reported most frequently.

Twenty-five reports were received from formula-feeding mothers, with commercial infant cereal (n=22) reported most frequently. In Zwelethemba, commercial infant food was also reported in focus group discussions while participants from Avian Park reported cooked soft porridge, starchy vegetables and rooibos tea. Meelbol was given by both communities but appeared to be a more common practice in Avian Park.
Discussion
The breastfeeding initiation rate of 77% was lower than rates seen in developing countries (95%),[6] the national rate in 2008 (88%)[21] and rates reported in rural and peri-urban areas of SA (88% - 100%).[12,14,16] Consistent with previous research and survey findings in SA,[8,15] most of the mothers who discontinued breastfeeding had done so before their infants were 3 months old. These rates of lower breastfeeding initiation and early discontinuation of breastfeeding are discouraging since breastfeeding is a key child survival strategy, especially in low-income settings.[1,2] Breastfeeding initiation was significantly influenced by maternal HIV infection and may improve after SA's adoption of the WHO recommendations that all HIV-positive pregnant women and breastfed infants should receive antiretroviral prophylaxis or treatment to support safer breastfeeding and child survival.[22] Similar to findings in Cape Town,[12] early initiation of breastfeeding was evident. Ninety-five per cent of the mothers who initiated breastfeeding had done so within the first hour after giving birth. This is a positive finding since early initiation is associated with increased breastfeeding success and the establishment of milk production.[23]
All mothers who never breastfed or who discontinued breastfeeding (31%; n=43) gave formula milk as replacement feed. However, despite the correct choice of product, formula-feeding practices were poor. Nearly half (45%; n=19) of the mothers overdiluted the milk and mothers reported deliberate overdilution to save milk. The practice of overdilution has been reported before[24,25] and is of concern since it lowers the energy density and nutrient concentration of formula milk, leading to decreased energy and nutrient intake.[26] Combined with poor hygiene practices such as mixing one big bottle for the day or keeping a flask of formula milk next to the bed at night, infants are put at risk of gastroenteritis, poor weight gain and malnutrition.[26,27]
In Avian Park and Zwelethemba, EBF was a rare practice. Only 6% (n=8) of the mothers breastfed exclusively at the time of the study. This is similar to the EBF rates in SA in 1998 (6.8%)[8] and 2003 (8.3%).[9] The early introduction of water, nutritive liquids and/ or food is well documented in SA.[12,14-16,26]
Similar to findings by Fjeld et al.,[28] mixed feeding was the conventional way to feed and, consistent with the findings of Sibeko et al.,[12] in a peri-urban area of Cape Town predominant breastfeeding was the most common method of feeding.
There was a significant difference in breastfeeding practices between the two communities. Partial breastfeeding was more common in Zwelethemba while predominant breastfeeding was more common in Avian Park (p=0.001). Both predominant and partial breastfeeding increase the risk for pneumonia and diarrhoea-related mortality.[6] While Buskens et al.[13] found that most mothers from SA used non-prescription medicines, very few accounts of this practice emerged from the quantitative reports. However, qualitative findings indicated that gripe water, Lennon's Behoedmiddel and herbal medicines were still used by some mothers and given to prevent or treat cramps, flatulence and jaundice.
Consistent with findings by Kruger et al.,[26] water was introduced within the first month of life and nutritive liquids and/or food within the first 3 months of life. Both breastfeeding and formula-feeding mothers supplemented their milk feeds. In 2011, Nor et al.[29] found that formula-feeding mothers also supplement their milk feeds, contrary to the belief that only breastfeeding mothers doubt their milk and therefore supplement feed. The practice of introducing water before 1 month of age (p=0.359) and nutritive liquids and/or food before 3 months of age (p=0.413) did not differ significantly between breastfeeding and formula-feeding mothers. Commercial infant cereal was the food most commonly given, similar to practices reported for urban areas[12,15] and dissimilar to practices reported for rural areas.[14-16] Second to infant cereal, breastfeeding mothers from Avian Park and Zwelethemba gave formula milk in addition to breastmilk.
Conclusion
Mothers from Avian Park and Zwelethemba applied suboptimal infant feeding practices. Breastfeeding initiation rates were lower than national rates,'211 while, similar to national figures, EBF was a rare practice.'8,91 Water, formula milk and commercial infant cereal were introduced at a young age. Formula-feeding practices proved to be poor due to a struggle to afford enough formula milk. SA has yet to improve significantly its infant and child mortality rates and alternative approaches to improving EBF rates are needed. We recommend testing different combinations of health-facility and community-based interventions, using rigorous research designs, to improve a practice embedded in traditional beliefs and conventional systems.
Acknowledgements. We thank the Stellenbosch University HOPE Project (Food Security Initiative) for the financial and administrative support that enabled this research to be undertaken. We also thank the fieldworkers and participants for their contributions to the success of the study.
References
1. World Health Organization Collaborative Study Team on the Role of Breastfeeding on the Prevention of Infant Mortality. Effect of breastfeeding on infant and child mortality due to infectious diseases in less developed countries: a pooled analysis. Lancet 2000;355:451-455. [http://dx.doi.org/10.1016/S0140-6736(00)82011-5] [ Links ]
2. Jones G, Steketee RW, Black RE, et al. How many child deaths can we prevent this year? Lancet 2003;362:65-71. [http://dx.doi.org/10.1016/S0140-6736(03)13811-1] [ Links ]
3. Edmond KM, Zandoh C, Quigley MA, et al. Delayed breastfeeding initiation increases risk of neonatal mortality. Pediatrics 2006;117:e380-e386. [http://dx.doi.org/10.1542/peds.2005-1496] [ Links ]
4. Kramer MS, Kakuma R. Optimal duration of exclusive breastfeeding. Cochrane Database of Systematic Reviews 2012;8:CD003517. [http://dx.doi.org/10.1002/14651858.CD003517.pub2] [ Links ]
5. Lanigan JA, Bishop JA, Kimber AC, et al. Systematic review concerning the age of introduction of complementary foods to the healthy full term infant. Eur J Clin Nutr 2001;55:309-320. 'http://dx.doi.org/10.1038/sj.ejcn.16011681 [ Links ]
6. Black RE, Allen LH, Bhutta ZA, et al. Maternal and child undernutrition: Global and regional exposures and health consequences. Lancet 2008;371:243-260. [http://dx.doi.org/10.1016/S0140-6736(07)61690-0] [ Links ]
7. Coovadia HM, Rollins NC, Bland RM, et al. Mother-to-child transmission of HIV-1 infection during exclusive breastfeeding in the first 6 months of life: An intervention cohort study. Lancet 2007;369:1107-1116. [http://dx.doi.org/10.1016/S0140-6736(07)60283-9] [ Links ]
8. National Department of Health, Medical Research Council, Measure DHS. South Africa Demographic and Health Survey 1998. Calverton, MD: Measure DHS, 2002. http://www.measuredhs.com/publications/publication-FR131-DHS-Final-Reports.cfm (accessed 27 October 2013). [ Links ]
9. National Department of Health, Medical Research Council, OrcMacro. South Africa Demographic and Health Survey 2003. Pretoria: DoH, 2007. http://www.measuredhs.com/pubs/pdf/FR206/FR206.pdf (accessed 27 October 2013). [ Links ]
10. Statistics South Africa. Millennium Development Goals. Country Report 2010. http://www.statssa.gov.za/news_archive/Docs/MDGR_2010.pdf (accessed 27 October 2013). [ Links ]
11. Magoni M, Giuliano M. Authors' response to "HIV and infant feeding: A complex issue in resource-limited settings" by Becquet and Leroy, to the letter to the editors by Coutsoudis et al., and to "Increased risk of infant HIV infection with early mixed feeding" by Piwoz and Humphrey. AIDS 2005;19:1720-1721. [ Links ]
12. Sibeko L, Dhansay MA, Charlton CE, et al. Beliefs, attitudes and practices of breastfeeding mothers from a peri-urban community in South Africa. J Hum Lact 2005;21:31-38. [http://dx.doi.org/10.1177/0890334404272388] [ Links ]
13. Buskens I, Jaffe A, Mkhatshwa H. Infant feeding practices: Realities and mindsets of mothers in Southern Africa. AIDS Care 2007;19:1101-1109. 'http://dx.doi.org/10.1080/095401207013364001 [ Links ]
14. Mamabolo RL, Alberts M, Mbenyane GX, et al. Feeding practices and growth of infants from birth to 12 months in the central region of the Limpopo province of South Africa. Nutrition 2004;20:327-333. [http://dx.doi.org/10.1016/j. nut.2003.11.011] [ Links ]
15. Steyn NP, Badenhorst CJ, Nel JH, et al. Breastfeeding and weaning practices of Pedi mothers and the dietary intakes of their preschool children. South African Journal of Food Science and Nutrition 1993;5:10-13. [ Links ]
16. Mushapi LF, Mbhenyane XG, Khoza LB, et al. Infant-feeding practices of mothers and the nutritional status of infants in the Vhembe District of Limpopo Province. S Afr J Clin Nutr 2008;21:36-41. [ Links ]
17. Breede Valley Local Municipality. Integrated Development Plan 2007-2012. Second Generation Review 4, 2011/2012. http://www.breedevallei.gov.za/bvmweb/images/IDP/IDP%202011%20-%202012.pdf (accessed 27 October 2013). [ Links ]
18. Academy for Educational Development, Linkages Project. Tanzania Integrated PMTCT Baseline Survey: Questionnaire for Use with Mothers of Infants Less Than 12 Months Old. LINKAGES, 2005. http://www.linkagesproject.org/publications/index.php?series=12 (accessed 27 October 2013). [ Links ]
19. Academy for Educational Development, Linkages Project (Zambia). Ndola Demonstration Project (NDP): Community-based Survey for Use with Mothers of Infants Age 0 to Less Than 6 Months Old. LINKAGES, 2001. http://www.linkagesproject.org/publications/index.php?series=12 (accessed 27 October 2013). [ Links ]
20. Cohen B. USDA Community Food Security Assessment Toolkit. Electronic publication from the Food Assistance and Nutrition Research Program No. (EFAN-02-013). USA: United States Department of Agriculture, 2002. http://www.ers.usda.gov/publications/efan02013/efan02013fm.pdf (accessed 27 October 2013). [ Links ]
21. Shisana O, Simbayi LC, Rehle T, et al. South African National HIV Prevalence, Incidence, Behaviour and Communication Survey, 2008: The Health of our Children. Cape Town: HSRC Press, 2010. http://www.hsrcpress.ac.za/product.php?productid=2279&cat=0&page=1&featured (accessed 27 October 2013). [ Links ]
22. National Department of Health, South Africa. South Africa National AIDS Council. Clinical Guidelines: PMTCT (Prevention of Mother-to-Child Transmission). Pretoria: Department of Health, South Africa, 2010. http://www.sahivsoc.org/upload/documents/NDOH_PMTCT.pdf (accessed 27 October 2013). [ Links ]
23. World Health Organization. Evidence for the Ten Steps to Successful Breastfeeding. Geneva: World Health Organization, 1998. http://whqlibdoc.who.int/publications/2004/9241591544_eng.pdf (accessed 27 October 2013). [ Links ]
24. Thairu LN, Pelto GH, Rollins NC, Bland RM, Ntshangase N. Sociocultural influences on infant feeding decisions among HIV infected women in rural KwaZulu-Natal, South Africa. Maternal and Child Nutrition 2005;1:2-10. [http://dx.doi.org/10.1111/j.1740-8709.2004.00001.x] [ Links ]
25. Faber M, Oelofse A, Kriek JA, Benade AJS. Breastfeeding and complementary feeding practices in a low socio-economic urban and a low socio-economic rural area. South African Journal of Food Science and Nutrition 1997;9:43-51. [ Links ]
26. Kruger R, Gericke GJ. A qualitative exploration of rural feeding and weaning practices, knowledge and attitudes on nutrition. Public Health Nutr 2003;6:217-223. [http://dx.doi.org/10.1079/PHN2002419] [ Links ]
27. Trahms CM, McKean KN. Nutrition during infancy. In: Mahan LK, Escott-Stump S, eds. Krause's Food Nutrition Therapy. USA: WB Saunders Company,2008:199-221. [ Links ]
28. Fjeld E, Siziya S, Katepa-Bwalya M, et al. 'No sister, the breast alone is not enough for my baby' a qualitative assessment of potential and barriers in the promotion of exclusive breastfeeding in southern Zambia. Int Breastfeed J 2008;3:26-37. [http://dx.doi.org/10.1186/1746-4358-3-26] [ Links ]
29. Nor B, Ahlberg BM, Doherty T, et al. Mothers' perceptions and experiences of infant feeding within a community-based peer counselling intervention in South Africa. Maternal and Child Nutrition 2012;8:448-458. [http://dx.doi.org/10.1111/j.1740-8709.2011.00332.x] [ Links ]
 Correspondence:
Correspondence:
C Goosen
(charlene.goosen@westerncape.gov.za)














