Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Child Health
versión On-line ISSN 1999-7671
versión impresa ISSN 1994-3032
S. Afr. j. child health vol.8 no.2 Pretoria may. 2014
RESEARCH
Profile of babies born before arrival at hospital in a peri-urban setting
N ParagI; N H McKerrowII; F NabyIII
IMB ChB, MBA; Division of Emergency Medicine, Pietermaritzburg Metropolitan Hospitals Complex, and Division of Emergency Medicine, University of KwaZulu-Natal, Durban, South Africa
IIMB ChB, BA, DCH (SA), FCPaed (SA), MMed Paed; KwaZulu-Natal Provincial Department of Health, and Department of Paediatrics, University of KwaZulu-Natal, Durban, South Africa
IIIMB ChB, DCH (SA), FCPaed (SA); Department of Paediatrics, Pietermaritzburg Metropolitan Hospitals Complex, and Department of Paediatrics, University of KwaZulu-Natal, Durban, South Africa
ABSTRACT
BACKGROUND: Babies born before arrival (BBAs) at hospital constitute a special group at risk of high morbidity and mortality.
OBJECTIVE: We conducted a 12-month retrospective review to describe maternal and neonatal characteristics of BBAs, and their outcomes compared with babies born in the state health sector.
METHODS: Using case-control sampling, all babies born outside a health facility and who presented to hospital within 24 hours of life were included and compared to the next in-hospital delivery occurring immediately after each BBA presented.
RESULTS: During the period reviewed, 135 BBAs (prevalence 1.8%) presented; 71% after hours with most deliveries occurring at home (73.8%). There was no birth attendant present at 70.5% of deliveries. Average birth weights were similar (2.86 kg in the BBA group, 95% confidence interval (CI) 2.73 - 2.95; 2.94 kg in the control group, 95% CI 2.78 - 3.02), but significantly more preterm babies were found in the BBA group (23% v. 9%, respectively; p<0.0001). Admitted BBAs had significantly lower average weights than those who were not admitted (2.19 kg v. 2.96 kg, respectively; p<0.0001). No significant differences were found when maternal age, parity, co-morbidities and distance from the hospital were compared. There were significantly more unbooked mothers in the BBA group (23.0% v. 6.7%, respectively; p<0.0001). Only 54.40% of the admitted BBAs' mothers had booked antenatally, compared with 78.89% of mothers whose babies were discharged. Admission and complication rates were similar between the groups, but average length of stay was longer in admitted BBAs compared with controls.
CONCLUSION: The prevalence of BBAs in this study is comparable to that in other developing countries, and is associated with poor antenatal attendance, prematurity, delay in presentation to hospital and lengthier hospital stays. These factors have implications for prehospital care of newborns and access to maternal and child healthcare in general.
It is estimated that just over 90% of births in South Africa (SA) occur within the health sector under the supervision of a skilled health professional. [1] Babies born outside the health sector fall into one of two groups: planned home births in a setting prepared and attended by trained health professionals; and unplanned deliveries without the attendance of skilled personnel. The latter group of babies born before arrival (BBAs) at hospital is more prevalent in developing and less-developed countries, and constitutes a special group with regard to mortality and morbidity. Given the high neonatal mortality rate in SA (19/1 000 live births in 2009'[2]), it is important to identify whether BBAs are a contributory factor.
The global BBA prevalence is poorly documented. The incidence varies (0.1 - 0.3%) in developed countries'[3,4] and rises exponentially in lesser-developed nations to >50% in countries such as India'[5] and southern Ethiopia.'[6] SA has a relatively high BBA rate, with National Department of Health data showing a prevalence of 5.4% in 2009 -the highest documented incidence being in KwaZulu-Natal (KZN) (5.7%) and Gauteng (5%) provinces.[1]
Prior studies have recognised the significant morbidity and mortality associated with BBAs,'[7-9] including hypothermia, hypo-glycaemia, lower birth weight, neonatal sepsis and a greater likelihood of admission to an intensive care unit.'[7,10-12] Recognised risk factors include low maternal age, high parity, low education level, poor access to transport and healthcare,'[12-16] and poor antenatal attendance.'[10,14,16] In addition, poverty, a rural lifestyle, and unwanted and teenage pregnancies are all expected to contribute to the prevalence of BBAs in SA.
This study was conducted at Edendale Hospital, a peri-urban, regional hospital in the KZN Midlands, to profile BBAs and factors giving rise to BBAs, and to describe the clinical presentation, management and outcomes of these babies.
Methods
We conducted a retrospective chart review of BBAs who presented to Edendale Hospital during the 12-month period from 1 July 2010 to 30 June 2011, using a case-control sampling strategy. BBAs were identified from the labour ward and neonatal nursery admissions registers. The clinical records for each mother-baby pair were retrieved from the medical records department of the hospital. All babies born outside a health facility and who presented to Edendale Hospital within the first 24 hours of life were included in the study. The control group comprised the in-hospital deliveries that followed immediately after the presentation of each BBA, and included normal vaginal births and babies delivered by caesarean section. Babies referred from other health facilities and BBAs who were >1 day old were excluded. Ethical approval for the study was obtained from the Biomedical Research and Ethics Committee of the University of KZN.
Data were extracted from the clinical records into an MS-Excel spreadsheet and subsequently imported to the statistical software SPSS (version 20) for analysis. The χ2 test was used where appropriate and p<0.05 was used in the study.
Results
During the study period, 135 BBAs were admitted to Edendale Hospital and these were matched with 126 controls. The discrepancy between the number of cases and controls resulted from two BBAs sharing a control when they were admitted sequentially with no intervening in-hospital delivery. Clinical records were retrieved for all BBAs but only 119 controls, resulting in 254 cases being included in the study.
As this was a retrospective study, there was a high level of missing data and only 13 cases had a complete record, defined as a record containing all the information required in the data collection tool, including a full antenatal history, circumstances surrounding the birth and birth history, measured physiological parameters and systemic examination findings, and the clinical outcome. Most records did not document the babies' temperature (94.9%), almost half (44.9%) did not record the blood glucose level and in 12 cases there was no record of the outcome of the hospital admission.
Table 1 portrays the characteristics of the two groups. Although there was a higher proportion of male babies in the control and female babies in the sample group, this was not significant. The average birth weight was similar in both groups: 2.86 kg (95% confidence interval (CI) 2.73 - 2.95) in the sample and 2.94 kg (95% CI 2.78 - 3.02) in the control group. Most babies (80.3%) were of normal weight (2.5 - 4.0 kg); however, there were significantly more preterm babies in the sample group than in the control group (23% v. 9%, respectively; p<0.0001).
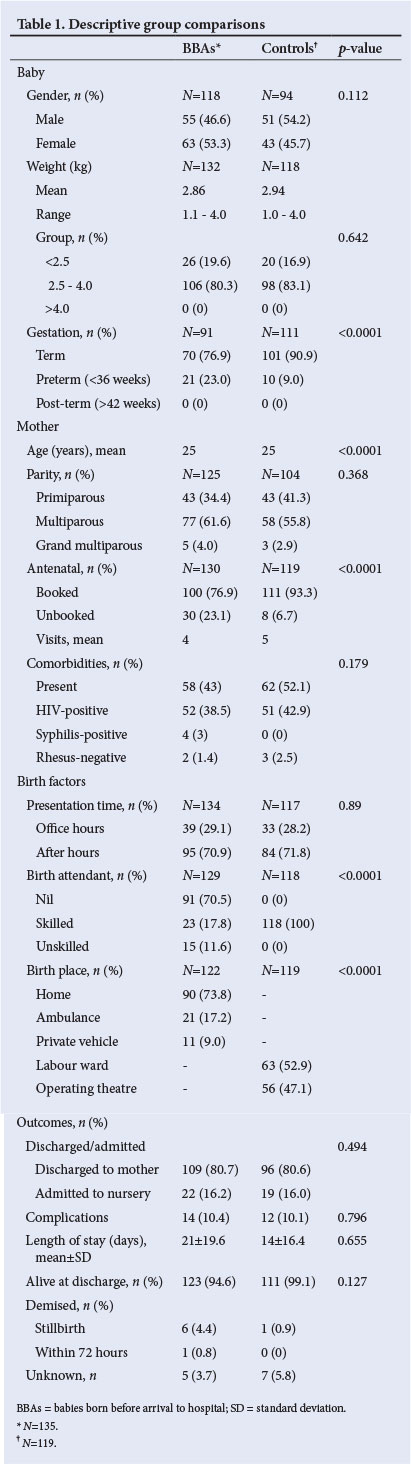
The mean age of 25 years was identical for the mothers in both groups, with a similar age range from 14 - 48 years in the sample and 15 - 40 years in the control group. Forty-five women (17.7%) in the study were below 18 years of age (23 in the BBA group and 22 in the control group) and 29 women (11.4%) in this study were over 35 years of age. There was a predominance of multiparous women (53.1%) and although most (83.1%) mothers had booked antenatally there were significantly fewer unbooked mothers in the control group (6.7% v. 23%; p<0.0001). The mean number of antenatal visits was 5 and 4 in the control and BBA groups, respectively.
Although there was no obvious difference in the morbidity of mothers in either group, 47.2% (n=120) ofthe women in this study had one or more comorbidity, the most prevalent being HIV infection (n=103). Less common comorbid factors included hypertensive disorders (n=12), Rhesus negativity (n=4), anaemia (n=2), pyelonephritis (n=1) and mental disability (n=1).
Most BBAs (71%) presented after hours (16h00 - 07h00). The majority of these deliveries occurred at home (73.8%) with a small proportion occurring en route to hospital (26.2%; 21 in an ambulance and 11 in a private vehicle). There was no birth attendant present at 70.5% (n=91) of BBA deliveries, while 23 (17.8%) had a skilled (emergency medical response crew member or nurse) and 15 (11.6%) had an unskilled (neighbour or relative) birth attendant. A similar proportion of women, 45% (n=60) in the BBA group and 37% (n=44) in the control group lived more than 15 km from the hospital. Almost half of the control group (47%) were delivered via caesarean section.
The clinical outcomes between the two groups were similar, with 41 babies requiring admission (22 BBAs and 19 controls) to the neonatal nursery. The most frequent reasons for admission were very low birth weight, neonatal jaundice and respiratory distress syndrome. Other reasons included septicaemia, hypoglycaemia, anaemia and patent ductus arteriosus. There was no significant difference in the number requiring admission (p=0.494), nor in the complication rates (14 BBAs v. 12 controls; p=0.796) between the two groups. Aspiration pneumonia, respiratory distress, apnoeic spells, hypoglycaemia and jaundice were recorded complications. The average length of stay was 7 days longer for admitted babies in the BBA group.
A total of eight deaths were identified in this study. Six BBAs were dead on arrival at hospital and one in-hospital delivery was stillborn. There was one early neonatal death in the BBA group.
The general condition and initial resuscitation performed on the two groups of babies is presented in Table 2.
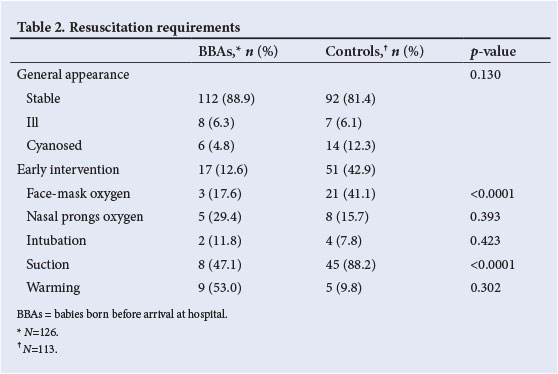
Early intervention was required for 68 of the babies in the study; the majority in the control group (p<0.0001). This higher rate of early intervention in the control group is anticipated, as there is immediate care available in hospital. A mean time delay of 169 minutes from delivery to presentation at hospital was found in the BBA group. Most of the babies (80.3%) were stable at first assessment, and in the majority of cases early intervention was limited to suctioning or face mask oxygen. Although only 17 BBAs required resuscitation, a significant proportion of these required either suctioning (47.1%) or warming, indicating a need for emergency medical assistance for these babies.
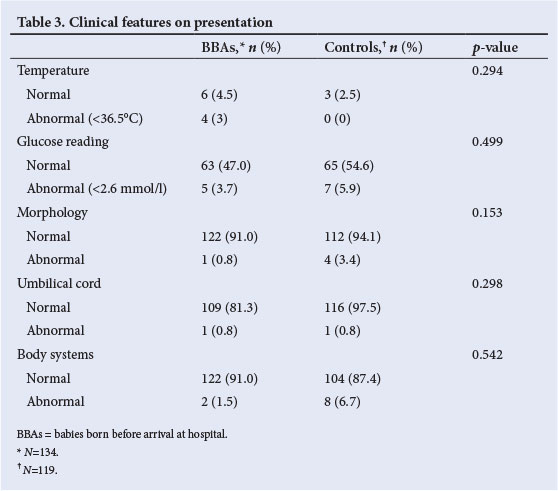
Table 3 shows the clinical features of the babies on arrival at hospital. Glucose readings were poorly documented, with absent data in 49.3% of the BBAs and 39.5% of the in-born babies. The temperature on arrival was very poorly documented, with only ten BBAs and three in-born babies having had a temperature recorded. These important vital signs were the most important contributors to missing information in the medical records of all the cases included in this study. There were more babies with an abnormal morphology in the control group (3.4% v. 0.8%), and also more systemic abnormalities detected in this group (6.7% v. 1.5%). The most frequent abnormalities observed were central nervous system hypoactivity and tachypnoea (respiratory rate more than 60 breaths per minute). Overall, there were no significant differences in the clinical features of the babies in the two groups.
A comparison of the admitted with the non-admitted babies in the BBA group is shown in Table 4.
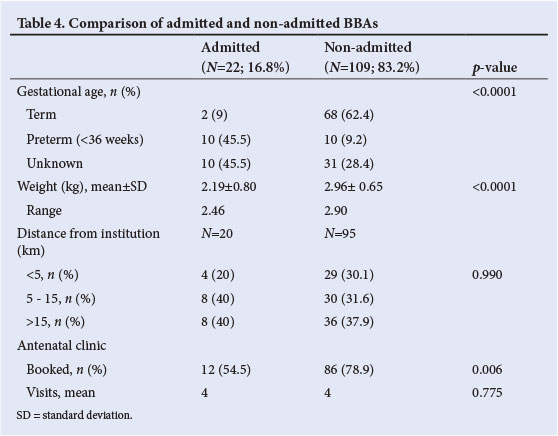
Twenty-two of the 135 BBAs required admission to the neonatal nursery. Reasons for admission included respiratory distress (n=9), neonatal jaundice (n=7), very low birth weight (n=5) and hypoglycaemia (n=3). Six of the admitted BBAs required neonatal intensive care during their admission. The average weight of the admitted babies was significantly less than that of the babies who did not require admission (2.19 kg v. 2.96 kg; p<0.0001). The mean gestational age in the BBA group was 36.5 weeks (standard deviation (SD) 2.33; variance 5.36). Although 15.26% (n=20) of BBAs were born preterm, only half required admission and these accounted for 45.5% of the BBAs who were admitted. The area of residence or the distance from the institution had no influence on the outcome of the BBA babies, with similar rates of admission regardless of where they came from. Only 54.5% of mothers of the admitted BBAs had booked antenatally, as compared to 78.9% of mothers whose babies were discharged; however, the mean number of antenatal visits remained constant.
Discussion
The prevalence rate of BBAs over the study period was 1.8%, which is comparable to rates in developed countries (0.1 - 2.2%),'3,4,101 but significantly lower than previously documented in the province (5.7%) and in SA in general (5.4%).'11 This may reflect the fact that this study was conducted in a peri-urban setting, with easier access to transport as well as the ongoing focus on the decentralisation of healthcare, leading to improved access to healthcare facilities.'171 Interestingly, however, most deliveries before arrival occurred at night, which may reflect poorer access to transport after hours.
The place of birth of BBAs was predominantly at home, with a small proportion occurring en route to hospital, which is similar to previous reports.[10] Bhoopalam[10] identified an increasing distance from hospital as a significant risk factor for the occurrence of BBAs, which was also found in this study where 45% of mothers delivering BBAs lived more than 15 km from the hospital.
The majority of babies in the BBA group had a multiparous mother, and as observed in previous studies, women of higher parity are more likely to deliver before arrival at a hospital due to the shorter duration of the second stage of labour and higher incidence of prelabour spontaneous rupture of membranes.[7,15] The observations from previous studies that found that women who delivered before arrival at hospital were more likely to be unbooked and of greater parity.[7,14] were also found in this study. Significantly fewer mothers of BBAs attended antenatal clinic, and this is possibly associated with greater risks as the opportunities for health education and early detection of complications are lost.[12] This could also be a reason for the higher stillbirth rate seen in the BBA babies.
The average birth weight of the BBAs was only marginally lower than babies born in hospital, but a larger proportion were preterm (born before 36 completed weeks' gestation).
Prematurity appears a consistent finding in studies of BBAs,'11,12,151 and is considered to be due to the unanticipated onset of labour. Hypothermia, hypoglycaemia, prematurity, sepsis and alterations in haemoglobin are complications found more frequently in BBAs than in those babies born in hospital.[8,11,12,15]
In a review of studies from the US, UK and Europe, which explored the presence of emergency medical services at unplanned births before arrival at hospital, the most frequent neonatal complication found (in 8 of 14 studies) was hypothermia, regardless of gestational age.'181 Unfortunately, temperature was very poorly documented in the babies in this study. According to standard clinical practice at the institution, well babies born in hospital do not routinely have temperature measured, but all BBAs are expected to have temperature and glucose readings done on presentation at hospital. The low rate of clinical observations (glucose and temperature) for anticipated complications could reflect a poor quality of care of these babies, as these vital signs are early warnings to possible critical illnesses in the newborn baby. Hypoglycaemia was also poorly documented, and this complication not only affects immediate survival but also predicts abnormal outcome in terms of the neurobiological risk score.[19] Failure to document these vital signs in BBAs indicates a failure to anticipate and hence treat these historically common complications in this group of babies, and is an indicator of poor neonatal care for this high-risk group.
The BBAs who required admission were significantly smaller than those who were discharged immediately, and the complications of prematurity are likely contributors to this need for inpatient care. This study did not show a higher rate of overall admissions of BBAs compared to babies born in hospital, which differs from the experience of Rodie'141 and Spillane[15]et al., who reported that in a developed setting more BBA neonates than hospital-born babies require admission to a neonatal unit.[14,15] In these studies, prematurity was the main contributing factor to this.
In keeping with previous observations, the BBAs in this study who required admission had to stay longer in hospital than the control group.[7,11] Considering the admission rate to be similar between the groups, this requirement may be more a function of prematurity and low birth weight than of the babies having been born before arrival to hospital.
Conclusion and recommendations
This study has demonstrated a decline in the prevalence of BBAs. It has also identified significant risk factors for the occurrence of BBAs, namely poor antenatal attendance and preterm delivery. Admission and complication rates were similar between BBA and hospital-born groups, but BBAs had significantly lower birth weights and lengthier hospital stays than in-born babies.
The prevalence of BBAs in this study is comparable to global figures in other developing countries, and similar risk factors for their occurrence have been identified (poor antenatal attendance, prematurity and a delay in presentation to hospital). These factors have implications for the prehospital care of newborns and access to maternal and child healthcare in general.
This study also identified a failure of clinicians to anticipate complications associated with BBAs and to instigate the appropriate clinical care, particularly the very poor documentation of temperature and glucose readings, two of the most important clinical observations to identify critically ill patients. This finding has implications for clinical training of healthcare workers and the need for protocol development for the acute assessment of these babies, both in the prehospital environment and upon arrival at hospital.
References
1. District Health Information System Database. National Department of Health. http://hisp.org (accessed 1 June 2012). [ Links ]
2. United Nations Children's Fund (UNICEF). Information by Country: South Africa - Statistics 2009. http://www.unicef.org/infobycountry/southafrica-statistics.html#73 (accessed 12 June 2011). [ Links ]
3. Viisainen K, Gissler M, Hartikainen AL, Hemminki E. Accidental out-of-hospital births in Finland: Incidence and geographical distribution 1963 -1995. Acta Obstet Gynecol Scand 1999;78:372-378. [http://dx.doi.org/10.1034/j.1600-0412.1999.780505.x] [ Links ]
4. Scott T, Esen UI. Unplanned out of hospital births - who delivers the babies? Ir Med J 2005; 98:70-72. [ Links ]
5. Kodkany BS, Derman RJ, Goudar SS. Initiating a novel therapy in preventing postpartum hemorrhage in rural India: a joint collaboration between United [ Links ]
States and India. Int J Fertil Women's Med 2004;49:91-96. [http://dx.doi.org/10.1016/j.ijgo.2005.12.009]
6. Sibley L, Buffington ST, Haileyesus D. The American College of Nurse-Midwives' Home-Based Lifesaving Skills Program: A review of the Ethiopia field test. J Midwifery Women's Health 2004;49:320-328. [http://dx.doi.org/10.1016/j.jmwh.2004.03.013] [ Links ]
7. Di Benedetto MR, Piazze JJ, et al. An obstetric and neonatal study on unplanned deliveries before arrival at hospital. Clin Exp Obstet Gynecol 1996; 23(2):108-111. [ Links ]
8. Bateman DA, O'Bryan L, Nicholas W, Heagarty MC. Outcome of unattended out-of-hospital births in Harlem. Arch Pediatr Adolesc Med 1994;148(2):147-152. [http://dx.doi.org/10.1001/archpedi.1994.02170020033005] [ Links ]
9. Ballot DE, Chirwa TF, Cooper PA. Determinants of survival in very low birth weight neonates in a public sector hospital in Johannesburg. BMC Pediatrics 2010:10:30. [http://dx.doi.org/10.1186/1471-2431-10-30] [ Links ]
10. Bhoopalam PS, Watkinson M. Babies born before arrival at hospital. BJOG 1991;98:57-64. [http://dx.doi.org/10.1111/j.1471-0528.1991.tb10312.x] [ Links ]
11. Sirimai K, Titapant V, Roongphornchai S. Morbidity and mortality from birth before arrival at Siriraj Hospital. J Med Assoc Thai 2002;85(12):1258-1263. [ Links ]
12. Sehgal A, Roy MS, Dubey NK, Jyothi MC. Factors contributing to outcome in newborns delivered out of hospital and referred to a teaching institution. Indian Pediatr 2001;38:1289-1294. [ Links ]
13. Bhat BA, Suri K, Gupta B. A clinico-epidemiological evaluation of infants born before arrival at hospital. Ann Saudi Med 2000;20(5-6):483-485. [ Links ]
14. Rodie VA, Thomson AJ, Norman JE. Accidental out-of-hospital deliveries: an obstetric and neonatal case control study. Acta Obstet Gynecol Scand 2002; 81(1):50-54. [http://dx.doi.org/10.1046/j.0001-6349.2001.00420.x] [ Links ]
15. Spillane H, Khalil G, Turner M. Babies born before arrival at the Coombe Women's Hospital, Dublin. Ir Med J 1996;89(4):146. [ Links ]
16. Department of Health, Medical Research Council, OrcMacro. South Africa Demographic and Health Survey 2003. Pretoria: Department of Health, 2003. [ Links ]
17. Blaauw D, Penn-Kekana L. Maternal Health. In: Fonn S, Padarath A, (eds). South African Health Review 2010. Durban: Health Systems Trust, 2010. [ Links ]
18. McLelland GE, Morgans AE, McKenna LG. Involvement of emergency medical services at unplanned births before arrival to hospital: A structured review. Emerg Med J 2013 Feb. Published online at http://emj.bmj.com/content/early/2013/02/15/emermed-2012-202309.abstract. Accessed 24 October 2013. [http://dx.doi.org/10.1136/emermed-2012-202309] [ Links ]
19. Contractor CP, Leslie GI, Brown JR, Arnold J. Neonatal neuro biologic risk score. Indian Pediatr 1996;33:95-101. [ Links ]
 Correspondence:
Correspondence:
N Parag
(nivishaparag@yahoo.com)














