Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Child Health
versión On-line ISSN 1999-7671
versión impresa ISSN 1994-3032
S. Afr. j. child health vol.8 no.1 Pretoria feb. 2014
CASE REPORT
Rubinstein-Taybi syndrome: Dental manifestations and management
T S RobertsI; M ChettyII; L StephenI; M UrbanIII; K FieggenIV; P BeightonV
IBChD, MChD; Faculty of Dentistry, University of the Western Cape, Bellville, Cape Town, South Africa; University of the Western Cape/University of Cape Town Dental Genetics Clinic, Red Cross War Memorial Children's Hospital, Cape Town, South Africa
IIBSc, BChD, MChD; Faculty of Dentistry, University of the Western Cape, Bellville, Cape Town, South Africa; University of the Western Cape/University of Cape Town Dental Genetics Clinic, Red Cross War Memorial Children's Hospital, Cape Town, South Africa
IIIMB BCh, FCPaed (SA), MMed; Division of Molecular Medicine and Human Genetics, Faculty of Medicine and Health Sciences, Stellenbosch University, Parow, Cape Town, South Africa
IVMB ChB, FCPaed (SA); Division of Human Genetics, Faculty of Health Sciences, University of Cape Town, South Africa
VMD, PhD, FRCP Division of Human Genetics, Faculty of Health Sciences, University of Cape Town, South Africa; University of the Western Cape/University of Cape Town Dental Genetics Clinic, Red Cross War Memorial Children's Hospital, Cape Town, South Africa
ABSTRACT
Rubinstein-Taybi syndrome (RSTS) is an uncommon genetic disorder characterised by a typical facies, small stature, broad angulated thumbs and intellectual impairment. Dental changes are a minor, yet significant component of the condition. Craniofacial growth retardation in RSTS is frequently complicated by unerupted teeth, while dental caries is related to the inherent intellectual deficit. Dental problems necessitate interdisciplinary management in terms of oral surgery, conservative dentistry, periodontics and orthodontics. When affected individuals are unco-operative, certain dental procedures may warrant general anaesthesia. In these instances, dental and medical staff will combine their expertise to enhance the well-being of the patient. In addition, specific dental changes may alert the medical practitioner to the possible diagnosis of RSTS. In this article we document the oro-dental manifestations and review the oro-dental approach in the management of three patients with RSTS. Our experience in South Africa may be relevant to other countries at a similar stage of development.
The major manifestations of Rubinstein-Taybi syndrome (RSTS) (OMIM 180849), also referred to as the 'broad thumb-hallux syndrome' and 'multiple congenital anomalies/mental retardation syndrome', are a characteristic facies, broad thumbs and great toes, stunted stature and mental retardation. Following the initial documentation by Rubinstein and Taybi (1963),[1] the condition that bears their names has been extensively reviewed by Hennekam et al.[2] and Stevens.[3]
RSTS can be transmitted as an autosomal dominant trait, but the majority of cases are sporadic, as the intellectual compromise may preclude procreation. The condition is uncommon, with a population prevalence of 1:100 000 - 1:125 000.[4,5] According to Stevens,[3] the majority of reports of RSTS worldwide pertain to persons of Caucasian stock; to the best of our knowledge, the syndrome has not previously been reported in Africa.
Although the literature contains reports of more than 1 000 affected persons, the oro-dental features have been significantly under-reported. The palate, jaws and teeth are involved in RSTS, and a variety of abnormalities may occur in these regions.[6,7] Dental management may require a specialised, structured approach, within a protocol, for the overall care of the affected individual. In this article we document and describe three cases of RSTS and review the manifestations and dental management of this syndrome.
Case reports
The archives of the Division of Human Genetics, University of Cape Town (UCT), South Africa, contain case notes of 23 persons with RSTS seen since 1972, based on clinical and radiographic features. Molecular studies were not available at the time of diagnosis. Retrospective analysis of these cases revealed no mention of oro-dental manifestations, as these were overshadowed by the mental impairment and clinical features.
The three patients reported in this article were assessed by a multidisciplinary dental team from the University of the Western Cape (UWC), Bellville, Cape Town, and medical genetics staff from UCT.
Case 1
An affected white girl born in 1985 was first seen at the UWC-UCT Dental Genetic Clinic in 2003. Her mother reported an uneventful pregnancy followed by an emergency caesarean section because of fetal distress. Her non-consanguineous parents and her elder brother were unafected.
The girl was 'floppy' during infancy and her developmental milestones were delayed. Her intellectual compromise persisted during childhood, and special educational facilities were necessary. She wore a bib until the age of 5 years because of constant drooling. Enuresis persisted until puberty. In adolescence, her joints were hypermobile, and ligamentous laxity and instability of the left knee necessitated orthopaedic intervention. An opthalmological operation was undertaken in 2002 to rectify deviation of her right eye.
On examination at the age of 18 years, she had the characteristic facies of RSTS, notably a prominent forehead, microcephaly, down-slanting palpebral fissures, epicanthal folds, strabismus, a broad nasal bridge, a pear-shaped nose with the nasal septum extending below the alae, and a small oral opening (Fig. 1). Her hands appeared normal, but both big toes (halluces) were broad.

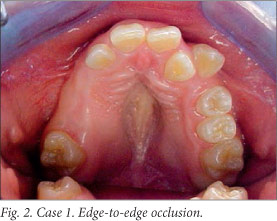
Intra-oral examination revealed a high-vaulted palate, and several teeth were absent from the oral cavity. Her malocclusion (Fig. 2) was characterised by edge-to-edge occlusion, a bilateral posterior cross-bite, a bilateral posterior open bite, and lack of posterior tooth support on the right side.
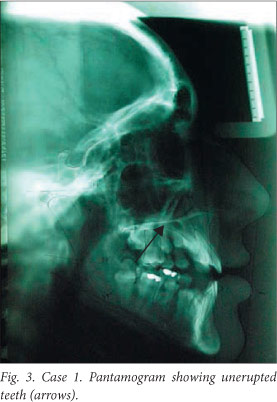
A pantomogram showed the clinically missing permanent teeth retained in the alveolar bone (Fig. 3). Analysis of the available jaw space failed to reveal any discrepancies that would affect the eruption of these teeth. Cephalometric analysis revealed a retrognathic mandible and maxilla with a high mandibular plane angle and cantered occlusal plane. The maxillary incisors had an angulation and inclination within the normal range, while the mandibular incisors were retroclined and retruded.
Routine chromosomal analysis did not reveal any abnormality. Molecular techniques, including fluorescence in situ hybridisation (FISH) testing and sequencing of the CREBBP gene, can be used to confirm the clinical diagnosis of RSTS, but are currently not available in South Africa.
Case 2
A South African black girl born in 2003 was diagnosed as having RSTS at 20 months of age and followed up regularly at Red Cross War Memorial Children's Hospital, Cape Town, until the age of 4 years. Her family history was negative.
She was born at term following a pregnancy complicated by hyperemesis gravidarum. She had no significant medical illnesses, but her developmental milestones were severely delayed: she started walking at 2 years of age and spoke her first words at 3 years of age.
Her growth was retarded with height below the third centile and weight on the third centile. She was microcephalic and had typical facial features of RSTS, including down-slanting palpebral fissures, a beaked nose with the columella extending below the alae nasae, a prominent lower lip and a grimacing appearance of the mouth. The palate was high-arched. The terminal phalanges of all fingers were broad, while both thumbs and halluces were strikingly broad. She had a slight pectus excavatum and mild thoracolumbar scoliosis. Radiological examination revealed six lumbar vertebrae.
The teeth were noted to be malaligned at 2½ years of age, and several required extraction for caries resulting from prolonged bottle-feeding (nursing caries). On follow-up one year later, several of the remaining teeth were carious.
At the age of 4 years, the patient had multiple carious teeth, associated with poor dental hygiene. Her dental age was within the normal range. Since several teeth in all four quadrants of her mouth required extraction, arrangements were made for this to be done under general anaesthesia.
Prophylactic scaling and polishing would be undertaken at the same time. The parents were presented with the treatment plan and given guidance concerning the importance of oral hygiene. However, they declined treatment.
Case 3
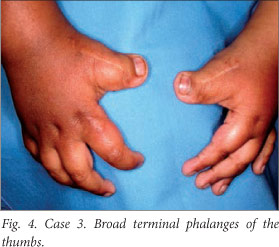
A boy of mixed ancestry and aged 7 years, previously diagnosed as having RSTS, was referred to the Faculty of Dentistry at Tygerberg Hospital, Parow, Cape Town, for dental assessment. He had the typical features of the syndrome, notably intellectual impairment, short stature, a bulbous nose and broad terminal phalanges of the thumb (Fig. 4) and halluces. No other family member was affected.
His developmental milestones were delayed and he had been bottle-fed until the age of 2 years. He started crawling at this stage and walked at the age of 4 years. By the age of 7 years he could only speak approximately 10 words and communication with him at the dental clinic was difficult. It was impossible to proceed with radiographic investigations due to his mental impairment.
Intra-oral examination revealed that he had a high-arched palate and several carious teeth. His dentition was otherwise unremarkable. He was a mouth breather and his oral hygiene was poor.
During the first visit, mother and child were given instruction in oral hygiene and his diet was analysed. The boy was not co-operative in the dental chair, but it was possible to apply topical fluoride to the teeth. Regular follow-up visits indicated that his oral health status had improved significantly. A finger brush was suggested for cleaning the maxillary teeth, as the gums in this area were very sensitive. Arrangements were made for conservative treatment and extractions of carious teeth under general anaesthesia. The boy returned to the dental clinic 4 years later when he was in the mixed dentition stage. Apart from poor oral hygiene and a few cavities, no additional dental anomalies were noted. The sequence of tooth eruption was within the normal range for his age. His extreme anxiety prevented any radiographs from being obtained.
Discussion
In 1957, Michail et al.[8] described a 7-year-old boy with the distinctive features of RSTS in a French orthopaedic journal. In 1963, unaware of the aforementioned report, Rubinstein and Taybi[1] documented the syndromic association of broad thumbs and toes with facial abnormalities, thereby delineating the condition that now bears their conjoined eponym.
A mutation in the CREBBP gene (OMIM 600140) at the chromosomal locus 16p13.3 is detectable by the FISH technique in about 15% of persons with RSTS (RSTS1). With sequence analysis, this figure rises to 30 -50%. In a minority of individuals, the EP300 gene (OMIM 602700) at 22q13 has been implicated (RSTS2).[9] Considerable intragenic heterogeneity has been recognised in both forms of RSTS. In general, the craniofacial abnormalities and intellectual impairment are more severe in RSTS1 than in RSTS2.[10]
The severity of the manifestations of RSTS is very variable, and the case reports presented in this article provide a perspective of the range of involvement. It is relevant that management, including dental measures, is determined by the severity, or otherwise of the feature in question. The main practical problem in RSTS is mental retardation, and affected persons are normally incapable of independent existence and adequate self-care. Guidelines for the general surveillance and medical management of the RSTS have been proposed by Wiley et al.[11]
Considerations pertaining to dental management include the use of general anaesthesia if cardiac or respiratory abnormalities are present. Possible challenges during intubation result from anterior positioning and mechanical inadequacies or weakening of the larynx, and there is a risk of aspiration pneumonia. Cardiac abnormalities and arrhythmias have been reported in RSTS,[11] and if present, require evaluation before conservative or invasive dental treatment. Skeletal and soft-tissue changes in the head and neck region resulting in upper-airway obstruction can lead to mouth breathing and recurrent pneumonia.
The oral features of RSTS have been reviewed extensively by Hennekam and Van Doorne[6] and Bloch-Zupan et al.,[7] and are mentioned by several other authors.[11-17] Dental talon cusps are present in a high proportion of persons with RSTS,[12] but this feature was absent in our patients. All three had high-arched palates - often associated with malocclusion and tooth malalignment. Hypo- and hyperdontia may also occur. Caries resulting from inadequate dental hygiene is frequent, and in older children may be the result of the intellectual disability and motor impairment that characterise the syndrome. Problems with feeding during early development could be the cause of the nursing caries in cases 2 and 3.
Optimal oral and dental health is of the utmost importance in the general well-being of a patient with RSTS. Good oral health enables problem-free assimilation and digestion of food, which translates to a physically healthy individual. Caries and periodontal disease affect quality of life. If individuals with RSTS cannot articulate coherently, they may suffer from dental pain for weeks or months. In turn, this may affect their eating habits, resulting in malnutrition and an impaired immune response. Bleeding gums may prevent caregivers or parents from continuing routine oral hygiene practices, and together with halitosis may result in social isolation and poor self-esteem.
Proposed management protocols
The dental treatment plan that we proposed for patient 1 encompassed 6-monthly follow-up visits for monitoring the eruption of the remaining teeth. As she showed no signs of a space discrepancy, surgical exposure and assisted eruption would have been unwarranted. Subsequent radiographs showed evidence of eruption with open root apices. Maxillary arch expansion for the correction of the bilateral posterior cross-bite was undertaken. In addition, the anterior teeth were levelled and aligned, where necessary, to facilitate the eruption of the canine and premolar teeth in their appropriate positions. A fixed lingual arch-wire was placed in the mandibular arch to maintain the space for the erupting canine and premolar teeth.
In view of her age and the developmental status of her dentition, patient 2 would ideally have been recalled at 6-monthly intervals to enable adequate monitoring of her growth and development.
Management of patient 3 was difficult because of the severity of his intellectual impairment. Extractions and conservative treatment were undertaken under general anaesthesia without complications. The boy returned to the dental clinic every 6 months for cleaning and prophylaxis.
Conclusion
The oro-dental complications of RSTS are important but neglected aspects of the disorder. On the basis of our experience in Cape Town it has become apparent that the multifaceted problems necessitate a team approach towards dental management and possible anaesthesia. Equally, in an environment where facilities may be suboptimal, multidisciplinary collaboration is crucial for efective management and for the well-being of the affected person.
Ethics approval
Ethics approval was obtained from the Human Research Ethics Committee, Faculty of Health Sciences, UCT.
Acknowledgements
Support for this project was received by PB from the South African Medical Research Council and the National Research Foundation.
References
1. Rubinstein JH, Taybi H. Broad thumbs and toes and facial abnormalities: A possible mental retardation syndrome. Arch Pediatr Adolesc Med 1963;105(6):588-608. [ Links ]
2. Hennekam RCM, Kranz ID, Allanson JE. Gorlin's Syndromes of the Head and Neck. 5th ed. New York: Oxford University Press, 2010:451-457. [ Links ]
3. Stevens CA. Rubinstein-Taybi Syndrome. GeneReviews: Genetic Disease Online Reviews at GeneTests-GeneClinics (database online). 2012. http://www.geneclinics.org (accessed 12 November 2012). [ Links ]
4. Hennekam RC, van den Boogaard MJ, Sibbles BJ, Van Spijker HG. Rubinstein-Taybi syndrome in the Netherlands. Am J Med Genet 1990;37(S6):17-29. [http://dx.doi.org/10.1002/ajmg.1320370604] [ Links ]
5. Marzuillo P, Grandone A, Coppola R, et al. Novel cAMP binding protein-BP (CREBBP) mutation in a girl with Rubinstein-Taybi syndrome, GH deficiency, Arnold Chiari malformation and pituitary hypoplasia. BMC Med Genet 2013;14(1):28. [http://dx.doi.org/10.1186/1471-2350-14-28] [ Links ]
6. Hennekam RC, Van Doorne JM. Oral aspects of Rubinstein-Taybi syndrome. Am J Med Genet 1990;37(Suppl 6):42-47. [http://dx.doi.org/10.1002/ajmg.1320370607]
7. Bloch-Zupan A, Stachtou J, Emmanouil D, Arveiler B, Griffiths D, Lacombe D. Oro-dental features as useful diagnostic tool in Rubinstein-Taybi syndrome. Am J Med Genet 2007;143A(6):570-573. [http://dx.doi.org/10.1002/ajmg.a.31622] [ Links ]
8. Michail J, Matsoukas J, Theodorou S. [Arched, clubbed thumb in strong abduction-extension & other concomitant symptoms.] Rev Chir Orthop Reparatrice Appar Mot 1957;43(2):142-146 (in French). [ Links ]
9. Roelfsema JH, Peters DJ. Rubinstein-Taybi syndrome: Clinical and molecular overview. Expert Rev Mol Med 2007;9(23):1-16. [http://dx.doi.org/10.1017/S1462399407000415] [ Links ]
10. Bartsh O, Kress W, Kempf O, Lechno S, Haaf T, Zechner U. Inheritance and variable expression in Rubinstein-Taybi syndrome. Am J Med Genet 2010;152(A):2254-2261. [http://dx.doi.org/10.1002/ajmg.a.33598] [ Links ]
11. Wiley S, Swayne S, Rubinstein J, Lanphear N, Stevens C. Rubinstein-Taybi syndrome and medical guidelines. Am J Med Genet 2003;119A(2):101-110. [http://dx.doi.org/10.1002/ajmg.a.10009] [ Links ]
12. Gardner D, Girgis S. Talon cusps: A dental anomaly in the Rubinstein-Taybi syndrome. Oral Surg 1979;47(6):519-521. [http://dx.doi.org/10.1016/0030-4220(79)90274-3] [ Links ]
13. Davidovic E, Eimerl D, Peretz B. Dental treatment of a child with Rubinstein-Taybi syndrome. Pediatr Dent 2005;27(5):385-388. [ Links ]
14. Freitas N, Imbronito C, La Scaloa C, Lotufo R, Pustiglion F. Periodontal disease in a Rubinstein-Taybi syndrome patient: Case report. Int J Paediatr Dent 2006;16(4):292-296. [http://dx.doi.org/10.1111/j.1365-263X.2006.00721.x] [ Links ]
15. Morales-Chávez MC. Dental management of a patient with Rubinstein-Taybi syndrome. Spec Care Dentist 2010;30(3):124-126. [http://dx.doi.org/10.1111/j.1754-4505.2010.00137.x] [ Links ]
16. McArthur R. Rubinstein-Taybi sydrome: Broad thumbs and great toes, facial abnormalities and mental retardation: A presentation of three cases. CMAJ 1967;96(8):462-466. [ Links ]
17. Gunashekhar M, Hameed MS, Bokhari SK. Oral and dental manifestations in Rubinstein-Taybi syndrome: Report of a rare case. Prim Dent Care 2012;19(1):35-38. [http://dx.doi.org/10.1308/135576112798990773] [ Links ]
 Correspondence:
Correspondence:
T S Roberts
(troberts@uwc.ac.za)














