Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Child Health
On-line version ISSN 1999-7671
Print version ISSN 1994-3032
S. Afr. j. child health vol.7 n.4 Pretoria Apr. 2013
RESEARCH
Outcomes of babies born before arrival at a tertiary hospital in Johannesburg, South Africa
M K BassingthwaighteI; D E BallotII
IMB ChB, MPH, DCH (SA); Department of Paediatrics and Child Health, University of the Witwatersrand and Charlotte Maxeke Johannesburg Academic Hospital, Johannesburg, South Africa
IIMB ChB, FCPaed (SA), PhD; Department of Paediatrics and Child Health, University of the Witwatersrand and Charlotte Maxeke Johannesburg Academic Hospital, Johannesburg, South Africa
ABSTRACT
BACKGROUND: Babies born before arrival (BBBAs) to hospital constitute a high-risk newborn population. The literature demonstrates that BBBAs have increased perinatal mortality and morbidity.
OBJECTIVES: To describe the maternal and neonatal characteristics of BBBAs presenting to Charlotte Maxeke Johannesburg Academic Hospital (CMJAH), South Africa, and assess whether they have increased morbidity and mortality compared with inborn babies.
METHODS: This was a matched case-controlled retrospective record review of newborns presenting to the neonatal unit at CMJAH between 1 January 2011 and 31 January 2013. BBBAs were matched 1:1 with the next consecutive inborn on birthweight category and gender.
RESULTS: A total of 356 neonates were analysed. BBBAs had higher mortality than inborn controls within the first 24 hours of hospital presentation (7.9% v. 3.9%; p=0.05). Mothers of BBBAs were more likely to be unbooked (58.4% v. 10.7%; p<0.001). Cases had a higher prevalence of early sepsis (22.9% v. 3.6%; p=0.03) and birth asphyxia (14.5% v. 0.8%; p<0.001) than controls. Overall, more deaths occurred in the very-low-birthweight (VLBW) (24% v. 10%; p=0.06) and low-birthweight (LBW) (7.46% v. 0%; p=0.02) BBBAs compared with controls.
CONCLUSION: We demonstrated higher mortality in the immediate postnatal period and in the VLBW and LBW categories compared with hospital-delivered neonates. Mothers who delivered out of hospital were more likely to be multiparous and unbooked and to have unknown HIV, syphilis and rhesus results. Neonatal resuscitation, transport and immediate care on arrival at the hospital should be prioritised in the management of BBBAs.
Millennium Development Goal (MDG) 4 aims to reduce the under-5 mortality rate by two-thirds between 1990 and 2015.[1] South Africa is one of 15 countries failing to achieve the targeted reduction.[2] Neonatal mortality accounts for 40% of deaths in children <5 years old.[3] Half of these newborn deaths occur during the first 24 hours after birth and 75% during the first week, with preterm birth, severe infections and asphyxia being the main causes.[4] Improving neonatal mortality, with a particular emphasis on early neonatal deaths, therefore provides an opportunity to impact on the elusive MDG 4.
Babies born before arrival (BBBAs) constitute a high-risk newborn population. The literature demonstrates that BBBAs have increased perinatal mortality and morbidity, a longer duration of hospital stay, and, on average, lower birth weight and gestational age compared with hospital-born neonates.[5-15] The majority of these studies, however, were conducted in First-World settings,[5-11] with a paucity of evidence from the developing-world context[13,15-16] Furthermore, prior to a 2011 study,[6] the most recent literature dates back over a decade.[7,13] Consequently, there is a considerable gap in our local understanding of this high-risk neonatal group, particularly with advances in neonatal and maternal care and within a changed political healthcare environment in South Africa.
A 1984 prospective study examined BBBAs at New Somerset Hospital in Cape Town, South Africa.[15] Newborns delivered en route to hospital had more major complications and a higher perinatal mortality rate than hospital-born infants. In a First-World context, BBBAs have been shown to have a higher mortality and an increased likelihood of intensive care unit (ICU) admission.[5,8,14] The exception was a UK-based study by Bhoopalam and Watkinson,[11] who reported that immaturity and low birth weight rather than being born before arrival were linked to higher perinatal mortality.[14]
Data from developing countries have mainly looked at being born before arrival as a risk factor for mortality, with little description of the maternal and neonatal characteristics defining this group. Locally, Ballot et al.[17] reported that birth before arrival was a major determinant of survival among very-low-birth-weight (VLBW) neonates (odds ratio (OR) 0.23; 95% confidence interval (CI) 0.08 -0.69). Earlier studies conducted in Zimbabwe[10] and Bangkok[7] also showed an increased neonatal mortality among BBBAs.
The literature surrounding BBBAs seems to conclude that this is a high-risk group. However, there is a need for more recent evidence from the developing-world context. Recognising neonates at increased risk of morbidity and mortality is of particular importance in this setting, where resources are scarce and access to tertiary specialised neonatal services is limited.
Our aim was to assess whether BBBAs presenting to Charlotte Maxeke Johannesburg Academic Hospital (CMJAH), South Africa, have increased morbidity and mortality compared with inborn babies. Furthermore, we wished to analyse the maternal and clinical characteristics of BBBAs to identify potentially correctable factors responsible for poor clinical outcomes.
Methods
Study population
This was a matched, case-controlled, retrospective record review. The study population were newborns presenting to the neonatal unit at CMJAH between 1 January 2011 and 31 January 2013. CMJAH is a tertiary care institution, providing secondary and tertiary services and functioning as a referral centre for surrounding clinics and hospitals.
The definition of BBBA used in this study was any baby delivered outside the hospital or clinic setting; this encompasses a broad array of locations, including those born in the ambulance en route to hospital, at home or on the roadside. All newborns weighing >500 g and born before arrival at CMJAH were identified as cases. BBBAs first taken to a midwife obstetric unit (MOU) or surrounding hospital and referred to CMJAH were also included as cases.
Controls were the next consecutive inborn neonate matched 1:1 for birth-weight category and gender. Birth-weight categories used were: (i) extremely low birth weight (ELBW), 500 - 999 g; (ii) VLBW, 1 000 - 1 499 g; (iii) low birth weight (LBW), 1 500 - 2 499 g; (iv) normal birth weight, 2 500 -3 999 g; and (v) large birth weight, >4 000 g. Babies delivered in the hospital emergency room and maternity admission ward were considered as inborn and not BBBAs. Babies delivered in healthcare facilities outside CMJAH, including surrounding MOUs and hospitals, were not eligible to be selected as controls. Stillborn babies and those who died before arrival at hospital were not included in the study.
Data collection
The admission records of the transitional nursery attached to the labour ward were reviewed to identify the BBBAs presenting to CMJAH during the study years. This transitional unit (TU) is the area where initial resuscitation, stabilisation and observation of babies are provided to allow appropriate triage for ongoing care. BBBAs brought to CMJAH are assessed in the TU, so babies who died there, and healthy babies who were discharged to their mothers, were included in the study. Once BBBAs were identified, consecutive inborn controls were matched for birth-weight category and gender.
Information on immediate outcomes (discharged, died or admitted), antenatal booking status, birth weight, gestational age, gender, mode of delivery, time spent in the TU, parity and gravidity was extracted from the admission records. Booking status was defined as either booked or unbooked as documented in the admission registry. 'Booking status' refers to attendance at an antenatal clinic, and a mother was considered 'booked' if she had attended any antenatal care. Furthermore, birth weights were plotted on Fenton growth charts and neonates were classified as appropriate for gestational age (AGA), small for gestational age (SGA) or large for gestational age (LGA).
Data on admitted babies were extracted from the existing CMJAH neonatal database. This database, which is part of a continuing clinical audit, is collected from clinician-completed hospital records and entered into a Microsoft Access (2003) database. Additional information on admitted neonates was therefore available. Maternal information obtained from the database included maternal age, rhesus result, syphilis screening and treatment, and HIV status and prophylaxis. Neonatal variables collected included overall outcome (death or discharge), multiple pregnancy, duration of hospital stay, ICU admission, neonatal jaundice requiring phototherapy, presence of anaemia, presence or suspicion of necrotising enterocolitis (NEC), presence of patent ductus arteriosus, intraventricular haemorrhage (IVH), birth asphyxia, and primary respiratory diagnosis. As BBBAs have no documented Apgar scores and often lack arterial blood gas measurements within the first hour, the diagnosis of birth asphyxia was as assessed by the attending physician. Sepsis was considered only to be culture-proven sepsis and not suspected or clinical sepsis. All blood cultures were reviewed from National Health Laboratory Service records and classified as early sepsis (positive blood culture within 72 hours after birth) and late sepsis (positive blood culture >72 hours after birth). Cause of death was taken from the database or death certificate and classified according to the Perinatal Problem Identification Programme classification,[18] a national tool used for perinatal mortality audit. Records were verified using admission books for the neonatal wards, and outcomes were reviewed using the hospital Medicom system. In the case of admitted neonates who did not appear on the database, hospital records were obtained from the medical records department of CMJAH and the relevant details were extracted. Unknown data were classified accordingly and included in the statistical analysis.
Statistical analysis
Statistical analysis was done using SAS version 9.3. Univariate statistical analysis was performed to ascertain baseline characteristics of cases and controls. Categorical variables were described using frequencies and percentages, and continuous variables as means and standard deviations (SDs). Bivariate analysis was conducted using chi-square tests of homogeneity in order to assess whether there was a statistically significant difference in frequency between cases and controls. Two-sample t-tests were used to compare differences in means across cases and controls for normally distributed continuous variables. Further stratified analysis was done to compare outcomes across birthweight category. A p-value ≤0.05 was considered to be significant.
Ethics
Study approval was obtained from the Committee for Research on Human Subjects, University ofthe Witwatersrand, Johannesburg.
Results
A total of 178 cases and 178 controls were analysed in the final dataset. BBBAs accounted for 3% of all infants assessed in the TU and 1.8% of all deliveries captured at CMJAH. There were 77 (43.3%) male and 101 (56.7%) female cases and controls in the final dataset; 26 (14.6%) were ELBW, 50 (28.1%) VLBW, 67 (37.6%) LBW, 29 (19.3%) normal and 6 (3.4%) large birth-weight pairs. The mean birthweight (±SD) of cases was 1 819 (±844) g and that of controls, 1 865 (±888) g. The mean gestational age was 32.1 (±4.8) weeks for cases and 32.5 (±4.7) weeks for controls. There was no statistical difference for any of these parameters, confirming that the cases and controls were matched.
Differences between cases and controls are depicted in Table 1. A total of 253 neonates were admitted to the neonatal unit at CMJAH, 131 cases and 122 controls. Immediate outcome in the TU differed significantly between cases and controls, 7.9% of BBBAs v. 3.9% of controls dying in the TU (p=0.05). There was a trend towards an overall increased mortality in cases v. controls (22.5% v. 15.7%, respectively). However, this difference was not statistically significant (p=0.11).
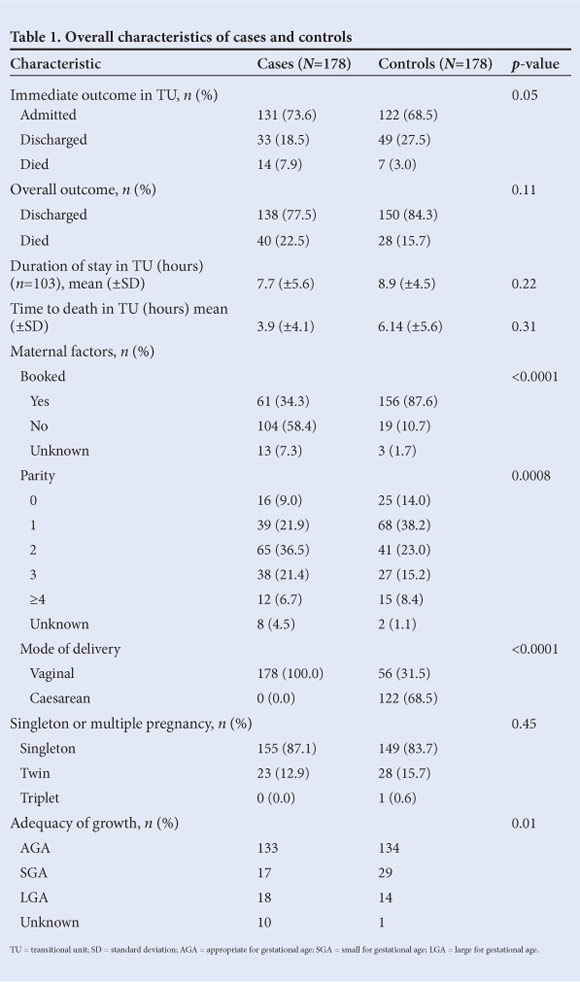
Transitional unit
The duration of stay in the TU for newborns who were discharged or died there (n=103) was similar between cases and controls (7.7 (±5.6) hours v. 8.9 (±4.5) hours; p=0.22). Cases died earlier than controls (3.9 (±4.1) hours v. 6.1 (±5.6) hours), but this was not statistically significant (p=0.31). Maternal factors that differed significantly between cases and controls included parity, booking status and mode of delivery. Controls had significantly lower parity than BBBAs. The majority (58.4%) of cases compared with 10.7% of controls were unbooked (p<0.001). All BBBAs were (understandably) born vaginally; 68.5% of controls were delivered via caesarean section. The adequacy of growth differed significantly between cases and controls; small for gestational age was more prevalent among controls (16.3% v. 9.6%; p=0.0117).
Admitted neonates
The 253 neonates who were admitted to the neonatal unit were analysed further (Table 2). The overall outcomes of admitted babies did not differ significantly between cases and controls. A total of 26 cases (20.2%) and 21 controls (17.2%) died after admission to the neonatal unit (p=0.55). The duration of hospital stay was similar between cases and controls (17.6 (±16.4) days v. 16.3 (±16) days; p=0.53). The time to death was not significantly different for cases and controls (5.3 (±6.3) days v. 8 (±8.8) days; p=0.23).
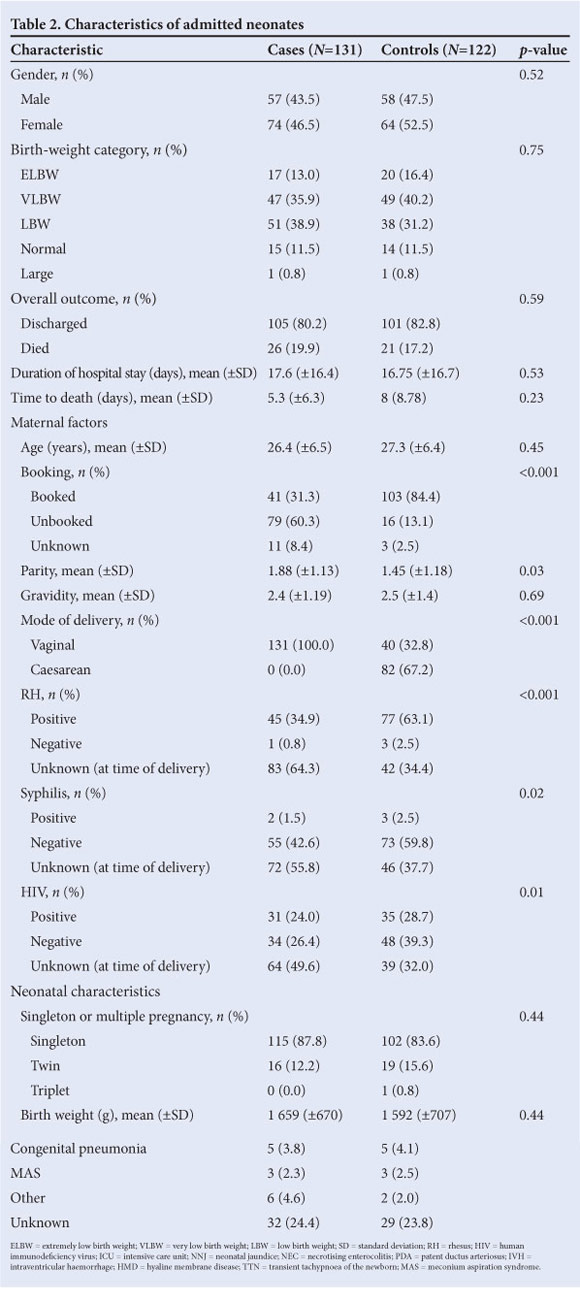
The average maternal age for cases (26.4 years) was similar to that for controls (27.3 years). Booking status differed significantly between the two groups, 60.5% of admitted cases being unbooked compared with 13.1% of controls (p<0.001). There were a large number of unknown results for HIV, syphilis and rhesus status among cases at the time of delivery.
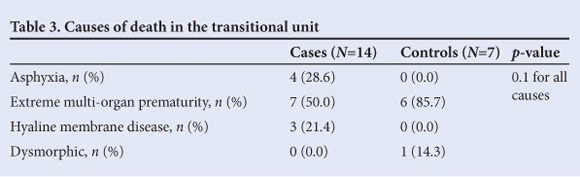
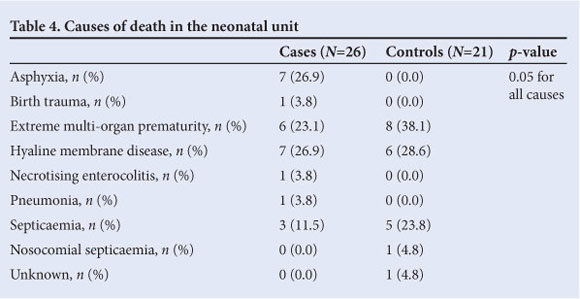
Neonatal characteristics, number of babies, ICU admission, neonatal jaundice, anaemia, NEC, IVH and respiratory diagnoses did not differ significantly between cases and controls. Although similar proportions of cases and controls had positive blood cultures (26.7% v. 23%; p=0.54), early sepsis was significantly more prevalent in BBBAs than in inborn controls (22.9% v. 3.6%; p=0.03). Birth asphyxia was more common in cases than controls (14.5% v. 0.8%; p<0.001). Tables 3 and 4 show the causes of death for babies by place of death (TU v. neonatal unit). There was higher mortality due to birth asphyxia among BBBAs compared with controls. Hyaline membrane disease and septicaemia were more often the cause of death in admitted newborns. Causes of death by birth-weight category are set out in Table 5.
Immediate and overall outcomes by birth weight
Stratified analysis of outcomes by birth-weight category is shown in Table 6. Overall, more deaths occurred in the VLBW (24.0% v. 10.0%; p=0.06) and LBW (7.46% v. 0%; p=0.02) cases compared with their respective controls. Immediate outcomes in the TU differed significantly in the LBW category. There were no LBW control deaths in the TU, compared with 3.0% of LBW cases (p=0.01).
Discussion
Neonates born before arrival are considered to be at high risk of mortality. Many previous studies have characterised a group of BBBAs, with few offering a comparison group and most making comparisons with national averages. The current study was a matched case-control review, which showed that BBBAs have higher mortality than inborn controls within the first 24 hours of presenting to hospital (7.9% v. 3.9%, respectively; p=0.05). No previous studies of BBBAs have explored the timing of neonatal deaths, yet they have identified prevalent co-morbidities such as hypothermia[10,11,13,19] and hypogycaemia,[7,12] which could explain the poor early survival. Worldwide, half of all newborn deaths occur during these initial 24 hours,[4] so recognising birth before arrival as a potential risk factor for early mortality should lead to targeted interventions to improve initial management of these neonates.
The literature consistently demonstrates that BBBAs have worse outcomes than their inborn counterparts.[5,7-9,14,19] We found a trend towards higher overall perinatal mortality in BBBAs compared with inborn controls (22.5% v. 15.7%; p=0.1057); however, this difference was not statistically significant, possibly owing to our small sample size. In addition, most of the above studies included stillbirths, which our study did not.
We found that once admitted, there was no difference in mortality, length of stay or number of ICU admissions between cases and controls. Our results are similar to those of Smith et al. ,[20] which showed that maternal booking status should not be used as a criterion for admission to an ICU, as once admitted to the ICU there was no difference in outcomes between babies of unbooked or booked mothers. This is in contrast to previous studies which have demonstrated that BBBAs have higher ICU admission rates[9] and longer hospital stays[10,13] than hospital-born infants.
We found increased mortality in our VLBW and LBW BBBAs compared with inborn babies. Previous studies on BBBAs did not stratify mortality by birth weight, but they did find that BBBAs were generally smaller and of lower gestational age than hospitalborn neonates.'7,11,131 Matching cases to controls with regard to birth weight and gender did not allow for determination of birth weight and gestational age of BBBAs compared with hospital-delivered neonates in our study, but it did allow us to identify birth before arrival as a risk factor for mortality among different birth-weight categories. In their recent study of VLBW neonates, Ballot et al.[17] identified being born before arrival as a major determinant of survival (OR 0.23; 95% CI 0.08 - 0.69). We found no difference in mortality for ELBW neonates, possibly because the overall mortality in this group is very high.[21]
BBBAs constituted 3% of all neonates who were assessed in the transitional unit at CMJAH during 2011 and 2012. From ongoing clinical audit, the BBBA rate for CMJAH was 1.8% during the study years. Potter et al.,[15] from Cape Town, proposed that a BBBA rate higher than 1.5% suggests poor access to perinatal care and warrants further investigation. Our CMJAH figure implies a need for review of our perinatal services, although encouragingly it is much lower than the national BBBA average, which according to current District Health Information System data is slightly less than 10% across all provinces.[22] Internationally, the reported rate varies from 2.9% in Muscat, Oman,[12] to 1.8% in Washington, DC,[9] and as low as 0.4% in Birmingham, UK.[11]
Consistent with the literature, we found a high number of unbooked mothers of BBBAs with unknown age, syphilis and HIV status. We found a significant difference in parity, with mothers of inborn babies more likely to be of lower parity compared with mothers of BBBAs. The literature remains inconclusive, although suggesting that mothers of BBBAs tend to be multiparous. Spillane et al.[5] (Ireland) and Bhoopalam et al.[11] (UK) found two distinct groups of mothers of BBBAs: multiparous, booked older women, and single, unbooked primigravidas. Nationality also played an important role, as refugees or foreign nationals were more likely to deliver out of hospital.[8,14]
Previous studies have generally used ICU admission as a proxy for increased morbidity among BBBAs and did not compare prevalences of conditions between BBBAs and inborn babies. We showed higher morbidity in terms of early sepsis and birth asphyxia among cases compared with inborn babies, which was expected given the unsterile environment of a birth before arrival and the lack of skilled attendants at the birth. Consequently there were more deaths due to birth asphyxia in the BBBA group compared with hospital-born controls. Despite there being no difference in culture-proven sepsis between cases and controls, we incidentally found more deaths due to sepsis in the inborn group. This could be a topic for future research.
Limitations
The retrospective design of this study is a significant limitation, as not all records were complete. Lack of consistent case definitions and inability to verify recorded diagnoses was also a problem. Furthermore, important potential modifiable factors such as maternal education, socio-economic status, nationality, area of residence, place of delivery and access to healthcare facilities could not be evaluated owing to lack of recorded information; this was particularly challenging in the case of babies who were not admitted. There was a high number of unknown HIV and syphilis results among our dataset, as information captured at the time of delivery was not subsequently updated. Measures have been instituted to improve this in the database.
There were potential unmeasured confounders not included in our analysis. Co-morbidities such as hypothermia or hypoglycaemia were not captured, and it is therefore difficult to conclude whether birth before arrival is an independent risk factor for mortality or instead due to unmeasured confounders.
It is important to recognise that both our case and control groups were heterogeneous. Our definition of a BBBA was any baby born before arrival at hospital; this could include delivery in a pit latrine or in an ambulance, as well as abandoned babies found some time after birth. The inborn controls were from a high-risk tertiary referral centre, with many babies delivered shortly after maternal admission or to significantly ill mothers. Antenatal steroid use at CMJAH is low at 35.5% (ongoing clinical audit), largely because many mothers present in advanced labour.[23] Being hospital delivered in this environment therefore does not always confer substantial benefits. Stillbirths, babies who died en route to hospital, and well BBBAs who presented to MOUs were not considered. The current results are therefore representative of a small population of BBBAs in an urban setting who present to a high-risk tertiary referral centre, and cannot be generalised to the rest of the province or country.
Conclusion
This matched case-controlled study confirmed that BBBAs constitute a vulnerable neonatal group at risk ofincreased mortality. We demonstrated higher mortality in the immediate postnatal period and in the VLBW and LBW categories compared with hospital-delivered neonates in a tertiary centre in Johannesburg, South Africa. Mothers who delivered out of hospital were more likely to be multiparous and unbooked, and to have unknown HIV, syphilis and rhesus results. Early sepsis and birth asphyxia were more prevalent among BBBAs, and mortality associated with birth asphyxia was more prevalent. Priority should be given to the training of emergency services in neonatal resuscitation and transport, as well as to maternal education on the importance of antenatal clinic attendance and recognition of the signs of labour. Immediate care on arrival at hospital should be prioritised in the management of BBBAs, as once admitted to the unit, outcomes in the two groups were comparable. A prospective population-based study is recommended.
References
1. Lawn JE, Costello A, Mwansambo C, Osrin D. Countdown to 2015: Will the Millennium Development Goal for child survival be met? Arch Dis Child 2007;92(6):551-556. [http://dx.doi.org/10.1136/adc.2006.099291] [ Links ]
2. Chopra M, Daviaud E, Pattinson R, Fonn S, Lawn JE. Saving the lives of South Africa's mothers, babies, and children: Can the health system deliver? Lancet 2009;374(9692):835-846. [http://dx.doi.org/10.1016/S0140-6736(09)61123-5] [ Links ]
3. Black RE, Cousens S, Johnson HL, et al. Global, regional, and national causes of child mortality in 2008: A systematic analysis. Lancet 2010;375(9730):1969-1687. [http://dx.doi.org/10.1016/S0140-6736(10)60549-1] [ Links ]
4. The Partnership for Maternal, Newborn & Child Health. 2011. A Global Review of the Key Interventions Related to Reproductive, Maternal, Newborn and Child Health (RMNCH). Geneva, Switzerland: PMNCH, 2011. http://www.who.int/pmnch/topics/part_publications/essential_interventions_18_01_ 2012.pdf (accessed 25 October 2013). [ Links ]
5. Spillane H, Khalil G, Turner M. Babies born before arrival at the Coombe Women's Hospital, Dublin. Ir Med J 1996;89(2):58-59. [ Links ]
6. Unterscheider J, Ma'ayeh M, Geary MP. Born before arrival births: Impact of a changing obstetric population. J Obstet Gynaecol 2011;31(8):721-713. [http://dx.doi.org/10.3109/01443615.2011.605484] [ Links ]
7. Rodie VA, Thomson AJ, Norman JE. Accidental out-of-hospital deliveries: An obstetric and neonatal case control study. Acta Obstet Gynecol Scand 2002;81(1):50-54. [http://dx.doi.org/10.1046/j.0001-6349.2001.00420.x] [ Links ]
8. King PA, Duthie SJ, To WK, Ma HK. Born before arrival - uncovering the hazards. Aust N Z J Obstet Gynaecol 1992;32(1):6-9. [http://dx.doi.org/10.1111/j.1479-828X.1992.tb01886.x]
9. Beeram M, Solarin K, Young M, Abedin M. Morbidity and mortality of infants born before arrival at the hospital. Clini Pediatr (Phila) 1995;34(6):313-316. [http://dx.doi.org/10.1177/000992289503400604] [ Links ]
10. Di Benedetto MR, Piazze JJ, Unfer V et al. An obstetric and neonatal study on unplanned deliveries before arrival at hospital. Clin Exp Obstet Gynecol 1996;23(2):108-111. [ Links ]
11. Bhoopalam PS, Watkinson M. Babies born before arrival at hospital. Br J Obstet Gynaecol 1991;98(1):57-64. [http://dx.doi.org/10.1111/j.1471-0528.1991.tb10312.x] [ Links ]
12. Bhat B, Suri K, Gupta B. A clinico-epidemiological evaluation of infants born before arrival at hospital. Ann Saudi Med 2000;20(5-6):483-484. [ Links ]
13. Sirimai K, Titapant V, Roongphornchai S. Morbidity and mortality from birth before arrival at Siriraj Hospital. J Med Assoc Thai 2002;85(12):1258-1263. [ Links ]
14. Ramsewak S, Narayansingh G, Thomas D. Born before arrival (BBA) in Trinidad - a seven year case-control study. J Obstet Gynaecol 1997;17(3):242-244. [ Links ]
15. Potter PC, Pelteret R, Reynolds L, Motala A, Kibel MA. Born before arrival: A study at the New Somerset Hospital, Cape Town. S Afr Med J 1984;66(10):377-380. [ Links ]
16. Fajemilehin RB. Factors influencing high rate of 'born-before-arrival' babies in Nigeria - a case control study in Ogbomosho. Int J Nurs Stud 1991;28(1):13-18. [http://dx.doi.org/10.1016/0020-7489(91)90045-5]
17. Ballot DE, Chirwa TF, Cooper PA. Determinants of survival in very low birth weight neonates in a public sector hospital in Johannesburg. BMC Pediatr 2010;10:30. [http://dx.doi.org/10.1186/1471-2431-10-30] [ Links ]
18. Perinatal Problem Identification Program. http://www.ppip.co.za (accessed 22 October 2013). [ Links ]
19. Kambarami R, Chidede O. Neonatal hypothermia levels and risk factors for mortality in a tropical country. Cent Afr J Med 2003;49(9-10):103-106. [ Links ]
20. Smith R, Ballot D, Rothberg A. Maternal booking status as a criterion for admission for neonatal intensive care. S Afr Med J 1995;85(5):430-431. [ Links ]
21. Kalimba E, Ballot D. Survival of extremely low-birth-weight infants. South African Journal of Child Health 2013;7(1):13-16. [http://dx.doi.org/10.7196/SAJCH.488] [ Links ]
22. National Perinatal Morbidity and Mortality Committee. National Perinatal Mortality and Morbidity Committee (NaPeMMCo) Triennial Report (20082010). South Africa, 2011. http://www.doh.gov.za/docs/reports/2011/perireport.pdf (accessed 22 October 2012). [ Links ]
23. Ballot DE, Ballot NS, Rothberg AD. Reasons for failure to administer antenatal corticosteroids in preterm labour. S Afr Med J 1995;85(10):1005-1007. [ Links ]
 Correspondence: M KBassingthwaighte (mairi.bass@gmail.com)
Correspondence: M KBassingthwaighte (mairi.bass@gmail.com)














