Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Child Health
versión On-line ISSN 1999-7671
versión impresa ISSN 1994-3032
S. Afr. j. child health vol.7 no.3 Pretoria ene. 2013
RESEARCH
Weight status and eating habits of adolescent Nigerian urban secondary school girls
A N OnyiriukaI; D D UmoruII; A N IbeawuchiIII
IMBBS, FMCPaed Department of Child Health, University of Benin Teaching Hospital, Benin City, Nigeria
IIMBBS, FWACP Department of Paediatrics, Nyanya General Hospital, Abuja, Nigeria
IIIMBBS, MWACP Department of Child Health, University of Benin Teaching Hospital, Benin City, Nigeria
ABSTRACT
BACKGROUND: Obesity in adolescence is common, and eating habits are a key determinant. Eating habits in adolescence often differ substantially from those in any other phase of life.
OBJECTIVE: To assess the weight status and eating habits of adolescent urban secondary school girls in Benin City, Nigeria.
METHODS: In this school-based cross-sectional study, data were obtained on the subjects' eating habits via a structured anonymous self-administered questionnaire, while their weights and heights were obtained by direct measurements. The body mass index (BMI), calculated as weight/height (kg/m2), was used in assessing the weight status of the participants. The study sample was 2 097 adolescent urban public school girls, aged 12 - 19 years. Information was obtained on frequencies of skipping meals, reasons for skipping meals and food choices, as well as the socio-demographic characteristics of the participants. All the students at the two study schools were invited to participate.
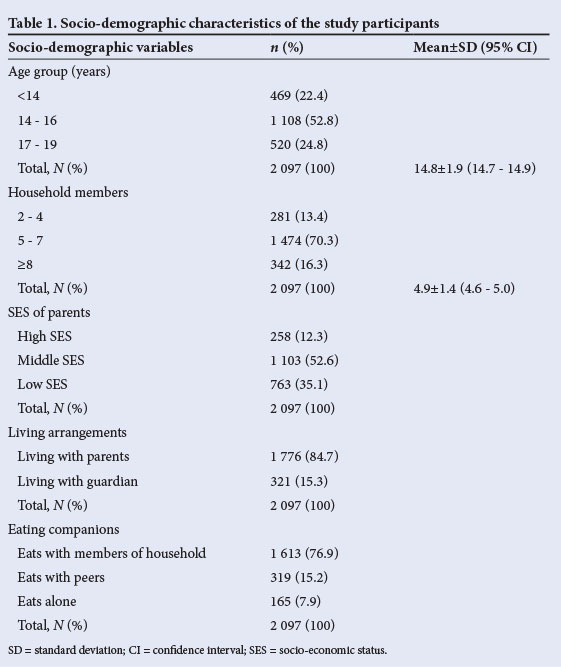
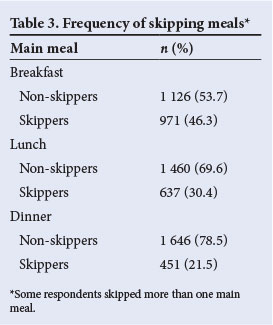
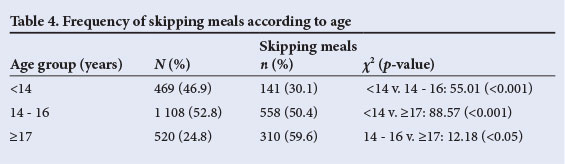
RESULTS: The mean age of the participants (± standard deviation) was 14.8±1.9 years (95% confidence interval (CI) 14.7 - 14.9). Slightly over half (52.6%) were from families of middle socio-economic status, and 84.7% of them lived with their parents. Of the 2 097 participants, 1 009 (48.1%) admitted to skipping at least one meal a fortnight. Of the three main meals, breakfast was the most frequently skipped (46.3%) and dinner the least frequently skipped (21.5%). With regard to age, the frequency of skipping meals was 30.1%, 50.4% and 58.5% among participants aged <14 years, 14 - 16 years and ≥17 years, respectively (p<0.001). The two leading reasons cited by participants for skipping breakfast were lack of appetite and time. Only 15.2% of the participants reported daily consumption of fruits and vegetables. Over half of the participants (60.2%) ate fast food at least once a week, with more than three-quarters of them (76.4%) consuming fast food along with soft drinks. The prevalences of both overweight (24.5% v. 13.2%) and obesity (2.5% v. 1.1%) were higher among girls who skipped meals compared with their peers who did not skip meals (odds ratio 0.4, 95% CI 0.32 - 0.50).
CONCLUSION: Meal skipping was associated with an increased prevalence of overweight and obesity among adolescent schoolgirls.
Obesity in childhood and adolescence is emerging as a major public health problem of our time and is known to be associated with substantial loss of quality of life and social stigmatisation that may trigger or exacerbate depression, anxiety, low self-esteem and feelings of guilt.[1-3] Studies have shown that the economic costs of obesity are substantial.[4,5] Although the prevalence of obesity is increasing worldwide, the increase has been faster in developing countries because of declining levels of physical activity as well as nutrition transition characterised by a trend towards consumption of a diet high in fat, sugar and refined foods and low in fibre.[6,7] Dietary habits are one of the modifiable risk factors for obesity in childhood and adolescence.
The developmental transition (physical, psychological and social) during adolescence provides a context for development and perpetuation of eating behaviours that are substantially different from those in other phases of life.[8] After the age of 12 years, adolescent girls seldom conform to a regular pattern of three meals a day, with over 50% of them admitting that they eat at least five times a day.[9] Healthy eating behaviour during adolescence is a fundamental prerequisite for physical growth, psychosocial development and cognitive performance, as well as for the prevention of diet-related chronic diseases in adulthood.[10] In this context, unhealthy eating behaviour is therefore a serious health issue and should be addressed.
Both clinical experience and research data indicate that irregular meal patterns are associated with obesity and that overeating is linked to breakfast skipping.[11,12] Despite the availability of reports from developing countries showing the influence of eating patterns on the escalating prevalence of obesity,[13] little is known about this relationship in the Nigerian setting. Adolescent girls as a group are highly receptive to new food products and to fast foods, largely owing to peer group influence. As a consequence, their food habits tend to be dynamic and change with time. In view of the fact that the outcome of drug therapy to curb overeating and obesity in adolescent girls is generally poor, efforts to halt the escalating prevalence of obesity in this age group in developing countries must include increased attention to healthy dietary practices.[14,15] This is important because studies have shown that adolescents tend to have insufficient knowledge of healthy dietary habits.[16] Given that prevention is the only viable long-term strategy for tackling obesity, there is a need to understand eating patterns and habits among adolescent schoolgirls before instituting effective remedial measures by means of a school-based health education programme.
The purpose of the present study was to assess weight status in relation to the eating habits of adolescent urban secondary school girls in Benin City, Nigeria. Such data are essential for dietary counselling by providing a starting point of reference for dietary modification to prevent overweight and obesity.
Methods
This descriptive, cross-sectional study was conducted in two public urban secondary day schools for girls in Oredo Local Government Area (LGA), Edo State, Nigeria, randomly selected by ballot from four all-girls' schools in the LGA.[17] The survey was designed to include all the students in the two schools (schools A and B), so no sampling was performed. There was a total of 1 394 girls in school A and 772 girls in school B, giving a grand total of 2 166, which was the target study population. Permission to conduct the study was obtained from the school administrators, and the teachers sent consent forms to parents via the students asking for permission for the child to participate.
The principals of the two schools introduced the authors during morning assembly. Subsequently, we addressed the students in their classrooms on the objectives of the study and how to fill in the questionnaire accurately. We emphasised that the questionnaires were anonymous and that the students' participation was entirely voluntary.
Data were collected between October and November 2011, using a structured anonymous self-administered questionnaire. The questionnaire was tested on 30 schoolgirls of similar age and school class in another girls-only secondary school in the same LGA. It was divided into two parts. The first part sought information on socio-demographic data, including age of the participant, number of people in the household, level of education of father and mother, occupation of father and mother, religion and state of origin. The girls were categorised into high, middle and low socio-economic groups according to the socio-economic status (SES) of their parents, which was determined using the classification suggested by Ogunlesi et al.[18] The second part of the questionnaire consisted of questions relating to eating habits, including number of meals eaten per day, whether meals were skipped, which meals were skipped, and reasons for skipping meals. Meal skipping was assessed by asking the girls whether they had skipped breakfast, lunch or dinner over the past 2 weeks; those who responded with 'yes' or 'sometimes' were regarded as skippers, while those who answered 'no' were regarded as non-skippers. The number of days meals had been skipped per week was also noted. Dietary intake data were obtained on all food items and drinks consumed during the 2 days before the survey.
All the measurements of weight and height were performed by one of the investigators (ANO) with an assistant, using the standard anthropometric methods of the International Society for the Advancement of Kinanthropometry.[19] The weight of each of the participants was measured to the nearest 0.1 kg, using a well-calibrated portable bathroom scale (Hana scale, model BR-9011) with the subject wearing a light cotton school uniform. Height was measured barefoot in the Frankfort horizontal plane to the nearest 1 cm, using a stadiometer. The body mass index (BMI) was calculated as weight/height (kg/m2), and the subjects were categorised into underweight (BMI for age <5th percentile), normal weight (BMI for age between 5th and 85th percentile), overweight (BMI for age ≥85th but <95th percentile), and obese (BMI for age ≥95th percentile), using World Health Organization criteria.[20] A snack was defined as a light meal and/or a drink consumed outside the main meals of breakfast, lunch and dinner, fast foods as quick, easily accessible and cheap alternatives to home-cooked meals, and soft drinks as non-alcoholic carbonated drinks sweetened with sugar.
The data were entered onto an Excel spreadsheet directly from the pre-coded questionnaire. Computer printouts of the data were reviewed for any information that was out of range. Statistical analysis was performed using SPSS software package version 15.0 (SPSS Inc., Chicago, IL, USA). Descriptive statistics such as frequencies, means, odds ratios (ORs), standard deviations (SDs), confidence intervals (CIs) and percentages were used to describe all the variables.
Results
At the time of the survey, a total of 2 166 girls (1 394 in school A and 772 in school B) were attending the two study schools. Seven students (5 from school A and 2 from school B) declined to participate, giving response rates of 99.6% for school A and 99.7% for school B. The overall response rate was 99.7%. The questionnaires for 62 students were excluded from the final analysis because they were incompletely filled out, leaving a total of 2 097 questionnaires (respondents) for data analysis. Students in the two schools had similar socio-demographic characteristics, so further analysis of data was done on the combined group of students. Of the 2 097 participants, 82.6%, 14.8% and 2.6% were from Christian, Muslim and traditional religion families, respectively. Eating patterns did not differ with regard to state of origin or religion. The socio-demographic characteristics of the participants are set out in Table 1. Over half of the girls (52.8%) were aged 14 - 16 years, the majority (84.7%) lived with family members, and over two-thirds (70.3%) lived in households with five to seven members. More than half (52.6%) of the participants came from families of middle SES.
The dietary practices of the participants are set out in Table 2. Starchy food and milk/dairy products were the most and the least frequently consumed food items, respectively. Of the 2 097 participants, 829 (39.5%) were not choosy with regard to types of food, reporting that they ate any available food. A little more than one-quarter (28.7%) admitted that they were trying to eat less to lose weight, although they did not follow any specific diet. More than half of the participants reported consuming soft drinks daily (Table 2); of these, 46.5% preferred small-size soft drinks (350 ml) and the rest (53.5%) large-size drinks (500 ml). Only 87 (4.1%) of the 2 097 participants took dietary supplements (mainly multivitamins and ferrous sulphate), those who used supplements doing so on their parents' advice. The family gathered together for meals in 33.9% of cases, with the father being the most frequently missing member.
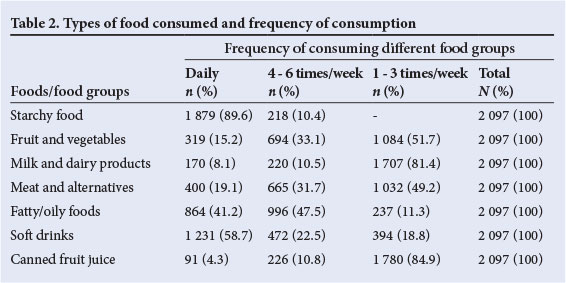
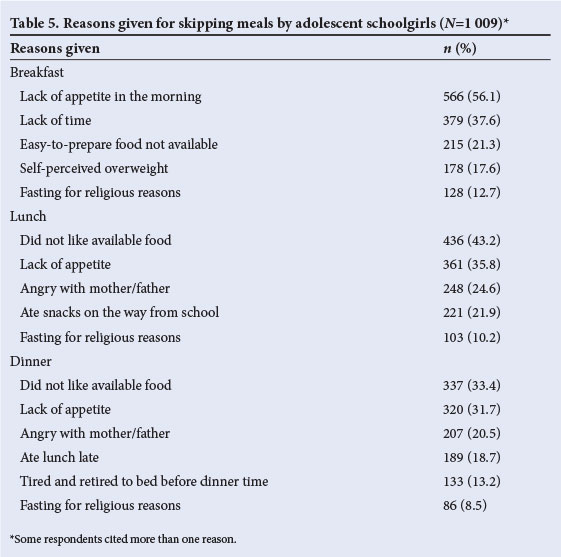
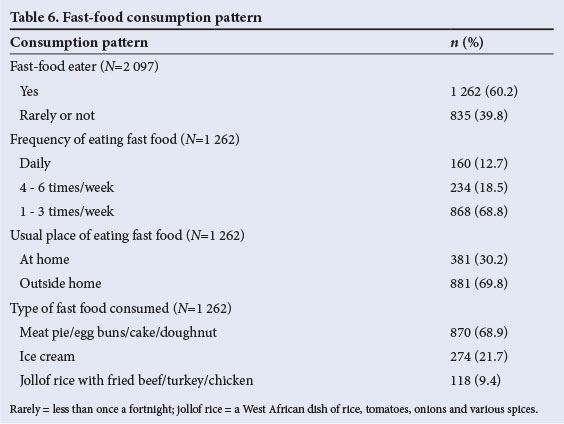
Of the 2 097 girls, 1 009 (48.1%) reported skipping at least one meal (skippers), while 1 088 (51.9%) were non-skippers. Table 3 shows that breakfast was the most frequently skipped meal, followed by lunch and then dinner. In comparison with dinner, breakfast was skipped 2.2 times more often and lunch 1.4 times more often. Among the 1 009 participants who admitted to skipping at least one meal a day, slightly over half (51.0%) ate alone, 33.8% ate with family members and 15.2% ate with peers. The frequency of skipping meals is related to age in Table 4, which shows that there was a significant increase in frequency of skipping meals with increasing age. The two main reasons for skipping breakfast were lack of appetite in the morning and lack of time (Table 5). As shown in Table 6, consumption of energy-dense fast-food items outside the home is common among adolescent schoolgirls. Over three-quarters (76.0%) of the respondents usually consumed fast foods along with soft drinks. The frequency of consumption of the various items in all the food groups did not influence the subjects' weight status.
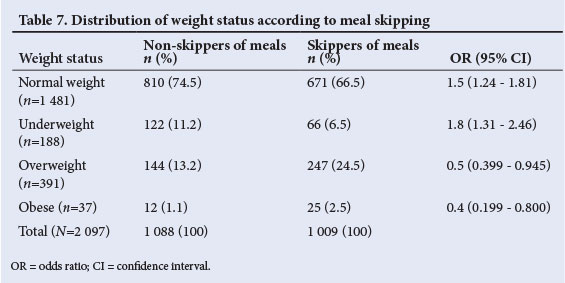
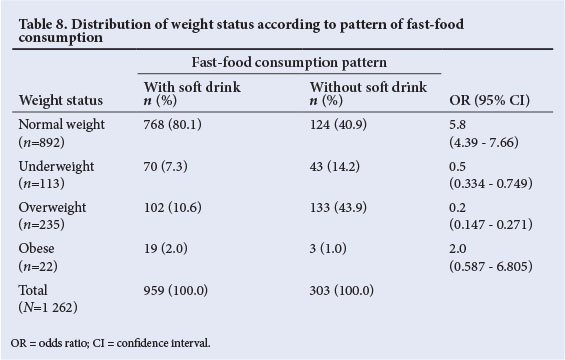
The prevalences of both overweight (24.5% v. 13.2%) and obesity (2.5% v. 1.1%) were higher in girls who skipped meals compared with their peers who did not (OR 0.4; 95% CI 0.32 - 0.50) (Table 7). With regard to consumption of fast food along with soft drinks, the prevalences of both underweight and overweight were higher among girls who did not consume fast food along with soft drinks (Table 8). Of the participants who reported consuming snacks regularly, over half also admitted to skipping meals.
Discussion
The study showed that skipping of meals was a common eating habit among adolescent Nigerian urban schoolgirls. This is not surprising, as studies from several other developing countries have reported similar findings.[21-24] Consistent with reports of others,[21,22,25] our data indicate that breakfast was the most frequently skipped of the three main meals. Older girls tended to skip breakfast more often than younger girls, suggesting that the prevalence of breakfast skipping increases with the transition from adolescence to adulthood. This is also not surprising, as two studies have reported a similar finding.[12,23] These studies demonstrated that breakfast skipping was linked to weight gain, ultimately resulting in overweight. The unhealthy habit of skipping meals that we detected among our adolescent schoolgirls may be of concern - results from a 2007 study suggested that skipping breakfast significantly decreased daily energy and nutrient intake,[26] some studies have linked skipping of meals with overweight as well as obesity,[12,23,27,28] and other studies have linked meal skipping by adolescents, particularly not eating breakfast, to adverse nutritional status, impaired cognitive performance and reduced quality of life.[29] Dinner was the least commonly skipped meal in the present study, as has been found by others.[30] Consistent with the results of a study in Turkey,[29] the main reasons cited by the participants for skipping breakfast were lack of appetite and lack of time. This finding is worrying, because breakfast is considered the most important of all the three main meals. SES of the participants' families did not appear to influence the prevalence of meal skipping in our study, suggesting that the effects of socio-economic differences are less pronounced during adolescence than during other phases of life. The apparent lack of influence of SES on meal skipping among adolescent schoolgirls is consistent with the results of the study by Soyer et al.,[29] and may be explained by the homogenising effects of school experiences as well as youth culture. Our data indicate that schoolgirls who were 17 or older were more likely to skip meals than their schoolmates who were less than 14 years old. A similar observation has been reported in an earlier study.[22] One possible explanation may be that older schoolgirls are more concerned with body image than their younger counterparts. This view is reinforced by the observation in the present study, as well as in previous ones, that concern about body image is linked to the practice of skipping meals among adolescent schoolgirls.[22,31,32]
Consistent with previous studies,[24,26,32] assessment of weight status revealed that the prevalences of both overweight and obesity were higher among participants who skipped meals compared with their peers who did not. A possible explanation was given by Savige et al.,[33] who observed that adolescent girls who skipped meals, particularly breakfast, were more likely to eat snacks during the day, ultimately resulting in excess daily energy consumption. Another explanation may be that not eating breakfast results in a poor quality of life, characterised by lack of energy in the morning and decreased motivation to participate in physical activity.[34] The combination of excess energy intake with reduced physical activity is well known to be a key determinant of overweight and obesity in adolescence.[16] The practice of skipping meals may be related to body image concerns, and a weight-loss strategy for adolescent girls. This view is supported by the report of Boutelle et al.,[35] as well as our finding that 17.6% of girls who skipped breakfast cited self-perceived overweight as the reason.
Our study revealed a relatively high rate of consumption of fast food by adolescent urban Nigerian schoolgirls. A similar finding was reported in a study of adolescent schoolgirls in Iran.[28] One feature of fast-food consumption in the present study that needs to be highlighted is that over three-quarters (76.0%) of the girls consumed fast food along with soft drinks. This is also not surprising, as it is consistent with studies of adolescents in Saudi Arabia and Iran,[12,28] and it is a worrying finding because two-thirds (68.9%) of the fast food consumed by the girls in the present study was energy-dense food such as meat pies, egg buns, cake and doughnuts; the combination of such food with soft drinks, which have a high glycaemic index and are also energy dense, is a very unhealthy eating habit. Regular consumption of fast food along with soft drinks has the potential to alter the balance between energy intake and expenditure in favour of the former, predisposing the adolescent to overweight and/or obesity. Data from the present study, however, revealed a higher prevalence of overweight in adolescents who did not consume fast food along with soft drinks. This finding is surprising because excessive soft-drink consumption in itself is known to promote overweight and obesity.[36] The reason for the difference between the finding in the present study and that of Shannon et al.[36] is not clear.
Some limitations of our study need to be considered. Firstly, it included only adolescent girls, so the results cannot be generalised to include both genders. Secondly, the findings are limited by the sampling location, since the participants were derived from schoolgirls in only one LGA. Despite these limitations, it gives insight into the weight status and eating behaviours of adolescent schoolgirls in this area. The strength of the study lies in the large study population, which allows meaningful conclusions. It is therefore suggested that the scope of future studies on the subject should be broadened to include male adolescents, secondary schools in other LGAs of the state, and adolescents in the rural areas.
In conclusion, the study revealed that adolescent schoolgirls who skip meals have a higher prevalence of both overweight and obesity.
References
1. Visscher TL, Seidell JC. The public health impact of obesity. Annu Rev Public Health 2001;22(1):355-375. [http://dx.doi.org/10.1146/annurevpublhealth.22.1.355] [ Links ]
2. Puhl R, Brownell KD. Bias, discrimination and obesity. Obes Res 2001;9(12):788-805. [http://dx.doi.org/10.1038/oby.2001.108] [ Links ]
3. Han TS, Tijhuis MA, Lean ME, Seidell JC. Quality of life in relation to overweight and body fat distribution. Am J Public Health 1998;88(12):1814-1820. [http://dx.doi.org/10.2105/AJPH.88.12.1814] [ Links ]
4. Cawley J, Mayerhoefer C. The medical care costs of obesity: An instrumental variable approach. J Health Economics 2012;31(1):219-230. [http://dx.doi.org/10.1016/j.jhealeco.2011.10.003] [ Links ]
5. Jurgen J, Wenig CM, Wolfenstetter SB. Recent economic findings on childhood obesity: Cost-of-illness and cost-effectiveness of interventions. Curr Opin Clin Nutr Metab Care 2010;13(3):305-313. [http://dx.doi.org/10.1097/mco.ob 013e328337fe18] [ Links ]
6. Monteiro CA, Benicio MHDA, Conde WL, Popkin BM. Shifting obesity trends in Brazil. Eur J Clin Nutr 2000;54(4):342-346. [http://dx.doi.org/10.1038/sj.ejcn.1600960] [ Links ]
7. Popkin BM. Understanding the nutrition transition: Measuring rapid dietary changes in transitional countries. Public Health Nutr 2002;5(6a):947-952. [http:dx.doi.org/10.1079/PHN2002370] [ Links ]
8. Quatromoni PA, Copenhafer DL, D'Agostino RB, Millen BE. Dietary patterns predict the development of overweight in women: The Framingham Nutrition Studies. J Am Diet Assoc 2002;102(2):203-211. [http://dx.doi.org/10.1016/S0002-8223(02)90049-0] [ Links ]
9. Swinburn B, Egger G. The runaway weight gain train: Too many accelerators, not enough brakes. BMJ 2004;329:736-739. [http://dx.doi.org/10.113/bmj.329.7468.736] [ Links ]
10. French SA, Lin BH, Guthrie JF. National trends in soft drink consumption among children and adolescents aged 6 to 17 years: Prevalence, amount, and sources, 1977/1978 to 1994/1998. J Am Diet Assoc 2003;103(10):1326-1331 [http://dx.doi.org/10.1016/S0002-8223(03)01076-9] [ Links ]
11. Keski-Rahkonen A, Kaprio J, Rissanen A, Virkkunen M, Rose RJ. Breakfast skipping and health-compromising behaviours in adolescents and adults. Eur J Clin Nutr 2003;57(7):842-853. [http://dx.doi.org/10.108/sj.ejcn.1601618] [ Links ]
12. Neimeier H, Raynor H, Lloyd-Richardson E, Rogers M, Wing R. Fast food consumption and breakfast skipping: Predictors of weight gain from adolescence to adulthood in a nationally representative sample. J Adolesc Health 2006;39(6):842-849. [http://dx.doi.org/10.1016/j.jadohealth.2006.07.001] [ Links ]
13. Prentice AM. The emerging epidemic of obesity in developing countries. Int J Epidemiol 2006;35(1):93-99. [http://dx.doi.org/10.1093/ije/dyi272] [ Links ]
14. Matthews VL, Wien M, Sabate J. The risk of child and adolescent overweight is related to types of food consumed. Nutr J 2011;10(1):71-74. [http://dx.doi.org/10.1186/1475-2891-10-71] [ Links ]
15. Pinhas-Hamiel O, Sabin M. Obesity in developing countries. In: Zacharin M, ed. Practical Paediatric Endocrinology in a Limited Resource Setting. Melbourne: Merck Sereno, 2011:109-129. [http://dx.doi.org/10.1016/B978-0-12-407822-2-00006-2] [ Links ]
16. Hassapiduo M, Fotiaduo E, Maglara E, Papadopoulou SK. Energy intake, diet consumption, energy expenditure and body fatness of adolescents in Northern Greece. Obesity (Silver Spring) 2006;14(5):855-862. [http://dx.doi.org/10.1038/oby.2006.99] [ Links ]
17. Ministry of Education, Benin City. Department of Planning, Research and Statistics. Directory of Pre-primary, Primary, Junior and Senior Secondary Institutions in Edo State, 2006. www.edostate.gov.ng/ministries/education (accessed 5 August 2013). [ Links ]
18. Ogunlesi TA, Dedeke IOF, Kuponiyi OT. Socioeconomic classification of children attending specialist paediatric centres in Ogun State, Nigeria. Nig Med Pract 2008;54(1):21-25. [http://-dx.doi.org/10.4314/nmp.v54i1.28943] [ Links ]
19. Marfell-Jones M, Olds T, Stew A, Carter L. International Standards for Anthropometric Assessment. Underdale, Australia: International Society for the Advancement of Kinanthropometry, 2006. [ Links ]
20. World Health Organization. Physical Status: The Use and Interpretation of Anthropometry. Report of a WHO Expert Committee. Geneva: World Health Organization, 1995 (WHO Technical Series, No. 854). [ Links ]
21. Gross SM, Bronner Y, Welch C, Dewberry-Moore N, Paige DM. Breakfast and lunch meal skipping patterns among fourth-grade children from selected public schools in urban, suburban, and rural Maryland. J Am Diet Assoc 2004;104(3):420-423. [http://dx.doi.org/10.1016/juda200312.014] [ Links ]
22. Chin YS, Mohd Nasir MT. Eating behaviors among female adolescents in Kuantan district, Pahang, Malaysia. Pakistan Journal of Nutrition 2009;8(4):425-432. [http://dx.doi.org/10.3923/pjn.2009.425.432] [ Links ]
23. Thompson-McCormick JJ, Thomas JJ, Bainivnualiku A, Khan AN, Becker AE. Breakfast skipping as a risk correlate of overweight and obesity in school-going ethnic Fijian adolescent girls. Asia Pac J Clin Nutr 2010;19(3):372-382. [ Links ]
24. Moy FM, Gan CY, ZalehaSiti MK. Eating patterns of school children and adolescents in Kuala Lumpur. Malaysian Journal of Nutrition 2006;12:1-10. [ Links ]
25. Shaw ME. Adolescent breakfast skipping: An Australian study. Adolescence 1998;33(132):851-861. [ Links ]
26. Chitra U, Reddy CR. The role of breakfast in nutrient intake of urban school children. Public Health Nutr 2007;10(1):55-58. [http://dx.doi. org/101017/S1368980007219640] [ Links ]
27. Neumark-Sztainer D, Wall M, Haines J, Story M, Eisenberg ME. Why does dieting predict weight gain in adolescence? Findings from Project EAT-II: A 5-year longitudinal study. J Am Diet Assoc 2007;107(3):448-455. [http://dx.doi.org/10.1016/j.jada2006.12.013] [ Links ]
28. Montazerfar F, Karajibani M, Dashipour AR. Evaluation of dietary intake and food patterns of adolescent girls in Sistan and Baluchistan Province, Iran. Functional Foods in Health and Disease 2012;2(3):62-71. [ Links ]
29. Soyer MT, Ergin I, Gursoy ST. Effects of social determinants on food choice and skipping meals among Turkish adolescents. Asian Pac J Clin Nutr 2008;17:208-213. [ Links ]
30. Samuelson G. Dietary habits and nutritional status in adolescents over Europe: An overview of current studies in the Nordic countries. Eur J Clin Nutr 2000;54:S21-S28. [http://dx.doi.org/10.1038/sj.ejcn.1600980] [ Links ]
31. Calderon LL, Yu CK, Jambazian P. Dieting practices in high school students. J Am Diet Assoc 2004;104(9):1369-1374. [http://dx.doi.org/10.16/j.jada.2004.06.017] [ Links ]
32. Sjoberg A, Hallberg L, Hoglund D, Hulthen L. Meal pattern, food choice, nutrient intake and life style factors in the Goteborg Adolescence Study. Eur J Clin Nutr 2003;57(12):1569-1578. [http://dx.doi.org/10.1038/sj.ejcn.1601726] [ Links ]
33. Savige G, MacFarlane A, Ball K, Worsley A, Crawford D. Snacking behaviours of adolescents and their association with skipping meals. Int J Behav Nutr Phys Act 2007;4(1):36-44. [http://dx.doi.org/10.1186/1479-5868-4-36] [ Links ]
34. Godin G, Anderson D, Lambert LD, Desharnais R. Identifying factors associated with regular physical activity in leisure time among Canadian adolescents. Am J Health Promot 2005;20(1):20-27. [http://dx.doi.org/10.4278/0890-1171-20.1.20] [ Links ]
35. Boutelle K, Neumark-Sztainer D, Story M, Resnick M. Weight control behaviors among obese, overweight and non-overweight adolescents. J Pediatr Psychol 2002;27(6):531-540. [http://dx.doi.org/10.1093/jpepsy/27.6.531] [ Links ]
36. Shannon C, Story M, Fulkerson JA, French SA. Factors in the school cafeteria influencing food choices by high school students. J Sch Health 2002;72(6):229-234. [http://dx.doi.org/10.1111/j.1746-1561.2002.tb.07335.x] [ Links ]
 Correspondence: A N Onyiriuka (alpndiony@yahoo.com; didiruka@gmail.com)
Correspondence: A N Onyiriuka (alpndiony@yahoo.com; didiruka@gmail.com)














