Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Child Health
On-line version ISSN 1999-7671
Print version ISSN 1994-3032
S. Afr. j. child health vol.7 n.1 Pretoria Jan. 2013
RESEARCH
Survival of extremely low-birth-weight infants
E M KalimbaI; D E BallotII
IMB BCh; Department of Paediatrics and Child Health, University of the Witwatersrand and Charlotte Maxeke Johannesburg Academic Hospital, Johannesburg
IIMB BCh, FCPaed (SA), PhD; Department of Paediatrics and Child Health, University of the Witwatersrand and Charlotte Maxeke Johannesburg Academic Hospital, Johannesburg
ABSTRACT
OBJECTIVES: Survival of extremely low-birth-weight (ELBW) infants in a resource-limited public hospital setting is still low in South Africa. This study aimed to establish the determinants of survival in this weight category of neonates, who, owing to limited intensive care facilities, were not mechanically ventilated.
DESIGN: A retrospective study in which patient data were retrieved from the departmental computer database.
SETTING: The neonatal unit at Charlotte Maxeke Johannesburg Academic Hospital, Johannesburg, South Africa.
SUBJECTS: Neonates admitted at birth between January 2006 and December 2010 with birth weights of ≤ 900 g.
OUTCOME MEASURES: Survival at discharge was the major outcome. Maternal variables were age, parity, gravidity, antenatal care, antenatal steroids, place and mode of delivery and HIV status. Neonatal variables were gestational age (GA), birth weight (BW), gender, place of birth, hypothermia, resuscitation at birth, sepsis, necrotising enterocolitis, intraventricular haemorrhage, jaundice, nasal continuous positive airway pressure (NCPAP) with or without surfactant, and Apgar scores.
RESULTS: A total of 382 neonates were included in the study. Overall survival was 26.5%. The main causes of death, as per the Perinatal Problem Identification Programme (PPIP) classification, were extreme multi-organ immaturity and respiratory distress syndrome. The main determinants of survival were BW (odds ratio (OR) 0.994; 95% confidence interval (CI) 0.991 - 0.997) and GA (OR 0.827; 95% CI 0.743 - 0.919). Overall the rate of NCPAP use was 15.5%, and NCPAP was not associated with improved survival.
CONCLUSION: Survival of ELBW infants is low. BW and GA were the strongest predictors of survival. Effective steps are required to avoid extreme prematurity, encourage antenatal care, and provide antenatal steroids when preterm birth is anticipated.
United Nations Millennium Development Goal 4 is to reduce child mortality by reducing under-5 mortality by two-thirds between 1990 and 2015. More than 8 million children aged under 5 die every year, and neonatal mortality and especially very low-birth-weight (VLBW) infant mortality are among the six factors to which over 90% of these deaths are attributed.[1]
Survival of extremely low-birth-weight (ELBW) infants has improved markedly over the past decade, largely owing to improved care, availability of antenatal steroids, provision of surfactant and establishment of appropriately equipped intensive care units (ICUs) where resources permit.[2-4] Yet survival of these infants in a resource-limited setting like South African public hospitals is still low.[5]
Mortality as a result of prematurity is the major contributor to the neonatal mortality rate in both developing and developed countries.[6] According to the World Health Organization, nearly 4 million neonatal deaths occur worldwide every year, most in developing countries.[7]
In South Africa, perinatal mortality and low-birth-weight rates have in the past generally been reported only for infants weighing ≥ 1 000 g at birth, because smaller infants are often regarded as miscarriages and not recorded. However, with improving maternal and neonatal care, more infants weighing 500 - 1 000 g are expected to survive.
In a study at Chris Hani Baragwanath Academic Hospital (CHBAH), a busy public hospital in Soweto, Johannesburg, the rate of survival of ELBW infants was found to be 34%.[5] A similar study done previously at Charlotte Maxeke Johannesburg Academic Hospital (CMJAH) found the rate of survival of ELBW infants to be 34.9%.[8] More recently, a study at Tygerberg Children's Hospital in the Western Cape reported the rate of survival of ELBW infants who received surfactant and nasal continuous positive airway pressure (NCPAP) to be 62.9%.[4] The infants in this study had back-up mechanical ventilation provided for failed NCPAP.
Our study was done in the neonatal unit at CMJAH, a busy public hospital in Johannesburg. Owing to limited neonatal ICU facilities, mechanical ventilation is only provided for infants with a birth weight (BW) >900 g. ELBW infants who have no access to an ICU are therefore managed in a busy high-care ward. The aims of this study were to review the survival of these infants and to evaluate factors determining their survival.
Methods
This was a retrospective study of all neonates with a BW of ≤ 900 g admitted to the neonatal unit at CMJAH between January 2006 and December 2010. These infants were not offered mechanical ventilation, as per the unit's neonatal ICU admission criteria. Infants' records were reviewed only for the period of hospitalisation until discharge. All in-born neonates were admitted directly to a transitional nursery in the labour ward, so statistics included babies who died shortly after birth. Neonates delivered at primary-level hospitals or clinics in the close vicinity and those who were born before arrival (BBA) were also admitted to the transitional unit and are therefore part of our statistics. NCPAP was introduced into the unit in 2006. Babies with a BW ≥ 750 g were offered NCPAP with surfactant at the discretion of attending staff. There was no back-up mechanical ventilation available for these infants.
A computer database is kept for purposes of clinical audit and information for outpatient neonatal follow-up. The following relevant data were retrieved from the database: maternal data - age, parity, gravidity, antenatal care (ANC), antenatal steroids, place and mode of delivery, and HIV status; infant data - the major outcome (death or survival), gestational age (GA), BW, gender, place of birth, hypothermia, resuscitation at birth, sepsis, necrotising enterocolitis (NEC), intraventricular haemorrhage (IVH), jaundice, NCPAP with or without surfactant, and 5-minute Apgar scores. The causes of death were reviewed and classified according to the Perinatal Problem Identification Programme (PPIP) classification (http://www.ppip.co.za). The PPIP was established in South Africa in 1999 as a national tool for perinatal death audit.
Data were entered onto an MS-Excel spreadsheet and then imported to the statistical software SPSS version 19 (http://www.spss.com) for analysis. Categorical data were described using frequencies and percentages, and continuous data as means and standard deviations (SDs). A univariate statistical analysis was done on maternal and neonatal variables considering survival at discharge as the outcome. Categorical data were compared using chi-square analysis and continuous data using unpaired t-tests (as the distribution was normal). A p-value of 0.05 was considered to be significant. Factors with a p-value of ≤ 0.1 were included in the multiple logistic regression analysis.
Ethics
Approval of the study was granted by the Committee for Research on Human Subjects, University of the Witwatersrand, Johannesburg.
Results
There was a total of 410 babies. Data were incomplete for 29, and 3 of these had no final outcome recorded. For the 26 whose inal outcome was recorded, GA, mode of delivery, HIV status, NCPAP and surfactant were some of the factors that were not available in our records. All the 29 who were excluded had BWs >600 g. There were 8 survivors in this group (30.6%). We therefore had 382 babies with complete records included in our study. Female infants accounted for a slight majority, at 53.5% of the total. Of the female babies 30.6% survived, whereas of the males 23.7% survived (x2 4.38; p=0.357). The infants' mean GA was 26.7 weeks (SD 2.37), and mean BW was 774 g (SD 94). The mean GA of non-survivors was 26.4 weeks (SD 2.331), as opposed to 27.6 weeks (SD 2.23) for survivors (p<0.001). The mean BW of survivors was 814 g (SD 74), as opposed to 759.8 g (SD 97) for non-survivors (p<0.001). The vast majority of infants were in-born (79.3%), with the rest either referred from the surrounding clinics or BBA.
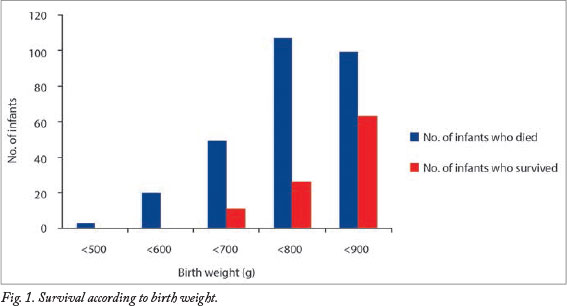
The overall survival rate was 26.5%. No neonate weighing <600 g survived (Fig. 1). The survival rate was highest for babies with the highest BWs.
The various causes of death according to the PPIP classification are shown in Table 1. The most frequent cause of death was extreme multi-organ immaturity (63.9%), followed by respiratory distress syndrome (RDS) (25.9%).

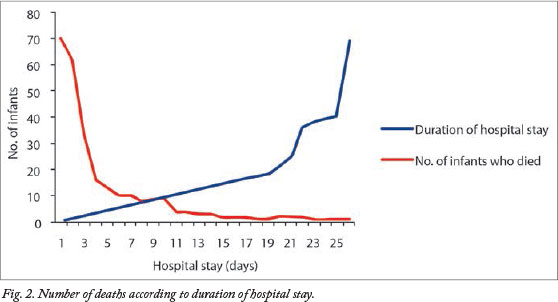
Most infants died within the irst few days of life, 60% within 72 hours and 79% by the end of the first week. The median age at death was 3 days (range 0 - 69 days) (Fig. 2).
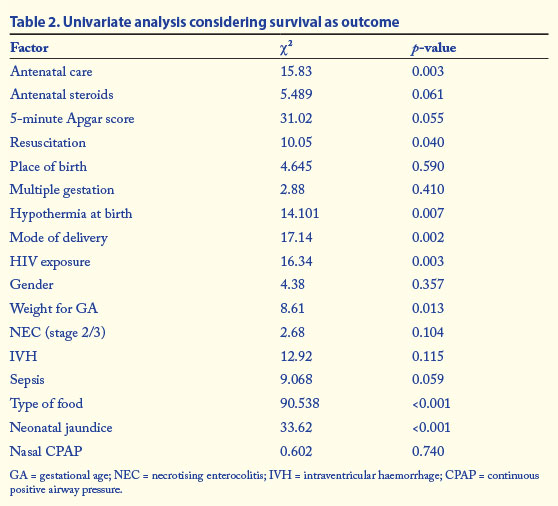
Univariate analysis was done on the various patient characteristics by comparing survivors and non-survivors using cross-tabulation with chi-square analysis. The results are shown in Table 2. The most significant predictors of survival on univariate analysis were antenatal care, HIV exposure, mode of delivery, hypothermia at birth, weight for GA, mode of feeding and the presence of neonatal jaundice. These factors together with GA and BW were considered in the binary logistic regression model with survival as the outcome. The final results of the logistic regression are shown in Table 3. BW, GA and neonatal jaundice were the most signiicant determinants of outcome.
Nasal continuous positive airway pressure
Over the 5-year study period, a total of 59 infants with BWs between 750 g and 900 g were given NCPAP. Twenty-nine of these infants were also given surfactant. The use of NCPAP in this group of patients increased signiicantly from less than 10% in 2007 to 37.5% in 2010. Of the 59 infants who received NCPAP, 16 (27.1%) survived until discharge. Overall, NCPAP had no influence on survival (x2 0.602; p=0.74). However, NCPAP was only used in the latter part of our study period and only in neonates with BWs ≥ 750 g. When only babies weighing >700 g in 2008 - 2010 are considered, babies weighing >800 g who received NCPAP were signiicantly less likely to survive (19% in the NCPAP group v. 27% in the non-NCPAP group; x2 9.247; p=0.002).
Discussion
This was the first study in our unit to look solely at ELBW infants, specifically those with BWs ≤900 g who did not receive conventional mechanical ventilation. Similar previous studies in the same unit included the VLBW category. Generally, all studies in the literature looking at ELBW babies have considered weights of 500 - 1 000 g. Our mean GA was 26.7 weeks, with 774 g the mean BW. This - mean BW was lower than that in the InSurE study at Tygerberg Children's Hospital in the Western Cape (856.2 g), as would be expected, since their weight category included 900 - 1 000 g.[4] Our overall survival rate of 26.5% is lower than the 62.9% in the InSurE study. However, our statistics included babies who died - in the labour ward shortly after birth as well as babies who were not born in our hospital, and these were both excluded in the InSurE study. The survival was also lower than the previous data from our unit, which showed survival in the ELBW category to be 34.9%, very similar to the CHBAH study indings of 34%. [5,8] However, it should be noted that our study only considered babies up to 900 g BW, excluding the 901 - 1 000 g babies included in both the above studies. This makes a significant difference, because previous data from our unit have demonstrated exponentially improved survival in babies weighing over 900 g, given also that they are allowed admission to the ICU.
In sthe current study, BW and GA were the most significant predictors of survival (p<0.001). This is well documented in the literature in studies done across both developed and developing countries[4,5,8] and was also found in both the previous study from our unit on determinants of survival in VLBW infants and the study at CHBAH.[5,8] Similar findings were reported from a large cohort study that included multiple participating academic centres in the USA.[9]
On univariate analysis, BW in relation to GA was also a signiicant determinant of survival (p=0.013). Similar findings were reported in a Norwegian study comparing survival of small for gestational age babies, deined as having a BW below the 5th percentile for postmenstrual age, with the appropriate for gestational age group and showing that the former had higher mortality and morbidity.[10]
Surprisingly, NCPAP did not seem to improve survival. Neonates weighing ≥ 750 g qualified for NCPAP according to the unit guidelines. None of the infants in our study group was given back-up ventilation in the ICU. However, owing to the limited number of NCPAP machines, the sickest babies were the ones given NCPAP, and this probably explains the increased mortality in this group.
Although antenatal steroids have been shown to improve survival, mostly by reducing the severity of RDS, our results only approached statistical significance (p=0.06). There was an association with improved outcome in the InSurE study, in which 76% of the mothers had received steroids with improved survival of babies at day 3 and day 7 of life.[4]
On univariate analysis, sepsis was paradoxically associated with an increased chance of survival. This finding contrasts with a large study carried out in India looking at survival and morbidity of ELBW infants over a 6-year period, where sepsis was a major contributor to mortality, being responsible for 41% of deaths.[11] The association between sepsis and survival could be explained by the fact that most babies in our study died within the first few days after birth. Those who survived longer had a higher chance of developing nosocomial sepsis.
There was a strong association between jaundice and survival (p<0.001). This would be explained by the fact that up to 80% of preterm babies have physiological jaundice, peaking towards the end of the irst week after birth. Since most of our babies died in the irst week after birth, the survivors were the babies who became jaundiced. There was an association between hypothermia and death (p=0.007), which has been well demonstrated previously. [12, 13]
HIV exposure in our study signiicantly increased the risk of death (p=0.003). However, it is worrying that 45.9% of the mothers did not know their HIV status.
Babies born by normal vaginal delivery had a signiicantly lower chance of survival than those born by caesarean section (CS). These indings are similar to data from a study in the USA showing that ELBW babies born by CS had a signiicantly increased chance of survival.[14] According to that study, the small babies born vaginally had more than twice the risk of developing severe intraventricular haemorrhage and having a poor short-term outcome compared with those born by CS.
After multiple logistic regression analysis, BW and GA were the most powerful predictors of survival. This is similar to findings in studies mentioned above as well as previous data from our unit.[4,5,8]
Conclusion
Our study shows that survival of ELBW infants in a resource-limited public hospital setting in South Africa is very low. BW and GA were the strongest predictors of survival. Although our results did not show NCPAP and surfactant to have a positive impact, it has been demonstrated in several studies that provision of NCPAP with surfactant to this category of infants improves outcome. Effective steps to avoid extreme prematurity and encourage ANC attendance need to be put in place. Preventing important causes of morbidity and mortality such as HIV, asphyxia and hypothermia would also improve survival.
References
1. United Nations. Reduce Child Mortality. The Millenium Development Goals Report. New York: UN, 2008. [ Links ]
2. Wilson-Costello D. Is there evidence that long-term outcomes have improved with intensive care? Semin Fetal Neonatal Med 2007;12(5):344-354. [http://dx.doi.org/10.1016/j.siny.2007.06.010] [ Links ]
3. Lorenz JM. Survival of the extremely preterm infant in North America in the 1990s. Clin Perinatol 2000;27(2):255-262. [http://dx.doi.org/10.1016/S0095-5108(05)70020-8] [ Links ]
4. Kirsten GF, Kirsten CL, Henning PA, et al. The outcome of ELBW infants treated with NCPAP and InSurE in a resource-limited institution. Pediatrics 2012;129(4):e952-959. [http://dx.doi.org/10.1542/peds.2011-1365] [ Links ]
5. Velaphi SC, Mokhachane M, Mphahlele RM, Beckh-Arnold E, Kuwanda ML, Cooper PA. Survival of very-low-birth-weight infants according to BW and gestational age in a public hospital. S Afr Med J2005;95(7):504-509. [ Links ]
6. Pattison RC. Saving Babies 2006-2007: Sixth Perinatal Care Survey of South Africa. Pretoria: Tshepesa Press, 2009. [ Links ]
7. Lawn JE, Cousens S, Zupan J. 4 million neonatal deaths: When? Where? Why? Lancet 2005;365(9462):891-900. [http://dx.doi.org/10.1016/S0140-6736(05)71048-5] [ Links ]
8. Ballot DE, Chirwa TF, Cooper PA. Determinants of survival in very low birth weight neonates in a public sector hospital in Johannesburg. BMC Pediatr 2010;10:30. [http://dx.doi.org/10.1186/1471-2431-10-30] [ Links ]
9. Fanaroff AA, Stoll BJ, Wright LL, et al. Trends in neonatal morbidity and mortality for very low birthweight infants. Am J Obstet Gynecol 2007;196(2):147.e1-147.e8. [http://dx.doi.org/10.1016/j.ajog.2006.09.014] [ Links ]
10. Westby Wold SH, Sommerfelt K, et al. Neonatal mortality and morbidity in extremely preterm small for gestational age infants: A population based study. Arch Dis Child Fetal Neonatal Ed 2009;94(5):F363-367. [http://dx.doi.org/10.1136/adc.2009.157800] [ Links ]
11. Narayan S, Aggarwal R, Upadhyay A, Deorari AK, Singh M, Paul VK. Survival and morbidity in extremely low birth weight (ELBW) infants. Indian Pediatr 2003;40(2):130-135. [ Links ]
12. Miller SS, Lee HC, Gould JB. Hypothermia in very low birth weight infants: Distribution, risk factors and outcomes. J Perinatol 2011;31(Suppl 1):S49-56. [http://dx.doi.org/10.1038/jp.2010.177] [ Links ]
13. Ogunlesi TA, Ogunfowora OB, Adekanmbi FA, et al. Point-of-admission hypothermia among high-risk Nigerian newborns. BMC Pediatr 2008;8:40. [http://dx.doi.org/10.1186/1471-2431-8-40] [ Links ]
14. Deulofeut R, Sola A, Lee B, Buchter S, Rahman M, Rogido M. The impact of vaginal delivery in premature infants weighing less than 1,251 grams. Obstet Gynecol 2005;105(3):525-531. [http://dx.doi.org/10.1097/01.AOG.0000177746.64361.04] [ Links ]
 Correspondence: E Kalimba (eddiekalimba@yahoo.co.uk)
Correspondence: E Kalimba (eddiekalimba@yahoo.co.uk)














