Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Bioethics and Law
versión On-line ISSN 1999-7639
SAJBL vol.16 no.2 Cape Town ago. 2023
http://dx.doi.org/10.7196/sajbl.2023.v16i2.1015
ARTICLE
Changes in the empathy levels of a group of undergraduate medical students: A longitudinal study
E ArcherI; R TurnerII
IPhD; Centre for Health Professions Education, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
IIMSc Nursing; Research assistant for Centre for Health Professions Education, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
ABSTRACT
BACKGROUND: The concept of empathy in students has gained significant attention in medical education. Whether implementing formal educational interventions to promote long-term and effective empathy levels leads to sustained increased empathy levels in students, is however less clear
OBJECTIVES: The study aimed to evaluate the trajectory of medical students' self-perceived empathy levels during their 6-year MB ChB degree
METHODS: A longitudinal, prospective study was conducted over 4 years. A cohort of 292 medical students was invited to participate. Participants completed the Jefferson Scale of Empathy for Students (JSE-S) at three intervals during their studies. The students attended two workshops related to empathic patient interactions during this time. The JSE-S mean score by age and gender was compared, making use of a linear regression model
RESULTS: A total of 119 students completed the study. Students' total empathy levels were similar during the first and the last measuring point (110), but there was a significant rise in the intermediate measuring point (113.3). When the male and female cohorts' scores were interpreted separately, both genders demonstrated a similar pattern to the total score, although females' JSE-S scores were higher than the males
CONCLUSION: The results of the study confirm that educational interventions can increase students' self-perceived empathy levels; however, we suggest that students require reinforcement and multiple opportunities to practise and observe empathic communication with patients to sustain high levels of empathy. Follow-up sessions to specifically target the promotion of empathy should be implemented; otherwise the long-term effect of educational interventions might be limited
Medical practitioners who demonstrate empathy during their interactions with patients evidently deliver core medical tasks more effectively. Showing empathy during consultations, has the potential to increase patient satisfaction and improve clinical outcomes.11,21 Moreover, studies have shown that clinicians who practise empathic patient care experience greater job satisfaction[3] and are potentially less inclined to burnout.[4] However, despite the conscious incorporation of empathy training and practice in healthcare globally, no consensus has been reached on a clear definition of empathy. Empathy in the context of medical care is often labelled as clinical empathy. One definition for clinical empathy that is often cited is that of Hojat et al.,[5] who allude to empathy as a balance between affective and cognitive aspects in the doctor-patient interaction. Recently, Tan et al.[6] conducted a study among healthcare workers and patients, and defined clinical empathy as 'a sense of connection between the healthcare worker and the patient as a result of perspective-taking arising from imaginative, affective and cognitive processes, which are expressed through behaviours and good communication skills that convey genuine concern'. While the literature offers various definitions of empathy, it is reassuring to note that most of the studies evidently found that empathy can be taught and supported by means of educational interventions. [7,8] This evidence has prompted most medical schools internationally to incorporate various educational interventions with the aim of promoting empathy among medical students. These interventions vary, from workshops, watching movies, reflecting on personal experiences, reading literature, to many others.[9] Authors have further suggested that the teaching and learning of empathy should not be presented as once-off interventions, but should be integrated and reinforced over various years in both the classroom and clinical areas.[101 Owing to the importance of empathy for medical practice and the inclusion of empathy teaching in many curricula, various institutions have conducted research to report on the trajectory of empathy levels of their medical students.[11-13] While anticipating that senior medical students would become more empathic, results are inconsistent as most of these studies demonstrated either an empathy decline or mixed results.[14,15] Most of the reported studies originate from countries in the northern hemisphere, and it is therefore uncertain whether these results are similar for medical students in South Africa (SA).
The measurement of empathy levels utilising an internationally accepted tool, the Jefferson Scale of Empathy for Students (JSE-S),[5] can provide opportunities to compare the empathy levels of medical students in our institution with global results. We are aware of two studies in SA that reported on the validity of the JSE-S in our context; however, both studies were cross-sectional studies.[16,17] This paper presents the longitudinal results of empathy levels of a cohort of medical students at Stellenbosch University, SA, by utilising the JSE-S tool. The aim was to evaluate the trajectory of undergraduate medical students' empathy levels across 4 years (2018 - 2021).
The medical programme at Stellenbosch University is a 6-year curriculum that has an annual intake of approximately 300 first-year students. The principles of patient-centredness and communication skills are introduced early in the curriculum as part of both theory and clinical blocks. The students are exposed to short interaction opportunities with patients during the first 2 years of study. During the third year of study, they experience longer interaction opportunities with patients in a tertiary hospital setting. From the fifth year onwards, students mostly work in the clinical areas with few theoretical classes.
Since 2018, additional educational interventions, which focused on empathy specifically to provide the students with opportunities to practise empathy skills and highlight the need for self-care and compassion, were introduced as part of the curriculum. These interventions occurred in a simulated environment, focusing on non-verbal messaging, as well as exercises designed to provide experience in effective listening, identifying non-verbal body language, and exploring alternative perspectives with simulated patients. In addition, students were presented with an opportunity of self-compassion after engaging with a difficult emotion.[10] We need to consider, however, that owing to the disruption of COVID-19, these specific students were not permitted to be on campus or to enter any clinical areas, for approximately 5 months during their fifth year of study.
Methods
This was a longitudinal, prospective study conducted over 4 years, which aimed to evaluate the trajectory of medical students' self-perceived empathy levels during their 6-year medical degree. The cohort of students who participated in the study was the third-year class of 2018 (n=292). These students were exposed to two new educational interventions as part of the formal curriculum that aimed to enhance knowledge and skills related to empathic patient interactions, one in year three and the other in year four. The JSE-S instrument was completed at three intervals during their training: at the start of year three, in the middle of year four, and again during year six. The implementation of the COVID-19 lockdown in SA meant students were unable to complete the JSE-S during their fifth year. Students were asked to complete hard copies during various classes in the Simulation and Clinical Skills Unit (SCSU). Staff members from the SCSU, who were not involved in the research, were responsible for getting the the students to complete the JSE-S instrument and collecting the data. The data were captured by an administrator onto an Excel spreadsheet after which a statistician assisted with the analysis. A breakdown of student age, gender and year was summarised in a descriptive table and a mixed linear regression model was used to compare the mean JSE-S across age (at 2018) and gender categories to account for the repeated JSE-S responses within students. The significance of the interaction effect between age, gender and year was tested, but since these effects were not significant, only the main effects are reported. The estimation of the age and gender effects was conducted using full maximum likelihood to serve as the imputation model for missing data in the cohort.
Data collection
We used the JSE-S since it is the most widely used measure for medical empathy.[18] It is a 20-item validated instrument specifically developed to measure empathy in the context of patient care in health professions students.[5] It is scored on a 7-point Likert scale (1 = totally disagree, 7 = totally agree). The possible scores range from 20 to 140 points, with the highest scores associated with a greater degree of empathy. While there is typically no time limit for students when they complete the instrument, it is usually completed within 10 minutes. The tool has three dimensions, namely, patient perspective taking, compassionate care, and standing in the patient's shoes. We previously validated the instrument for our context with the same cohort of students during 2018 and the Cronbach's a was reported as 0.81.[17] Permission to use the JSE-S was obtained from Thomas Jefferson Medical College. No changes were made to the original instrument.
Ethical considerations
We obtained ethical approval (N18/01/001) from the Health Research Ethics Committee at Stellenbosch University. Participation was voluntary and students provided informed consent before data collection commenced. Students were assured that there would be no negative consequences if they did not participate in the research.
Results
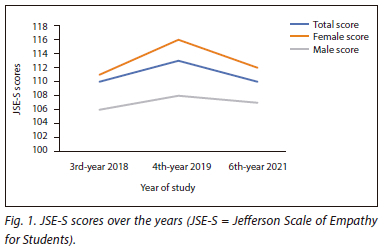
Students completed the JSE-S during 2018, 2019 and 2021. Data were not gathered during 2020 because of the COVID-19 crisis. The mean JSE-S scores per year, as well as by gender and age, are reported below. The mean total JSE-S score increased significantly from 2018 to 2019 and then declined to the same level as during 2018. These were measured during 2021 (Fig. 1). The female students had the same trend in the mean score as the total mean score, with a sharper increase and then showed a decline after a year, while the men's total score increased gradually from 2018 to 2019 and then declined narrowly in 2021.
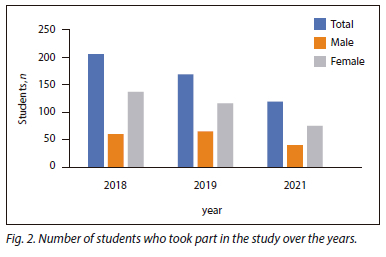
As is often the case with longitudinal studies, the number of students that participated in the study annually decreased (2018: n=206, 2019: n=169, 2021: n=119). As indicated in Fig. 2, more females participated (2018: n=137, 2019: n=102, 2021: n=75) than males (2018: n=60, 2019: n=65, 2021: n=40); this was not surprising, as it is representative of the gender demographics of the class. For each year there were students who did not complete the gender category on the JSE-S questionnaire. We included them in our total but not according to gender (2018: n=9, 2019: n=2, 2021: n=4).
It was evident that students who were older than 25 years had a higher mean JSE-S score than their younger peers (Table 1). Five students in the 2018 cohort did not complete the age category; therefore they were included as unknown, as indicated in Table 1.
Mixed effects linear regression result
For this analysis the JSE-S scores of 275 medical students were linked over the 3 years where available. The JSE-S mean scores were significantly associated with age (2018), gender and year, but none of the interactions were associated. The older participants (>25 years) in the cohort had a higher mean JSE-S score than the youngest age group (<22 years) with a mean difference of 6.4 units (95% confidence interval (CI) 1.0 - 11.7; p=0.020), whereas the age group 22 - 24 and the younger age group were not significantly different (p=0.905. Females had a higher mean JSE-S compared with males, mean difference = 6.3 units (95% CI 3.6 - 9.1; p<0.001). The year effect was non-linear, with a significant increase between 2018 and 2019, mean difference = 3.4 units (95% CI 1.6 - 5.3; p=0.0003, and a significant decline between 2019 and 2021, mean difference = -2.9 units (95% CI -5.4 - -0.5; p=0.0198. The mean JSE-S difference between 2018 and 2021 was not significant (p=0.682).
Discussion
This paper reports the JSE-S score of the same cohort of medical students over a period of 4 years of their study (years three to six). The results showed that the total level of empathy increased from study year three to four, and then declined during their sixth year to the original score during year three. By interpreting the male and female cohorts' scores separately, both genders demonstrated a similar pattern to the total score, although females' JSE-S score were higher than the males'.
The baseline JSE-S measurement of 110 compares well with data presented by Kataoka et al.,[19] who report on a longitudinal study of medical students. They reported that the JSE-S empathy score in male students did not change much over time and the significant changes reported for the whole group appear to have been influenced by the empathy score changes among the female students. It is well known that women score higher on empathy scales[20] because stereotypically women are perceived as more nurturing. Vallabh[16] also found a statistically significant difference in the mean empathy scores between female and male students. Bleakley et al.[21] reported that women show stronger patient-centred values which does not fluctuate over time. In addition, there is a neurobiological basis for these gender differences, probably due to evolutionary gender roles which result in differences in basic brain networks involved in affective and cognitive forms of empathy.[22]
Gallagher et al.[23] evaluated teaching empathy to medical students and compared the results with a group of nursing students who had had no specific intervention, and concluded that isolated teaching interventions are of no value as empathy is something which is'caught, not taught'. While we recognise that being empathic is learned by students seeing it in action, the literature suggests that there is value in sensitising students to the need for empathy and awareness of non-verbal cues, role modelling empathic communication skills to patients, and for dealing compassionately with their own difficult emotions.[10] In a previous study[10] we conducted focus group discussions with the same group of students during year four of their study. They highlighted the value of strong empathic role models in the clinical environment, as well as the value of positive feedback from patients when they engaged empathically.[10] We are unsure regarding the level of impact of COVID-19 owing to limited or no learning opportunities and exposure for students to engage with patients. Patient contact is important for the development of empathy.[241 During this period, some students had opportunities to assist with contact tracing and other COVID-19 support structures; however, these engagement processes were usually authoritative, directive, and prescriptive, which further reduced opportunities to practise empathic communication and to observe empathic behaviour. There is a risk that modelling of a more paternalistic style of medical encounter,[21] as well as the lack of meaningful contact, can increase the perceived distance between student and patient, resulting in an erosion of empathy.[25]
Many studies have been published regarding various educational interventions to develop empathy in healthcare students.[9,26] One of the limiting factors in our context is resources, especially with regard to lecturers facilitating small group sessions and the available number of simulated patients who can provide feedback to students. It is reassuring though to see that some institutions have managed to be innovative without making use of multiple resources. In these instances, they used DVD-based learning packages to teach and sustain empathy levels.[27] From our experience we managed to reduce didactic sessions by incorporating a flipped classroom and a blended learning approach for some of the theory regarding the concepts of empathy within health professions education.[10]
Strengths and limitations of the study
A limitation of the study is that data were collected at a single institution with undergraduate medical students. While we strived to make use of a well-established self-report measure, there could still be inherent reporter biases present. The major strength lies in the fact that largely the same cohort of students was involved in the study. This provided us the opportunity to monitor the trajectory of their empathy levels over a period of 4 years. The study had a major co-intervention with the national lockdown due to COVID-19 in 2020, and the impact of the students engaging in much less patient contact time compared with previous year groups cannot be estimated; however, the decline in self-perception of empathy levels can perhaps partially be ascribed to this.
Conclusion
This study confirms that educational interventions aimed at empathy in an undergraduate medical curriculum can increase students' self-perception of empathy. The fact that students need reinforcement and the opportunity to practise and observe empathic communication with patients in authentic clinical settings should however not be undervalued. Therefore, to sustain the long-term levels of empathy of medical students, curriculum developers need to map and plan strategic educational interventions throughout the early as well as the later clinical years of the curriculum.
The study highlights a need for further research focusing on specific interventions that can assist undergraduate medical students to sustain their levels of empathy and also the effect that role models with a paternalistic style of medical encounter can have on the perceived empathy of undergraduate medical students.
Declaration. None.
Acknowledgements. We would like to thank the MB ChB class of 2021 for their willingness to participate in the study. We are grateful to Dr Carl J. Lombard from the Division of Epidemiology and Biostatistics, University of Stellenbosch, for his assistance with the statistical data. Thanks to Jefferson Medical College for granting us permission to use the JSE-S for this study.
Author contributions. Both authors contributed equally to the work. EA led the conceptual phase and the research and RT led the manuscript preparation.
Funding. This work was partly funded by the Centre for Teaching and Learning, Stellenbosch University, Teaching and Learning Fellowship.
Conflicts of interest. None.
References
1. Levinson W, Gorawara-Bhat R, Lamb J. A study of patient clues and physician responses in primary care and surgical settings. JAMA 2000;284(8):1021-1027. https://doi.org/10.1001/jama.284.8.1021
2. Zachariae R, Pedersen CG, Jensen AB, et al. Association of perceived physician communication style with patient satisfaction, distress, cancer-related self-efficacy, and perceived control over the disease. Br J Cancer 2003;88(5):658-665. https://doi.org/10.1038/sj.bjc.6600798
3. Lamiani G, Dordoni P Vegni E, Barajon I. Caring for critically ill patients: Clinicians' empathy promotes job satisfaction and does not predict moral distress. Front Psychology 2020;10:2902. https://doi.org/10.3389/fpsyg.2019.02902
4. Shanafelt TD, West C, Zhao X, et al. Relationship between increased personal well-being and enhanced empathy among internal medicine residents. J Gen Intern Med 2005;20(7):559-564. https://doi.org/10.1111/j.1525-1497.2005.0108.x
5. Hojat M, Gonnella JS, Nasca TJ, et al. Physician empathy: definition, components, measurement, and relationship to gender and specialty. Am J Psychiatry 2002;159(9):1563-1569. https://doi.org/10.1176/appi.ajp.159.9.1563
6. Tan L, Le MK, Yu CC, et al. Defining clinical empathy: A grounded theory approach from the perspective of healthcare workers and patients in a multicultural setting. BMJ Open 2021;11(9):e045224. https://doi.org/10.1136/bmjopen-2020-045224
7. Jeffrey D, Downie R. Empathy - can it be taught? J Royal Coll Physicians Edin 2016;46(2):107-112. https://doi.org/10.4997/JRCPE.2016.210
8. Kelm Z, Womer J, Walter JK, Feudtner C. Interventions to cultivate physician empathy: A systematic review. BMC Med Educ 2014;14(1):1-11. https://doi.org/10.1186/1472-6920-14-219
9. Batt-Rawden SA, Chisolm MS, Anton B, Flickinger TE. Teaching empathy to medical students: An updated, systematic review. Acad Med 2013;88(8):1171-1177. https://doi.org/10.1097/ACM.0b013e318299f3e3
10. Archer E, Meyer IS. Applying empathic communication skills in clinical practice: Medical students' experiences. South Afr Family Pract 2021,63(1):5244. https://doi.org/10.4102/safp.v63i1.5244
11. Hojat M, Vergare MJ, Maxwell K, et al. The devil is in the third year: A longitudinal study of erosion of empathy in medical school. Acad Med 2009,84(9):1182-1191. https://doi.org/10.1097/ACM.0b013e3181b17e55
12. Chen D, Lew R, Hershman W, Orlander J. A cross-sectional measurement of medical student empathy. J Gen Intern Med 2007,22(10):1434-1438. https://doi.org/10.1007/s11606-007-0298-x
13. Chen DC, Kirshenbaum DS, Yan J, Kirshenbaum E, Aseltine RH. Characterizing changes in student empathy throughout medical school. Med Teach 2012,34(4):305-311. https://doi.org/10.3109/0142159X.2012.644600
14. Papageorgiou A, Miles S, Fromage M. Does medical students' empathy change during their 5-year MB BS degree? Educ Health 2018,31(3):142.
15. Spatoula V, Panagopoulou E, Montgomery A. Does empathy change during undergraduate medical education? A meta-analysis. Med Teach 2019,41(8):895-904. https://doi.org/10.1080/0142159X.2019.1584275
16. Vallabh K. Psychometrics of the student version of the Jefferson Scale of Physician Empathy (JSPE-S) in final-year medical students in Johannesburg in 2008. S Afr J Bioethics Law 2011,4(2):63-68.
17. Archer E, Turner R. Measuring empathy in a group of South African undergraduate medical students using the student version of the Jefferson Scale of Empathy. Afr J Primary Health Care Fam Med 2019,11(1):1-5. https://doi.org/10.4102/phcfm.v11i1.1956
18. Blanco JM, Caballero F, Álvarez S, Plans M, Monge D. Searching for the erosion of empathy in medical undergraduate students: A longitudinal study. BMJ Open 2020,10(12):e041810. https://bmjopen.bmj.com/content/10/12/e041810
19. Kataoka H, Iwase T, Ogawa H, et al. Can communication skills training improve empathy? A six-year longitudinal study of medical students in Japan. Med Teach 2019,41(2):195-200.
20. Berg K, Majdan JF, Berg D, Veloski J, Hojat M. Medical students' self-reported empathy and simulated patients' assessments of student empathy: An analysis by gender and ethnicity. Acad Med 2011,86(8):984-988. https://doi.org/10.1097/ACM.0b013e3182224f1f
21. Bleakley A, Bligh J, Browne J. Let's get real: Medical students learning from, with and about patients. In: Medical Education for the Future. Advances in Medical Education. Dordrecht: Springer, 2011,1:187-200. https://doi.org/10.1007/978-90-481-9692-0_13
22. Christov-Moore L, Simpson EA, Coudé G, Grigaityte K, Iacoboni M, Ferrari PF. Empathy: Gender effects in brain and behavior. Neurosci Biobehav Rev 2014,46:604627. https://doi.org/10.1016/j.neubiorev.2014.09.001
23. Gallagher P, Moriarty H, Huthwaite M, Lim B. Challenging some assumptions about empathy. Clin Teach 2017,14(6):437-440. https://doi.org/10.1111/tct.12607
24. Light A, Gupta T, Burrows A, Nandakumar M, Daniel A, Karthikeyan S. Learning empathy: The medical student perspective. Clin Teach 2019,16(1):76-77. https://doi.org/10.1111/tct.12801
25. Southworth E, Gleason SH. COVID 19: A cause for pause in undergraduate medical education and catalyst for innovation. HEC Forum 2021,33(1):125-142. https://doi.org/10.1007/s10730-020-09433-5.
26. Stepien KA, Baernstein A. Educating for empathy. J Gen Intern Med 2006,21(5):524-530. https://doi.org/10.1111/j.1525-1497.2006.00443.x
27. Williams B, Brown T, McKenna L, et al. Student empathy levels across 12 medical and health professions: An interventional study. J Compassionate Health Care 2015,2(1):1-6. https://doi.org/10.1186/s40639-015-0013-4
 Correspondence:
Correspondence:
E Archer
elizea@sun.ac.za
Accepted 17 July 2023














