Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
Journal of Contemporary Management
versão On-line ISSN 1815-7440
JCMAN vol.10 no.1 Meyerton 2013
RESEARCH ARTICLES
Electronic health records: managing the transformation from a paper-based to an electronic system
Dr RV Weeks
University of Pretoria
ABSTRACT
South Africa has taken the first steps in implementing a National Health Insurance (NHI) scheme. An electronic health record (EHR) system will form a vital component of the infrastructure that needs to be put into place for managing healthcare services. Even a brief review of the literature reveals that managing the transformation from a paper-based to an electronic based system is complex in nature, as it entails a fundamental change in the healthcare culture. Consequently, in many instances such systems do not fully realise the benefits and objectives envisaged. With this in mind, this research study focuses on gaining an insight into to complexities and challenges involved in implementing an EHR system, taking the current South African situation into consideration. The research study constitutes a multi-disciplinary literature review and a limited in scope and extent narrative enquiry. The purpose of the latter being an attempt to validate some of the insights gained from the literature. The value of the research study stems from the fact that an EHR system will form an essential component of the NHI initiatives supporting infrastructure and the insights gained from the research study could inform the project's management strategy.
Key phrases: change management; electronic healthcare record; enterprise content management; organisational culture.
1. BACKGROUND
"Often, the process of transitioning from paper to an EHR seems so daunting that it can appear to be unachievable. The process is complex. However, when the paper-to-digital transition is compartmentalized into manageable tasks, the process is achievable. " Hartley 2010:32
Hartley's (2010:32) introductory statement attests not only as to the complexity associated with the implementation of an EHR system, but also the need for identifying the strategic dimensions that need to be addressed in managing the transformation from paper to an electronic format. This transition entails far more than the identification and implementation of the technology systems concerned, it necessitates a need to manage the human dimensions of change that essentially is instrumental in assigning the "complex" connotation to the change management process involved. Munir and Kay (2003:484) also note that in practice many such systems are not fully exploited and again, as suggested by the researcher, it is the human and healthcare culture related issues that constitute the neglected aspect of electronic patient record system implementation.
Harrison, Koppel and Bar-Lev (2007:542), on a more general basis, specially claim that "a growing body of research and user reports reveals many unanticipated and undesirable consequences of implementation", thereby also attesting to the complexity involved in implementing EHR systems. Anderson and Anderson (2010:5) similarly state that over the past two decades 70 present of all change efforts fail to deliver their intended outcomes and according to the researchers this could be attributed to the people concerned "viewing transformation through old mindsets with limited critical awareness and applying traditional management approaches that just do not work".
Despite the apparent complexity and challenges associated with its implementation and utilisation, it is stressed by Gelmon and Droppers (2008:1, 6) that information technology still offers the "best hope for the future of health care" as it allows providers to "electronically create, store, organize, edit and retrieve patient medical records", thereby enabling enhanced healthcare service delivery at the point of care.
This brief introductory literature review captures a few very fundamental truths, namely that EHR systems implementation, utilisation and management embodies far more that technology related issues. It embodies complex issues such a transition in traditional thinking, management, and ways of doing things within healthcare settings. This notwithstanding, it is frequently argued that the advantages associated therewith far outweigh the initial difficulties encountered. Seen in the context of South Africa's implementation of the National Health Insurance initiative this research study endeavoured to gain an understanding of the complexities and challenges associated with the implementation of EHR systems. The objective is well summarised by Gelmon and Droppers (2008:2): "no community health centre should have to rediscover an avoidable problem".
The research methodology adopted in conducting the research study constitutes of a multi-disciplinary literature review in order to gain an insight into the difficulties encountered in practice and possible means for addressing these. In addition interviews were conducted with a limited sample of four ICT practitioners involved in the implementation of EHR systems and seven physicians in the use thereof. The narrative enquiry was specifically undertaken so as to verify insights gained from the literature review. In effect the research study was therefore analytically descriptive and qualitative in nature.
In the ensuing sections conceptual clarity is attained as to the concept "EHR systems", the difficulties encountered in implementing, managing and utilising the systems, and the best means of addressing or managing these transformational difficulties. In order to gain an insight into the South African context of EHR implementation a brief review of the current NHI implementation situation is also provided.
2. DEFINITION OF THE CONCEPT "EHR"
"The Electronic Health Record (EHR) is a longitudinal electronic record of patient health information generated by one or more encounters in any care delivery setting. Included in this information are patient demographics, progress notes, problems, medications, vital signs, past medical history, immunizations, laboratory data, and radiology reports. The EHR automates and streamlines the clinician's workflow. The EHR has the ability to generate a complete record of a clinical patient encounter, as well as supporting other care-related activities directly or indirectly via interface-including evidence-based decision support, quality management, and outcomes reporting."
Health Information Management Systems Society
In The Mitre Corporation 2006:1
The introductory definition of EHRs, cited by The Mitre Corporation (2006:1), is quite extensive in nature and incorporates an extended list of patent centric healthcare information sources. Specifically noted in the definition is also the fact that it constitutes a longitudinal electronic record, implying that it captures both past and current emergent sources of information. In defining an EHR, Gartee (2011:4) citing Murphy, Walters, Hanken and Pfeiffer, also specifically suggests that it includes "any information relating to the past, present or future physical/mental health, or condition of an individual which resides in electronic system(s) used to capture, transmit, receive, store, retrieve, link and manipulate multimedia data for the primary purpose of providing healthcare and health-related services".
In so doing not only "what" information is stored is addressed, but also what can be done with this data is elaborated on in defining the concept. The versatility associated with the use of "electronic systems" becomes quite clear from the definitions and this often features in the advantages cited by researchers in regard to electronic systems over traditional paper-based systems. The motivation in essence assumes a patient centric incentive of enhanced healthcare safety and service delivery, at a reduced cost (Gartee 2011:5,14; Xue, Liang, Wu, Gong, Li & Zhang 2012:684).
In defining EHRs Garrett and Seidman (2011:Internet) draw a distinction between EHRs and Electronic Medical Records (EMR), which they acknowledge are often used interchangeably within the literature. They suggest that EMRs are a digital version of the paper charts in the clinician's office, while EHRs focus on the total health of the patient and go beyond standard clinical data collected in the provider's office and provide a more inclusive broader view on a patient's care (Garrett & Seidman (2011:Internet).
This wider connotation of EHRs is certainly manifested in definitions attributed to the concept, where the accent is on diverse sources of information generation, such as physicians, laboratories, radiology, specialists, nurses, and pharmacies, and a sharing of the information concerned where relevant (The Mitre Corporation 2006:3). There are, however, definitions attributed to EMR systems that capture this wider total patient centric health information connotation, as may be seen from the ensuing description of such systems by Spratt and Dickson (2008:21):
"EMR systems represent a departure from traditional paper records keeping in that they include patient demographics, medical histories, and all records of patient treatment stored in a computerized format. When coupled with network systems and the Internet, the EMR platform offers versatility in terms of transferability of information, greater communication among doctors, and improvement in quality of care, just to name a few advantages".
The preceding EMR definition will be seen to essentially resonate with that previously attributed to EHR systems and thus the distinction alluded to by Garrett and Seidman (2011 :Internet) may not be all that fundamental in practice. For the purposes of this paper they are considered to be very similar in nature and definition. Chang (2011:580) adopts a similar interpretation in contending that both embody similar characteristics.
3. ANALYSIS OF THE CONCEPT "EHR"
Emphasized in the Spratt and Dickson (2008:21) definition is the fact that EMRs constitute a definite departure from traditional paper records. It is also worth noting at this stage that Spratt and Dickson (2008:25) also affirm that "while EMR technology has been around for several years, the majority of hospitals and private clinics have still yet to adopt such systems". A common problem encountered in terms of this wider definition inferred connotation of interoperability and the transferability of patient centric information is the need for generally accepted standards. In this regard Jin, Ahn, Hu, Covington and Zhang (2011:116) state that there are several standards currently under development to structure and specify the clinical content of an EHR, such as openEHR and HL7. A more extensive analysis of standards for interoperability does not, however, form a key focus of this paper and it is but noted from a definition implication perspective.
Ariffin, Yunus and Embi (2008:51) view EMRs as constituting the primary record of care meeting all clinical, legal and administrative requirements, which implies that it is more than an electronic version of the paper record. It is seen as being a structured and integrated approach to managing patient information, resulting in a reduction of incomplete charts and the waiting time for paper-based test results, but with concern for patient privacy, confidentiality and security (Ariffin et al. 2008:51). In so describing the concept Ariffin et al. (2008:51) draw attention to the evolution of the concept and the terms used for referencing the concept, namely computerised patient records (CPR), computerised medical records (CMR), electronic medical records (EMR), electronic health records (EHR), and automated medical records (AMR) to but name a few.
In essence the systems are deemed to be cumbersome, unwieldy, unfriendly and opaque to the users and the patients, and according to Ariffin et al. (2008:51) they could better be described as complex adaptive systems that have evolved over the space of time. The researchers' description and definition would appear to also add aspects not previously alluded to such as the concern for patient confidentiality. Each of the definitions' attributed to the concept would therefore seem to add an aspect, that seen in a collective sense, would appear to enrich our understanding of the concept. Yet the notion of patient centric health information remains a key factor, while electronic-based technology, it is asserted by Ariffin et al. (2008:56) smooth the linkages between information and patient care by providing access to the rich information environment.
With the preceding conceptualisation of EHR systems as well the potential advantages that may be derived therefrom kept in mind, it is important to observe that Mars and Seebregts (undated:4) have found that only a third of South African provincial hospitals have some form of functioning electronic medical record system. They further claim that a multiplicity of systems exist both within the public and private sector and interoperability, as intimated within the definitions, would therefore seem to be elusive in practice. The National Department of Health's (NDOH) (2012:14) e-strategy document confirms that South African "EMR record systems are somewhat functional in just one-third of provincial hospitals" and that there are currently "five different proprietary systems in use with little integration between them".
It is also stated in the document that "the private sector also faces the same problem of fragmented systems" (National Department of Health 2012:14), thereby confirming the research findings of Mars and Seebregts (undated:4). As a consequence the NDOH has made a strategic decision to implement a national EHR system to address the issue of a lack of interoperability and fragmentation (National Department of Health 2012:15). The preceding definitions' attributed to EHR systems collectively could inform the understanding of what constitute such systems in this endeavour that yet needs to be clearly articulated from a design, implementation, management and use perspective. Also of pertinence in the document is the mention that technical standards are required to ensure national and international compatibility, interoperability, open architecture, modularity and capacity for upgrade (National Department of Health 2012:16).
4. MANAGING THE TRANSITION FROM PAPER-BASED TO EHR SYSTEMS
"Alongside regulatory requirements for records retention, hospitals are faced with moving forward with electronic charts while needing to manage the information contained in paper charts gathered during the transition so that they can be made available to caregivers. This challenge creates the need for hospitals and practices moving to the EHR to consider and adopt a records transition strategy that allows them to access historical data while moving forward with their EHR. "
Hanover 2011:2
Historically, a patient's medical record consisted of handwritten notes, typed reports, and test results stored in a paper file system (Gartee 2011:14). A separate file was created and stored at each healthcare facility and radiological records were typically stored separately (Gartee 2011:14). A vast number of paper-based patient records have consequently come into being and as reflected in the introductory quotation by Hanover (2011:2) regulatory requirements necessitate that such records be retained for prescribed periods of time. Capturing these records in electronic format to facilitate interoperability, without doubt, would entail a very extensive and time consuming process. Interviews conducted with South African doctors, both in public and private sector healthcare facilities reveal that paper based records are still frequently used in practice, a realty that may also be inferred from the National Department of Health's (2012:14) e-strategy document.
The transition from paper-based to EHR records, from a strategic perspective, would need to address the issue of the existence of paper-based EMRs, while simultaneously introducing and moving over to an EHR system. This needs to be seen in the context of Jin et al.'s (2011:116) contention that in modern healthcare environments, a fundamental requirement for achieving continuity of care is the seamless access to distributed patient health records in an integrated and unified manner, directly at the point of care. It also accentuates the motivation for a structured and integrated phased approach in managing the transition.
The College of Physicians and Surgeons of Alberta (2004:1) contend that medical records are an integral part of medical practice and moving to an electronic record system entails a very fundamental change in thinking and clinical processes. In a sense advocated is the notion of paper records forming part of clinical practitioners' administrative healthcare DNA, or as suggested by a physician interviewed in the course of this study, it forms part of the very life blood of the practice in terms of the "way that things are done". Williams and Boren (2008:141) would seem to concur with the expressed sentiment in alleging that "converting from a paper-based to an EMR system is complex and difficult because it represents a paradigm shift for the work of physicians and other staff".
The College of Physicians and Surgeons of Alberta (2004:1) similarly refer to it as representing "a paradigm change for the physician". Koriwchak (2010:Internet) quite pertinently alleges that most healthcare institutions fail to recognise that the biggest obstacle to EMR implementation are not financial, but are cultural, in that "the art and science of medicine defy, to some degree, traditional software structure and data capture techniques". A research study undertaken by Ilie, Courtney and Van Slyke (2007:8) found that EMR systems "did not seem very compatible with the way the family practitioners liked to practice" and most of the resident physicians interviewed mentioned that they would use paper if that was an option, both in the clinic or in their future practice". Hersh (1995:773) also concludes that despite the documented benefits associated with EHR systems "most clinical encounters are still recorded by hand in a paper record".
McGinn, Grenier, Duplantie, Shaw, Sicotte, Mathieu, Leduc, Légaré and Gagnon (2011:2) conducted a very extensive literature review and identified the most commonly encountered issues whichneeds to be addressed in EHR implementation, namely: privacy and security, cost, increased workload and time constraints, productivity, interoperability, professional interaction with patients, and a lack of familiarity with the system. Resistance to change, however, was found to feature as a particularly pertinent issue that needed to be addressed, an aspect accentuating the need for an effective change management strategy (McGinn et al. 2011:4). The most cited interaction change reported by clinicians and managers, according to McGinn et al. (2011:4), was a loss of both physical and relational contact with the patient due to interaction with the technology.
At the core of this concern is a well-established practice of paper-based medical records that does not distract from the physicians interaction with patients at the point of care. Based on their research findings Saleem, Russ, Justice, Hagg, Ebright, Woodbridge and Doebbeling (2009:619) similarly conclude that while some of the potential benefits of EHRs are well-known, they do not produce completely "paperless" processes and they assert that research alludes to the phenomenon as constituting "paper-persistence". Implied is an underlying paper-based culture of medical records that has evolved over an extensive period of time and come to be accepted as the way things are done in practice. So entrenched has this thinking become that in many instances, according to Saleem et al. (2009:619), it "may lead to paper-based workarounds".
The picture that emerges from the literature would seem to indicate a trend of paper-based medical record systems values, beliefs, norms and practices having become ingrained in medical practitioners' mindsets. Therefore necessitating what the College of Physicians and Surgeons of Alberta (2004:1) and Williams and Boren (2008:141) termed to be a paradigm change, in order to get the people concerned to make use of the EHR systems concerned.
So ingrained has this become that Ilie et al. (2007:8) found that most physicians, who for administrative purposes need to make use of EHR systems, "used workarounds such as documenting diagnoses and medications on the paper during the patient encounter, and then entering them in the computer system". A significant number of the South African doctors interviewed in the course of this research study expressed a similar sentiment of preferring to make use of paper-based systems and only using the EHR system for financial and administrative purposes. It is a trend that seems to have not gone unnoticed by the Western Cape Department of Health.
5. EHR's: AN ENTERPRISE CONTENT MANAGEMENT PERSPECTIVE
The Western Cape Department of Health first deployed an Enterprise Content Management (ECM) system at the Forensic Pathology Services, as well as within the Oncology unit at Tygerberg Hospital, and based on the success achieved subsequently rolled the system out at the Khayelitsha hospital. They are currently in the process of deploying the system across the whole of the Tygerburg hospital in Bellville Cape Town (Datacentrix 2012:8; Dicks 2012:Interview; Dorrington 2012:Interview).
It would seem that at the core of this success story is the fact that physicians and medical staff are still able to generate new content in the form of paper-based healthcare records that are then scanned into the ECM system. The ECM system provides a central repository for the electronic capture of the paper-based documents, with secure access control in a file structure using an indexing system that allows medical practitioners to rapidly access patient records using a few key indexing fields.
Dorrington (2012:Interview) indicated that one of the very positive factors associated with the success of the project was the elimination of "bottlenecks" previously encountered at admission, namely patients having to wait for paper-based files to be retrieved. Medical practitioners are now able to access patient records electronically, even before the patient enters the consulting room, thereby enriching the doctor / patient interaction and relationship. Dicks (2012:Interview) and Dorrington (2012:Interview) both were of the view, however, that being able to integrate a traditional healthcare culture of paper-based clinical records and notes with an electronic medical record format was one of the key determinants that gave rise to the successful adoption of the ECM system.
The Khayelitsha admission system and the use of "episode folders" is depicted in Figure 1. It brings together a well-established paper-based culture of medical records and the need for electronic document interoperability. A well-structured change management strategy forms an important dimension of the ECM system implementation, according to Dorrington (2012:Interview). Hartley (2010:35) also accentuates the fact that implementation needs to be a team effort that includes the EHR system vendor, the project manager, the information technology team and physician champions, an approach that it appears Dorrington (2012:Interview) and Dicks (2012:Interview) would concur with.
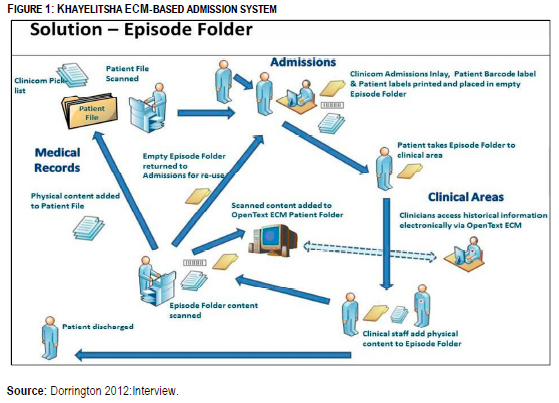
The transition process briefly alluded to in the discussion in effect entails a far less radical transformation. Dicks (2012:Interview) and Dorrington (2012:Interview) also confirm that staff training in the use of the ECM system constituted an important element of the change management strategy, directed at ensuring that users acquired the technology based skills for their specific job's functional requirements. Dicks (2012:Interview) and Dorrington (2012:Interview) also mentioned that a help desk was established to assist in instances where staff experienced difficulty. Clearly, the process depicted would seem to resonate with the literature finding that effective training and staff involvement forms a critical component of the EMR implementation process. This may typically be seen from Marcus, Lubrano and Murray's (2009:34) assertion that strong physician leadership and involvement, sufficient resources for both physician and staff training and patience to allow everyone to overcome the learning curve, are key ingredients for successful transformation to an electronic system.
6. CHALLENGES ASSOCIATED WITH THE DEPLOYMENT OF EHR SYSTEMS
Hersh (1995:773) attests to the fact that the financial management system modules incorporated within EHR systems serve as a major catalyst for the EHR system implementation. On the clinical side the most common computerised function is deemed to be laboratory reports. Discussions with South African doctors in private practice reveal a similar trend, namely with most making use of the electronic financial components of the EHR system to submit claims to medical aids. This has resulted in some instances in dual paper-based clinical and electronic financial records existing side-by-side at the same point in time. Only those clinical aspects, such as diagnostic and treatment codes, that have financial billing implications are being specifically recorded and captured in the EHR system.
Asked as to why they did not then just use the electronic system for capturing clinical information as well a number of issues surfaced, such as the previously discussed aspect of the computer systems in a sense being a disruptive element when they are examining and interacting with patients. Episode files or paper-based systems are seen as being far less disruptive and more user-friendly.
In support of this contention it is claimed by Zandieh, Yoon-Flannery, Kuperman, Langsam, Hyman, and Kaushal (2008:759) that practitioners are in effect reluctant to adopt new ways of doing things that interfere with their workflow and that take time away from patient care. In light of the preceding discussion it is not surprising to find that Zandieh et al. (2008:757) found that the main advantages of EHR systems cited by users of paper-based systems were: improved communication, an ability to have remote access of patient information, and improved revenue streams. Notably the first two advantages feature in the ECM system implemented at the Khayelitsha hospital as well.
The technology challenges associated with EHR implementation in the literature tend to also feature people related aspects such as training of healthcare practitioners in the utilising of the system and issues relating to technical support and, privacy and security of patient information (Buchan 2011:321; Boonstra & Broekhuis 2010:4; Zandieh et al. 2008:758).
The complexity associated with EHR system implementation it would seem is not really related to the technology, but the people aspects involved. There are technology aspects, such as system interoperability, standards used availability of computer equipment at points of patient care, and system reliability, that feature as well, but they are seen as being more complicated and not complex in nature, as they can dealt with on a logical ordered, structured and systemic basis. The people, cultural issues in contrast embody emotional and emergent properties that are far more complex to deal with.
From the literature as well as from the relatively restricted number of interviews conducted with practitioners, it would appear that it is the human or people related issues, and not really the technology issues, that result in the complexity associated with the management of moving from paper-based to EHR systems. In the ensuing section dealing with the management of these issues will be dealt with in more detail from a complexity theory basis.
7. MANAGING THE COMPLEX PEOPLE RELATED ASPECTS OF EHR SYSTEM IMPLIMENTATION
"When we understand culture as the meaning giving system of a society then it becomes a current ever evolving force which can best be experienced in active engagement with today's human beings as well as with local nature, not with yesterday's historical beings." Ronnie Lessem and Alexander Schieffer 2009:118
The introductory statement attests to the concept of culture being "a living system", thereby inferring that it is not cast in stone but able to evolve through active engagement within healthcare settings. From the preceding discussion it will have become evident that if the existing well-established values, beliefs, norms and mental models of healthcare practitioners are in conflict with that required for EHR systems, a definite change in the culture of the institution will be required. The only alternative, as in the case of the ECM system implemented at the Khayelitsha hospital, is that of designing and implementing the EHR system with the existing healthcare culture in mind. In researching the installation of EHR systems Lœrum, Karlsen and Faxvaag (2004:2).also found that a large number of legal and practical constraints, such as culture change, influence the design and introduction of the systems.
This often means that the paper-based counterpart is not eliminated in a single step. In such cases, healthcare practitioners have to deal with a hybrid electronic and paper based solution, as is the case at the Khayelitsha hospital. It is contended by Lœrum et al. (2004:2) that in many instances hospital EMR projects in Norway have not yet passed beyond this phase.
In the case of a fully-fledged EHR system implementation, however, a change in the existing culture will need to be engendered. In this regard it needs to be stated that there are researchers, such as Munck (2002:23), who suggests that transforming an organisation's culture is one of the most fundamental challenges confronting an institution, as people's natural inclination is to hold on to whatever feels familiar, even if confronted with better alternatives.
The importance attributed to the healthcare culture concept stems from the fact that it serves as a perceptual and behavioural determinant, thereby shaping clinical practice within healthcare institutions (Seel 2000:1; Tosti 2007:21). According to Boonstra and Broekhuis (2010:12), however, "although it is a very important part of a change process and interrelated with organizational working procedures" it is an "issue largely overlooked by researchers and implementers". Boonstra and Broekhuis (2010:12) go on to claim that "how to create an appropriate organizational culture for the use of EMRs is an important topic that deserves further research in learning how to implement EMRs successfully". Following a similar trend Crosnick (2012:Internet) argues that:
"Managing the cultural change process is critical to the success of implementing an EHR. In fact, implementing an EHR is not all about the system; it is about embracing the change necessary to integrate the EHR into how the physician practices medicine... Culture change must be an integral part of the EHR implementation project plan; it should not be taken on informally, nor should the need for it be put off or ignored".
8. EHR SYSTEM SYTEM IMPLIMENTATION: A CHANGE MANAGEMENT PERSPECTIVE
McCarthy and Eastman (2010:6) describes the change management process as being "messy" in that "people start where they are, not where we want them to be". They suggest that the personnel within a typical hospital, can be "all over the place" in terms of comfort with computers, stage in life, commitment to the organisation, and fear of change (McCarthy and Eastman 2010:6). McCarthy and Eastman (2010:6) indicate that in a metaphorical sense the transformation from a paper to an EHR system constitutes a journey of letting go of "current reality", going through a confused period in-between, and only then staring on a new beginning.
The description of the process, as being messy in nature, stems from the reality that it is essentially emergent in nature and does not really follow the traditional mechanistic Cartesian-Newtonian change management paradigm that has dominated management thinking for many years. Gebauer and Fleisch (2007:337) explicitly contend that the existing literature largely avoids the issue of having to deal with complex behavioural patterns, as a dimension of transformation management. Quite pertinently Mintzberg (1993:25) also asserts that the literature generally assumes an intentional or deliberate strategic approach, to the virtual exclusion of an emergent strategy.
9. CULTURE AS A DETERMINANT IN MANAGING THE TRANSTION TO AN EHR SYSTEM
Snowden (2005:2), in contrast to the more traditional view, very pertinently suggests that culture constitutes the patterning of our interactions with our environment and it is therefore not susceptible to intentional design principles. It is this more contemporary view of culture transformation that is not explicitly manifest in most of the literature relating to the management of EHR systems. It is maintained in this paper that the failure to realise the intended benefits associated with the implementation of EHR systems, in many instances, can be traced back to an adoption of traditional structured mechanistic processes, which includes culture change.
Yet researchers such as Weeks and Galunic (2003:1309), using a "meme" perspective, insinuate that healthcare facilities "are best thought of as cultures, as social distributions of modes of thought and forms of externalization". The researchers use the term "meme" to refer "collectively to cultural modes of thought (ideas, beliefs, assumptions, values, interpretative schema, and know-how), to describe culture as a social phenomenon, patterns of symbolic communication and behaviour that are produced as members of the group enact the memes they have acquired as part of the culture" (Weeks & Galunic 2003:1309).
It is a view that undoubtedly reflects a significant departure from the more mechanistic traditional Cartesian-Newtonian management approach of structured intentional culture transformation. Intimated, in contrast, is the notion of culture as a social phenomenon of patterns of symbolic communication and behaviour that emerge as members of the group enact the memes they have acquired as part of the culture (Weeks & Galunic 2003:1309).
Two very different constructs of culture transformation thus emerge, that of intentionally managed systemic change, and emergent complex adaptation. The former is well documented within the literature, but less well articulated is the more contemporary complex adaptive systems view deemed to be more effective in practice. In the ensuing brief discussion the focus will therefore be on this more contemporary postmodern view of culture realignment. Fard, Rostamy & Taghiloo (2009:46) articulate institutional culture as constantly evolving "along an infinite continuum in a harmonious learning environment", characterised by staff engaging in new emergent habits and routines, passing along corporate myths and stories, and in the process developing new shared jargon.
It is a view that Bennet and Bennet (2004:150) would endorse, as may be ascertained from their description of culture as an emergent phenomenon, namely taking place as "workers go about their daily business of communicating, solving problems, taking action, and reacting to information from others". The researchers allege that before an institution can adopt new practices to significantly change the way it conducts its business, such as would be the case in implementing an EHR system, it must be willing to admit that current practices are inadequate, which in essence requires a paradigm shift (Bennet & Bennet 2004:11). It is a contention that resonates with what McCarthy and Eastman's (2010:6) previously alluded in their description of the first phase of the journey, namely letting go of "current reality" so as to be able to develop a new shared understanding of EHR systems and new ways of doing things.
Notably, even the ECM system deployed at the Khayelitsha hospital entailed an element of culture change, but as expressed by respondents interviewed, the change was far less dramatic as it was welcomed by most of the people involved. The culture change was described by the respondents interviewed as being of an emergent nature. It was mentioned that the old system resulted in many difficulties that were addressed in the ECM system and even though it entailed an acquisition of new skills, these skills were seen in a positive light. An important aspect of the system is that it retains the positive aspects of a paper-based system, while incorporating the positive aspects associated with electronic document access and retrieval.
A sense of resiliency in dealing with the change emerged, in that the people concerned gained an awareness of the changes required and how they would impact in a positive sense on their day-to-day activities through a process of active engagement and involvement. As the people concerned interacted and made use of the ECM system a new set of shared beliefs, values, norms and ways of doing things therefore emerged over a relatively short space of time. An important aspect was that physicians were able to still make use of paper records and were not exposed to the negative aspects associated with the electronic system previously cited, such as having to enter the data in the computer system while attending to the patient. From a cultural transformation perspective, Bryson (2008:744) would describe the process that has taken place as one of allowing culture to be understood "as a dynamic, constantly negotiated phenomenon".
Culture viewed as emergent and shaped by negotiations and interactions taking place between the various agents involved would tend to stand in contrast to the traditional view of its active intentional management (Bryson 2008:745). The researcher, however, states that "post-modern approaches provide ample description and analysis but very few tools for action" (Bryson 2008:746). Citing Williams, Bryson (2008:747) theorises it as a "struggle between the dominant, residual and emergent cultures". In the context of this paper the dominant paper-based culture therefore being conceptualised as being in a "struggle" with the emergent EHR cultural system that needs to come into being.
The ECM approach adopted at the Khayelitsha hospital, of having the two being complimentary as opposed to conflicting, allows for the cultural transition to take place on a real time exploratory basis of negotiation as to what paper-based cultural aspects to retain and what to change in order to conform to the EHR or ECM system. It is argued that culture in this sense is not a static system and that to understand this dominant culture we need to understand both the process of selective tradition and the social process of incorporation (Bryson 2008:747).
A new dominant culture emerges by retaining aspects of the traditional culture and incorporating new emergent meanings, values, and practices found to be more effective. "Thus, hegemony of the effective dominant culture is characterised as a complex, multilayered negotiation and renegotiation of the emergent and residual cultures and of those cultures relative to the dominant culture" (Brynson 2008:748). An important aspect of emergent cultural theory is that it essentially constitutes a bottom-up, as opposed to a top-down intentionally directed change management process. At best management and the various healthcare practitioners involved can influence the culture formation process through active participation and involvement.
10. CONCLUSION
An important conclusion derived from the discussion is that the cultural attributes of a healthcare culture are deeply imbedded in an altruistic belief in the social value that emanates from the professional activities of healthcare professionals (Walshe & Smith 2011:6). It is a culture manifested in a traditional paper-based healthcare record system.
Attempting to intentionally manage the culture transformation so as be able to implement an EHR system it would appears resembles an act in futility if the change comes into conflict with a well-entrenched, patient centred, ethically based healthcare culture. Many of the failures cited in the literature, in regard to the implementation of EHR systems, could probably stem from cultural dissidence encountered in implementing the system. The ECM system as deployed at the Khayelitsha hospital would seem to be a step in the right direction, as it allows for the retention of ingrained cultural attributes of patient centred healthcare practice, while enabling the emergence of a new technology attributes that will enhance the services delivered to patients. It is suggested that in implementing a national EHR system, as part of the NHI initiative, very pertinent thought needs to be given as to the transformation of a well-entrenched paper-based culture in many public sector healthcare facilities.
REFERENCES
ANDERSON D & ANDERSON LA. 2010. Beyond change management: How to achieve breakthrough results through conscious change leadership. San Francisco: Pfeiffer. [ Links ]
ARIFFIN NAN, YUNUS AM & EMBI ZC. 2008. Improving electronic medical records (EMRs) practices through a clinical microsystem in the Malaysian government hospitals. Communications of the IBIMA 5(8):50-64. [ Links ]
BENNET A & BENNET D. 2004. Organizational survival in the new world: The intelligent complex adaptive system. Amsterdam: KMCI. [ Links ]
BOONSTRA A & BROEKHUIS M. 2010. Barriers to the acceptance of electronic medical records by physicians from systematic review to taxonomy and interventions BMC Health Services Research. [http://www.biomedcentral.com/content/pdf/1472-6963-10-231.pdf; downloaded on 2012-12-19] [ Links ]
BUCHAN I. 2011. Informatics for healthcare systems. In WALSHE K & SMITH J. (eds.) Healthcare Management, 2nd edition. New York: McGraw-Hill. pp.321-336. [ Links ]
BRYSON J. 2008. Dominant, emergent, and residual culture: The dynamics of organizational change. Journal of Organizational Change Management, 21 (6):743-757. [ Links ]
COLLEGE OF PHYSICIANS AND SURGEONS OF ALBERTA. 2004. Transition to electronic medical records. [http://www.cpsa.ab.ca/Libraries/Res_advice_to_the_profession/transition_to_electronic_medical_records_EMRs.pdf; downloaded on 2013-01-12] [ Links ]
CHANG PH. 2011. Modelling the management of electronic health records in healthcare information systems. Paper presented at IEEE Computer Society international conference on cyber-enabled distributive computing and knowledge discovery. October 2011. Beijing, China. [ Links ]
CROSNICK M. 2012. Change management is crucial for successful EHR implementations. [http://healthworkscollective.com/michael-crosnick/33555/change-management-crucial-successful-ehr-implementations; downloaded on 2012-12-29] [ Links ]
DATACENTRIX. 2012. Khayelitsha hospital creates and maintains electronic patient records. Infocentrix 2012(1):8-9 [ Links ]
DICKS T. 2012. Insights gained from the successful implementation of the ECM system deployed at the Khayelitsha hospital. (Verbal communication with researcher; notes made during the interview are in possession of the researcher.) (Ms. Dicks is the National Strategic Manager: ECM, public sector for Datacentrix and was extensively involved in the development and successful role out of the project at the hospital. [ Links ])
DORRINGTON C. 2012. Insights gained from the successful implementation of the ECM system deployed at the Khayelitsha hospital. (Verbal communication with researcher; notes made during the interview are in possession of the researcher.) (Mr Dorrington is the ECM, project manager at Datacentrix and was responsible for the management of the ECM project at the hospital. [ Links ])
FARD HD, ROSTAMY AAA & TAGHILOO H. 2009. How types of organisational cultures contribute in shaping learning organisations. Singapore Management Review 31 (1):49-61. [ Links ]
GARRETT P & SEIDMAN J. 2011. EMR vs EHR - What is the difference? [http://www.healthit.gov/buzz-blog/electronic-health-and-medical-records/emr-vs-ehr-difference/; downloaded on 2012-12-15] [ Links ]
GARTEE R. 2011. Electronic health records: understanding and using computerized medical records. 2nd edition. Boston: Pearson. [ Links ]
GELMON SB & DROPPERS O. 2008. Community health centers and electronic health records: Issues, challenges and opportunities. Portland, Oregon. [http://nwhf.org/images/files/Electronic_Medical_Record_Handbook.pdf; downloaded on 2012-11-4]. [ Links ]
GEBAUER H. & FLEISCH E. 2007. An investigation of the relationship between behavioral processes, motivation, investments in the service business and service revenue. Industrial Marketing Management 36(3):337 - 348. [ Links ]
HARRISON MI., KOPPEL R. & BAR-LEV S. 2007. Unintended consequences of information technologies in health care: An interactive sociotechnical analysis. Journal of the American Medical Informatics Association 14(5):542-549. [ Links ]
HARTLEY CP. 2010. Managing your practice's transition from paper to EHR. [http://www.physiciansehr.org/docs/The-Path-from-Paper-to-EHR.pdf; downloaded on 2012-12-10] [ Links ]
HERSH WR. 1995. The electronic medical record: Promises and problems. Journal of the American Society for Information Science 46(1):772-776. [ Links ]
ILIE V, COURTNEY JF & VAN SLYKE C. 2007. Paper versus electronic: challenges associated with physicians' usage of electronic medical Records. IEEE Proceedings of the 40th Hawaii International Conference on System Sciences. [ Links ]
JIN J, AHN G, HU H, COVINGTON MJ & ZHANG X. 2011. Patient-centric authorization framework for electronic healthcare services. Computers & Security 30(2/3): 116-127. [ Links ]
KORIWCHAK M. 2010. Physicians vs. health IT: The EMR culture war. [http://thewiredpractice.blogspot.com/2010/09/physicians-vs-health-it-emr-culture-war.html; downloaded on 2012-12-17] [ Links ]
L/ERUM H, KARLSEN TH & FAXVAAG A. 2004 Use of and attitudes to a hospital information system by medical secretaries, nurses and physicians deprived of the paper-based medical record: A case report. Bio-Medical Central Medical Informatics and Decision Making, 4(18):1-10. [ Links ]
MARCUS DD, LUBRANO J & MURRAY J. 2009. Electronic medical record implementation guide: The link to a better future, 2nd edition. The Physicians Foundation. [http://tenstarhealth.typepad.com/EMR%20Implementation%20Guide.pdf; downloaded on 2012-12-19] [ Links ]
MARS M & SEEBREGTS C. Undated. Country case study for e-health South Africa. [http://ehealth-connection.org/files/resources/County%20Case%20Study%20for%20eHealth%20South%20Africa.pdf; downloaded on 2012-12-16] [ Links ]
MCCARTHY C & EASTMAN D. 2010. Change management strategies for an effective EMR implementation. Chicago: HIMSS. [ Links ]
MCGINN CA, GRENIER S, DUPLANTIE J, SHAW N, SICOTTE C, MATHIEU L, LEDUC Y, F LÉGARÉ F & GAGNON M. 2011. Comparison of user groups' perspectives of barriers and facilitators to implementing electronic health records: a systematic review. [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3103434/; downloaded on 2012-12-17] [ Links ]
MINTZBERG H. 1994. The rise and fall of strategic planning: reconceiving roles for planning, plans, planners. Toronto: FP. [ Links ]
MUNCK B. 2002. Changing a culture of face time. In Harvard Business Review on culture and change. Boston: Harvard, p21-36. [ Links ]
MUNIR SK & KAY S. 2003. Organisational culture matters for system integration in health care. AMIA 2003 Symposium proceedings. [ Links ]
NATIONAL DEPARTMENT OF HEALTH. 2012. E-health strategy South Africa 2012-2016. [http://www.doh.gov.za/docs/stratdocs/2012/eHealth_Strategy_South_Africa_2012-2016.pdf; downloaded on 2012-12-14] [ Links ]
SALEEM JJ, RUSS AL, JUSTICE CF, HAGG H, EBRIGHT PR, WOODBRIDGE PA & DOEBBELING BN. 2009. Exploring the persistence of paper with the electronic health record. International Journal Of Medical Informatics 78(9): 618-628. [ Links ]
SEEL R. 2000. Culture and complexity: new insights on organisational change. Organisations & People 7(2):2-9. [http://www.new-paradigm.co.uk/culture-complex.htm, downloaded on 14-11-2011] [ Links ]
SNOWDEN D. 2005. Being efficient does not always mean being effective: A new perspective on cultural issues in organisations. [http://www.cynefin.net; downloaded on 2007-8-6] [ Links ]
SPRATT AD & DICKSON KE. 2008. Change factors affecting the transition to an EMR system in a private physician's practice: An exploratory study. Proceedings of the Academy of Health Care Management 5(2):21-25. [ Links ]
THE MITRE CORPORATION. 2006. Electronic health records overview. [http://www.himss.org/content/files/Code%20180%20MITRE%20Key%20Components%20of%20an%20EHR.pdf; downloaded on 15 December 2012] [ Links ]
TOSTI DT. 2007. Aligning the strategy and culture for success. Performance Improvement 46(1):21-25. [ Links ]
WALSHE K & SMITH J. 2011. Introduction: The current and future challenges of healthcare management. In WALSHE K & SMITH J. editors. Healthcare management. 2nd edition. New York: McGraw-Hill, pp1-10. [ Links ]
WEEKS J & GALUNIC C. 2003. A theory of the cultural evolution of the firm: The intra-organizational ecology of memes. Organization Studies 24(8):1309-1352. [ Links ]
WILLIAMS F & BOREN SA. 2008. The role of the electronic medical record (EMR) in care delivery development in developing countries: A systematic review. Informatics in Primary Care 16:139-45. [ Links ]
XUE Y, LIANG H, WU X, GONG H, LI B & ZHANG Y. 2012. Effects of electronic medical record in a Chinese hospital: A time series study. International Journal Of Medical Informatics 81 (10):683-689. [ Links ]
ZANDIEH SO, YOON-FLANNERY K, KUPERMAN GJ, LANGSAM DJ, HYMAN D & KAUSHAL R. 2008. Challenges to EHR implementation in electronic- versus paper-based office practices. Journal of General Internal Medicine 23:755-761. [ Links ]














