Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
Journal of Contemporary Management
versão On-line ISSN 1815-7440
JCMAN vol.9 no.1 Meyerton 2012
RESEARCH ARTICLES
Healthcare services management: a systems perspective
RV Weeks
University of Pretoria
ABSTRACT
The implementation of the National Health Insurance (NHI) is one of the government's strategic priorities. From a services management perspective it is suggested that the project necessitates a fundamental review, analysis and in some instances adaptation of key healthcare delivery and support systems to realise the strategic objective of providing patients with quality care and cost effective health services. It is envisaged that the project will be implemented over a 14 year period and cost over R300 billion. It would seem that the project will feature as one of the most ambitious, costly, complex, and multidisciplinary systems re-engineering projects ever undertaken by the Department of Health (DOH). The dysfunctionality of healthcare service delivery and the underpinning support systems appear to be generally acknowledged and the question posed is one of what needs to now be done to address the situation from a systems management perspective. The question posed is explored by means of a multi-disciplinary, contemporary literature study in order to gain an understanding of the management issues involved. Healthcare informatics, critical skill sets and organisational culture emerge as essential factors of transformation management that need to be taken into consideration.
Key phrases: healthcare informatics, healthcare services, National Health Insurance, service systems.
1. BACKGROUND
"South Africa is besieged with a quadruple burden of diseases. The burden becomes overwhelming if one has to look at it holistically and taking inefficiencies and challenging factors that are worsening the situation like the unavailability of proper health care systems or at least dysfunctional plethora of health systems in the country." - Department of Health 2011a:3
The South African Deputy Minister of Health, Dr Ramokgopa, in his introductory statement to the South African e-Health strategy makes specific reference to the problem of dysfunctional health systems and the consequential unavailability of a proper functional national healthcare system (Department of Health 2011a:3). The adverse systemic and operational challenges associated with the South African health systems are also attested to by the National Consultative Health Forum (2011:3). The National Health Insurance (NHI) project launched by the South African Government is a strategic initiative directed at addressing the inherent systemic challenges involved, in order to ensure that all South Africans have access to appropriate, efficient and quality health services.
The NHI policy paper confirms that the project is aimed at providing universal "improved access to quality health services for all South Africans irrespective of whether they are employed or not" (Department of Health 2011 b:18). The World Health Organisation (WHO) defines universal coverage as "the progressive development of a health system including its financing mechanisms into one that ensures that everyone has access to quality, needed health services and where everyone is accorded protection from financial hardships linked to accessing these health services" (Department of Health 2011b:18). The systems and services connotation attributed to healthcare in the definition assumes distinct relevance in the context of this paper.
The enormity and complexity of the systemic transformation could be inferred from the estimated cost associated with the NHI roll-out. Bateman (2010:792) cites Dr Olive Shisana, the chairperson of the NHI Ministerial Advisory Task Team, as contending that the incremental roll-out will escalate from an initial R128 billion in 2012 to R375 billion by 2025. In effect envisaged is a radical total transformation of healthcare and its supportive systems at a national, provincial and district level, with an associated transformation of the healthcare financing model (Department of Health 2011b:27). The extent of the transformation can also be appraised by the fact that there are 52 health care districts with an estimated 4200 healthcare facilities (Bateman 2011:859). In order to manage such an extensive transformation a well-articulated plan has been developed with phased implementation at both the national and sub-national levels (Department of Health 2011b:27).
The transformation is planned to occur in three phases over 14 years and entails a transition from current fragmented and often non-interactive systems to an integrated holistic healthcare and support services system infrastructure (Department of Health 2011b:44-51). A central tenet of the initial phase, starting in 2012, is the focus on conducting an assessment of existing system infrastructure, which includes inter-alia facilities, technology and management capacity, as well as the formulation of "a plan to improve its capacity and effectiveness to support health services delivery and provision within the National Health Insurance" (Department of Health 2011b:45).
In the predicting discussion the emphasis has been on the public health sector. It can be expected that the impact on the private healthcare sector, of the implementation of the NHI strategy, will be very wide-ranging and in a sense could fundamentally change the healthcare and business models of many of the healthcare networks concerned. An understanding of the systems adopted and their management, within the private healthcare sector, could serve to inform appropriate practice in managing the public sector systems transformation. Lessons learnt from international experience in the implementation of NHI systems could also be of significant value. With a multi-disciplinary, contemporary literature study serving as basis, the ensuing discussion will focus on gaining a healthcare service systems management perspective of the NHI transformation, with specific reference to the governance, technology, human resources, and cultural implications thereof. Where relevant private sector and international lessons learnt will be taken into consideration.
2. A HEALTHCARE SERVICES SYSTEMS PERSPECTIVE OF THE NHI INTITIATIVE
"To successfully implement a healthcare financing mechanism that covers the whole population such as NHI, four key interventions need to happen simultaneously: i) a complete transformation of healthcare service provision and delivery; ii) the total overhaul of the entire healthcare system iii) the radical change of administration and management iv) the provision of a comprehensive package of care underpinned by a re-engineered Primary Health Care". - Department of Health, 2011b:5
As may be inferred from the introductory statement a generic conceptualisation of what constitutes a healthcare system is assumed. Also not specifically stated, but implied is that the administration and management systems form an inherent component of the healthcare system. At the core of a healthcare services system is the provision of both services and products to patients, the latter constituting medication and similar manufactured items for monitoring and managing patient treatment. In the introductory quotation this is referred to as a "comprehensive package of care" (Department of Health 2011b:5).
Ideally the healthcare system needs to provide patients with an integrated, holistic and affordable health care solution that will meet their specific needs. Two specific value chains from a client/patient perspective emerge and assume relevance namely that of services and products, this is diagrammatically depicted in Figure 1. Also reflected in the diagram are the systems that support value creation within the services and product value chains.
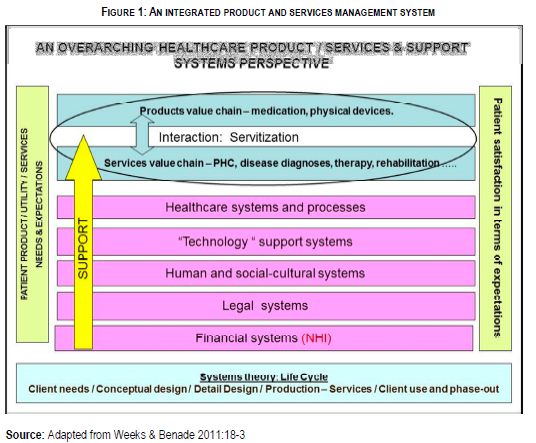
Baines, Lightfoot, Benedettini & Kay (2007:1545) describe product-service systems as an integrated system to deliver user functionality in a way that reduces the environmental impact. At an operational level the integration of services and product value streams, as well as their inherent characteristic differences need to be taken into consideration, as they have definite process and management implications. Non-ownership, intangibility, and perishability characteristic of services are alluded to by Fitzsimmons and Fitzsimmons (2010:20-21) as attributes differentiating services from products. An important distinguishing characteristic of the services component is the role played by the patient in the service delivery process (Fitzsimmons & Fitzsimmons 2010:18; Fließ & Kleinaltenkamp 2004:392).
The intangible nature of healthcare services will in particular complicate healthcare service delivery as "services" cannot be inventoried or stored, as would be the case with products such as the medication required by patients. Services, simultaneous production and consumption within a healthcare setting, undoubtedly adds to the complexity of service systems management (Desmet, Van Looy & Van Dierdonck 2003:12,19; Wilson, Zeithaml, Bitner & Gremler 2008:15-16).
Reflected in Figure 1 are human resources featuring as an important element of consideration in designing, implementing and managing an integrated healthcare system. Appropriately trained and well experienced healthcare professionals of all categories are in short supply (Department of Health 2011c:12) and improving human resources planning, development, and management systems forms one of the key points on the health sector's 10 Point Plan for 2009-2014 (Department of Health 2010:7,20). It needs to be noted that ICT skills are also in short supply and need to be taken into consideration. This aspect will be dealt with in greater detail in an ensuing discussion section within this paper.
The extent and importance of technology as a business critical domain of healthcare support is diagrammatically reflected in Figure 2. It provides support at a business systems level for governance, medical and training systems.
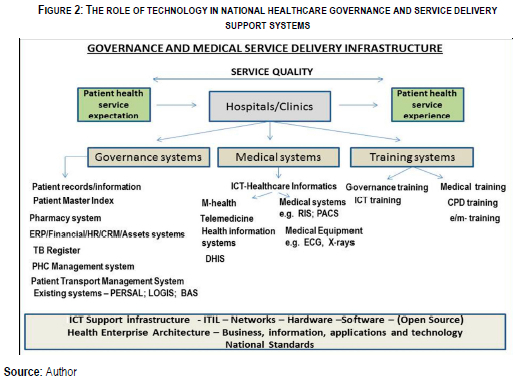
The WHO defines eHealth as the use of information and communication technologies for health (Department of Health 2011a:5), a definition that for all practical purposes is relatively wide in scope. Within the literature a number of terms are used in relation to technology based support systems within the healthcare industry, namely healthcare informatics, telemedicine, m-health (mobile), e-health (electronic) and ICT-health (information and communication technology) systems (Bateman 2011b:368; Department of Health 2011a:5; Mars & Jack 2010:55; WHO 2011:6). In many instances the descriptions and definitions attributed to the concepts are very similar in nature or have nuance differences that are of a more specific descriptive orientation. The common denominator in most of the descriptions, however, relates to their service support role.
3. GOVERNANCE SYSTEMS
A patient entering the doors of a public sector hospital or clinic does so with a service expectation, yet media reports present a very dismal reality of the service delivery that takes place within public sector medical facilities. Bailey, Maphumulo and Govender (2012:1) describe the situation as one where "hospitals are under siege as doctors, nurses and patients battle with broken equipment, shortages of linen, medicine and food, flooded theatres and no telephone lines". Add to this a critical shortage of healthcare professionals (Department of Health 2011c:12), utterly exhausted doctors, nurses and medical interns (Health24 2011:1) and the potential of a patient's healthcare service expectation being realised appears to be rather bleak. The patient's total healthcare experience in relation to his or her prior expectation will define the quality of the healthcare experience from the patient's perspective.
From a healthcare management standpoint the concept of governance is complex and multifaceted and, as noted by Som (2004:87), the concept has developed many organisational interpretations that are reflected in a proliferation of definitions and models. The researcher claims that a closer analysis of the definitions reveals that none of them capture the essence of an integrated system for effective healthcare service delivery and in practice governance systems implementation has engendered a sense of confusion as to the systems integration processes and structures (Som 2004:87).
The WHO (2008:2) acknowledges that "governance in health is a cross-cutting theme", as could to be expected to be the case in managing any contemporary organisation. The health sector would from a governance perspective, however, introduce nuance differences in terms of healthcare management specialised systems, such as electronic health records (EHR), telemedicine, mobile health systems, and the electronic TB register to cite a few such systems (Department of Health 2011a:2,28). Common to most healthcare governance conceptualisation is the notion of an integrated systems approach that, as iterated by Som (2004:88), "incorporates the overall patient experience including co-ordination of diagnosis, treatment and restoration taking into account the overall environment".
Implied in effect is a macro systems perspective that necessitates taking into consideration the vast network of systems and their interaction to ensure effective service delivery to patients, a view consistent with the management system as reflected in Figure 1. Edwards (2006:2-3) attest to the fact that most developed nations have integrated patient administrative systems with well-structured national standards for electronic data interchange. At a more micro level the individual system design testing implementation and management aspects come into consideration (Edwards 2006:3).
An important consideration of healthcare governance is the issue of national standards. Lourens (2012:3) describes the purpose thereof as the establishment of a benchmark for quality care and a framework for national accreditation of healthcare facilities. The standards are structured in seven cross-cutting domains, namely patient rights; patient safety; clinical governance and care; public health; leadership and corporate governance; operational management; and facilities and infrastructure (Lourens 2012:3). The first three represent the core business of the health system, delivering quality healthcare. The remaining domains serve as support systems for delivery.
The researcher argues that these core standards call for evidence-based practice or current appropriate practice integrating individual clinical expertise with best available external evidence from systemic research (Lourens 2012:3). The Department of Health (2011d:8) identifies seven pertinent support services that from a governance perspective assume relevance, namely: pharmaceutical, diagnostic, therapeutic and support; health technology; sterilisation, mortuary and clinical efficiency management services. Technology in this sense tends to assume a relatively wide ranging array of systems. Management of hospitals and clinics are expected to bring these healthcare services and support systems in line with the national standards. The implementation of the NHI will undoubtedly bring standards into the picture when considering governance systems.
The picture that emerges is one of governance bringing together interdependent and interacting systemic networks that collectively enable healthcare professionals and administrators to render quality services to patients entering the doors of clinics and hospitals. Quality in this sense relates to the extent to which healthcare facilities meet clients' needs and expectations, which are in line with predetermined standards (Whittaker, Shaw, Spieker & Linegar 2011:60). The element of standards assumes relevance as clients' expectations can also be unrealistic and unaffordable within a NHI dispensation. Standards thus define the required systemic functions, activities, process and structures so that various healthcare facilities across provincial and district boundaries, as well as departments within the respective facilities, can interactively provide quality services (Whittaker et al. 2011:60).
Primary Healthcare (PHC) from a systems perspective extends beyond the doors of healthcare facilities. Bezuidenhout (2008:1) argues that the healthcare system forms part of a larger community social system. This is undoubtedly true when it comes to PHC. The health care system is an open system, strongly influenced by the environment in which it functions and issues such as poverty, lack of resources and information will undoubtedly influence PHC, resulting in the need for curative as opposed to preventative systems. New forms of governance infrastructures and systems are deemed imperative to address the issue (Bezuidenhout 2008:1-5). A case in point being the need to prevent raw sewer water flowing from treatment plants into dams and rivers and thereby engendering a health risk to communities. Clean water and sustainable energy resources are also required by communities and healthcare facilities thereby extending the governance boundaries associated with PHC.
Iluyemi and Croucher (2006:91) asserted that PHC is informed by four philosophical parameters, one of which constitute appropriate technologies, which they describe as equipment, medications, procedures and techniques that are used to promote health, health-related behaviours and the functioning of health care systems. The researchers then articulate the role of e-health systems as appropriate technology in PHC with specific reference to its promises to increase efficiency in healthcare, improving quality of healthcare, the ability of empowering patients to take responsibility for their own health, and improving access to health care information and healthcare services (Iluyemi and Croucher 2006:91-93).
The key theme running through this discussion is that of ICT as an enabling mechanism to assist individuals and communities to gain access to healthcare information and services. Typical e-health technologies, from a governance perspective, that come to mind are integrated regional and national health information networks that would feature under the banner of e-health informatics. In the ensuing section the specifics of e-health technologies will be analysed in greater detail.
4. E-HEALTH TECHNOLOGY SUPPORT SYSTEMS
"Everybody talks about e-health these days, but few people have come up with a clear definition of this comparatively new term. Barely in use before 1999, this term now seems to serve as a general "buzzword," used to characterize not only 'Internet medicine', but also virtually everything related to computers and medicine." - Eysenbach (2001 :e20)
The provision of a comprehensive seamless healthcare service ranging from prevention (PHC), diagnosis and treatment to long-term care, necessitates a health service delivery system consisting of interrelated value chains of individual health service providers with a supporting e-health systems infrastructure (Stroetmann, Artmann, Stroetmann, Protti, Dumortier, Giests, Walossek & Whitehouse 2011 xii). The introductory statement by Eysenbach (2001:1) attests to a wide ranging interpretation and conceptualisation of what has become termed to be e-health technologies. Eysenbach (2001 :e20) goes on to define the term and concept as follows:
"e-health is an emerging field in the intersection of medical informatics, public health and business, referring to health services and information delivered or enhanced through the Internet and related technologies. In a broader sense, the term characterises not only a technical development, but also a state-of-mind, a way of thinking, an attitude, and a commitment for networked, global thinking, to improve health care locally, regionally, and worldwide by using information and communication technology".
The definition introduces a human or people determinant in defining what could be deemed to be a broader conceptualisation of "e-health technologies". The reference to technology brings into question three important determinants, namely context (in this sense healthcare), systems and people. The three determinants are diagrammatically depicted in Figure 3. Burgelman, Christensen and Wheelwright (2009:2) in defining technology as "the theoretical and practical knowledge, skills, and artefacts that can be used to develop products and services, as well as their productive and delivery systems" clearly attribute a human connotation to the concept. Khalil (2000:1) defines "technology" as "all the knowledge, products, processes, tools, methods and systems employed in the creation of goods or in providing services".
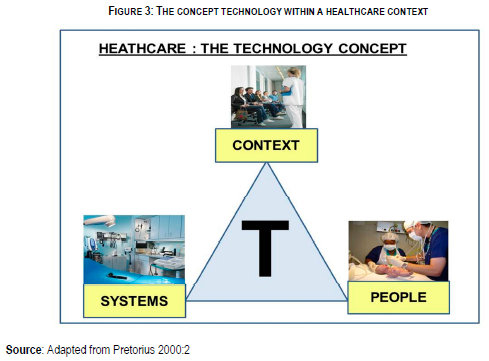
Within a healthcare services context technology therefore in terms of this latter definition assumes a very wide ranging conceptualisation of "healthcare systems". In defining technology as the mechanism through which humankind has leveraged its efforts, both individually and collectively, to improve peoples' quality of life, Harrison and Samson (In Weeks & Benade 2010:3) introduce the notion of technology with an ultimate purpose of improving peoples' quality of life, an aspect that has strong resonance within a healthcare context.
Pretorius (2000:2) brings together most of the preceding conceptualisations of Healthcare technologies by highlighting three key determinants of the concept, namely: knowledge, people and tools, and systems. It is suggested that the latter may be generically captured by the term artefacts. Skills then assume a people or human attribute in the application of artefacts or tools and systems (Weeks & Benade 2010:3). The human and skills aspect of healthcare technologies will from a systems perspective and will be addressed in more detail in the latter section of this paper. In terms of this paper it is contended that knowledge and skills development, from a technological perspective, are critical aspects that need to be considered in establishing a healthcare technology management support system and is deemed an essential element of the NHI initiative.
Stroetmann, in the preface to the European Commission (2007:7) report on e-health priorities and strategies in European countries, defines e-heath more specifically as the beneficial application of ICT-enabled solutions to health and healthcare. The definition embodied within an ICT context is, however, quite wide ranging. Mars and Scott (2010:239) in a very similar sense define e-heath as "information and communication technology that facilitates health and healthcare". In so defining the concept Mars and Scott (2010:239) add that it "provides an example of this new-found freedom to function in a borderless or interjurisdictional environment", an aspect previously addressed in discussing national standards as a governance consideration.
The WHO (2005) adopts a similar stance in defining the concept as "the cost-effective and secure use of information and communication technologies in support of health and health-related fields, including health-care services, health surveillance, health literature, and health education". Of relevance in this latter definition is the accent placed ICT technologies as a support system for healthcare services and education, both aspects reflected in Figure 2.
The context of e-health technology as seen from the preceding discussion embodies governance aspects, such as electronic medical records, pharmacy systems and healthcare informatics; electronic healthcare services, telemedicine, m-health, and digital imaging; and electronic training of healthcare professionals as well as administrative staff. These contextual domains and the components thereof are largely encapsulated with the South African e-health draft strategy document where it is suggested that the concept includes (Department of Health 2011a:5):
• Electronic Health Records (enabling sharing of patient data between points of care),
• Routine health management information,
• Vital Registration (registration of births and deaths),
• Consumer Health Informatics (access to information on health by healthy individuals or patients),
• Health Knowledge Management (best practice guidelines managed and accessed electronically),
• M-Health (use of mobile devices such as cell-phones to share information or to collect aggregate or patient data),
• Telemedicine (use of Information and Communication Technologies (ICTs) to provide physical or psychological care at a distance),
• Virtual Healthcare (teams of professionals working together via ICTs), and
• Medical Research (use of high performance computing to handle large volumes of data).
Seen within the context of the services model presented in Figure 1, Stroetmann et al. (2011:3) present a model depicting the health services value system, which they describe as health promotion, diagnosis therapy, rehabilitation and long-term care. Underpinning this value system are appropriate ICT systems (Stroetmann et al. 2011:3). Their description tends to resonate with the medical systems reflected in Figure 2. The researchers list EMR, e-prescriptions, telehealth and electronic identifiers as key technologies underpinning the healthcare services rendered to the community.
The researchers further claim that an important objective is to achieve a seamless exchange of health information across boundaries, which in the context of the European Union, is the various state borders concerned (Stroetmann et al. 2011:vii). The means of which to attain this objective is what the researchers describe as telehealth or more descriptively "health information networks link(ing) hospitals, laboratories, pharmacies, primary care and social centres" (Stroetmann et al. 2011:viii). It is acknowledged by Stroetmann et al. (2011:vii) that the wider use of such systems with the European Union is still the exception.
The convergence of healthcare information systems and EMR is gaining ground, yet Ratha (2012:1) notes that current generations of EMR have no fields for genetic data. The researcher further argues that in future personalised medicine will necessitate increased networking across systems and this would seem to imply a need for reviewing the ICT architectures from an interoperability perspective so as to avoid a duplication of very large patient data bases (Ratha 2012:1). The aspect of core national standards previously alluded to in this paper will therefore, from a management of the networks and systems concerned, assume increasing importance in the future.
Within a South African healthcare context the interoperability of systems and ICT support systems has also been addressed by the Department of Health (2012) in a needs assessment of provincial profiles. It would appear from the report that a large number of factors at a district level within the various provinces, such as different versions of the district health information system in operation, significant numbers of computers not functional for periods of time, limited computer hard-drive and memory capacity, and similar aspects act as a constraint in ensuring an effective healthcare information operational systems. Loveday, Smith and Monticelli (2006:31) in a similar sense draw attention to the fact that 50% of provincial HIS staff do not have Internet and 39% no Intranet accessibility. The implementation and management of the NHI program will necessitate an extensive review and where relevant upgrading and renewal of ICT infrastructure to effectively support healthcare services delivery.
5. E-HEALTH AND TELEMEDICINE
Al-Shorbaji (2003:13) defines telemedicine as the "use of information technology to deliver medical services and information from one location to another" and includes medical care delivery, consultation, diagnoses and treatment, as well as education of the patient and staff. In a similar sense Steyn (2010:Internet) describes telemedicine as the use of any technology that can provide medical diagnoses or patient care over a vast distance. These are definitions that resonate with the service science healthcare perspective presented in Figure 2.
The deployment of telemedicine to address the shortage of healthcare professionals could be achieved by means of what Dr Eshwari (2012) terms to be "teleConsultation" rooms situated at more remote district hospitals and clinics The purpose of the facility is one of linking healthcare professionals from diverse disciples in conducting examinations of patients where the diagnoses is of a complex and difficult nature or where the local healthcare professional requires a second opinion. Such a facility negates the need to transfer patients for referrals to a regional or more specialised hospital facility, saving both time and cost of transportation. Suggested by Dr Eswari (2012) is the need for clinic, regional, district and video conferencing e-health packages that will facilitate healthcare professional interaction in providing patients with medical services remotely. These same facilities can be used for continuous education programmes of healthcare workers.
Mars (2010:75) acknowledges that despite the obvious advantages of telemedicine its uptake has been relatively slow and limited in extent as a result of restricted capacity development in the field concerned. Steyn (2010:Internet) similarly notes that it is difficult to get busy doctors at a rural hospital to link up with busy doctors at a tertiary hospital especially if the setup is time-consuming. The use of telemedicine in clinical practice requires some training and capacity development of the practitioners involved and it is here where e-education has a very definite role to play (Mars, 2010:76). There already are too few doctors to train doctors in specialities and sub-specialities and e-health is seen as a possible solution through distance education, telemedicine, and computerised health information systems, but currently there are far too few practitioners trained in e-health (Mars 2011:32).
The successful implementation of the NHI initiative will necessitate the need for the optimal use of scarce resources and healthcare professions are most probably at the top of this list. This would seem to suggest that from a healthcare management perspective telemedicine systems have the potential to enhance healthcare services delivery to communities in rural districts.
6. THE PEOPLE COMPONENT OF HEALTHCARE TECHNOLOGY MANAGEMENT
"When we understand culture as the meaning giving system of a society then it becomes a current ever evolving force which can best be experienced in active engagement with today's human beings as well as with local nature, not with yesterday's historical beings". - Lessem and Schieffer, 2009:118
Attested to in the introductory quotation is the emergent nature of an institution or societal culture as a living system that is responsive to a forever changing and complex contextual setting, which in this case would be that of healthcare facilities. Managing the implementation of E-Health technologies will of necessity entail an evolutionary process of culture realignment. As alluded to in the preceding discussion it is this people element of the e-health technological change management process that will be most challenging to deal with.
Munck (2002:23) suggests that transforming an organisation's culture in effect constitutes one of the most fundamental, challenges confronting an institution, as people's natural inclination is to hold on to whatever feels familiar, even if confronted with better alternatives. Nowhere is this contention more important than in the case of healthcare professions who have become accustomed to well established practices of medicine and healthcare management. The introduction of EMR, telemedicine or similar systems will of necessity entail a change in the way things are done and thus in the culture of the healthcare facility concerned.
The traditional management view is one of being able to actively and intentionally manage the concept to realise a desired or envisioned culture. It would seem that many practitioners have bought into the idea that culture can be intentionally managed and as noted by Trompenaars and Prud'Homme (2004:34) institutions have as a consequence spent significant financial resources on consultants brought in to assist them to "roll-out" a new desired culture. It would seem that management practitioners have bought into the idea that culture can be managed and, as noted by Trompenaars and Prud'Homme (2004:34), institutions have as a consequence spent significant financial resources on consultants brought in to assist them to "roll-out" a new desired culture.
This would seem to be contradicted by a more contemporary complexity theory approach in dealing with the concept, where it is suggested that it is a naturally evolving "living system" and the outcome of the culture formation process can therefore not be predicted with any degree of certainty (Bate 1994:136; Bennet & Bennet 2004:150). McCormick (2008:78) tends to substantiate this view in claiming that "culture for the most part develops in an evolutionary unmanaged process".
These essentially conflicting divergent views are of great significance for those who will be involved in formulating and implementing the change management process associated with the e-health strategy as part of the NHI project. In practice the more traditional view of intentional culture change management is tending to make way for the emergent perspective as the latter is found to more accurately reflect the actual process that takes place (Weeks, 2010:44). Trompenaars and Prud'Homme (2004:34) suggests that if one where to understand culture as a meaning giving system of society, then it becomes a current and forever evolving force, which can best be experienced in active engagement.
Bennet and Bennet (2004:150) very pertinently assert that culture emerges out of the nonlinear interactions that takes place among individuals and cannot be traced back to a single cause or individual. The researchers stress that emergence is not random, but rather the result of multiple interactions that settle down to internal coherence and patterns. Snowden (2002:4) in this regard confirms that if cultural interventions are seen as pattern revealing and influencing activities, institutions will have a far greater degree of success in dealing therewith.
A complex adaptive perspective of culture change within an e-health management context would suggest that getting healthcare practitioner buy-in would be essential. Mars (Undated:Internet) confirms that getting such buy-in is in fact critical for the successful implementation of telemedicine technologies. The research further claims that "incentives should be offered for already overworked staff to use telemedicine, which is seen as an additional and time-consuming burden" and that "there should be a local telemedicine champion to drive the changes" (Mars, undated:Internet). All these statements resonate with a complex adaptive systems view of culture transformation, namely that as a living system it evolves as people come to accept or buy-in to new values, beliefs, norms and ways of doing things.
At best the change agents involved (telemedicine champions) can therefore actively live out their belief in the advantages to be derived from the use of the technology concerned. As the real life experiences in utilising the systems unfold, so new values, beliefs and norms will come into being that will support the adoption of the new technology. It is a view that Bennet and Bennet (2004:150) would certainly endorse, as may be determined from their observation of culture as an emergent phenomenon, namely as "workers go about their daily business of communicating, solving problems, taking action, and reacting to information from others". It is further argued by Bennet and Bennet (2004:150) that before an institution can adopt new practices to significantly change the way it conducts its activities, such as would be the case in implementing e-health technologies, it must be willing to admit that current practices are inadequate, which in essence requires a change in mind set. It is a statement that resonates with Munck's (2002:29,30) assertion that people need to truly want the change in the first place.
7. CONCLUSION
The literature study reveals that e-health technology systems are likely to form an ever increasing dimension in bringing into being the new NHI dispensation. The strategic changes involved require not only very significant systemic changes, but also a culture change. Traditional management thinking and practice that stem from the scientific era of management tend to suggest that a healthcare facilities' culture can be intentionally managed so as to ensure a more appropriate strategy - culture alignment. The reality, however, would appear to be rather different if a more contemporary complex adaptive systems perspective is adopted in dealing with the culture transformation management.
Culture change then is deemed to be an emergent process, one that at best can be influenced through active engagement and involvement of healthcare practitioners in living out the desired values and beliefs and not merely by mission, vision and values statements reflecting a need for culture change.
References
AL-SHORBAJI N. 2001. Health and medical informatics. Technical paper. Cairo, Egypt: World Health Organization. [ Links ]
BAILEY C, MAPHUMULO S & GOVENDER P. 2012. Public hospitals in Gauteng sick and tired. [http://www.timeslive.co.za/sundaytimes/2012/03/25/public-h; downloaded on 2012-03-14] [ Links ]
BAINES TS, LIGHTFOOT HW, BENEDETTINI O & KAY JM. 2009. The servitization of manufacturing: A review of literature and reflection on future challenges. Journal of Manufacturing Technology Management, 20(5):547-567. [ Links ]
BATE P. 1994. Strategies for cultural change. Oxford: Butterworth-Heinemann. [ Links ]
BATEMAN C. 2010. NHI consensus: Fix the existing system or risk failure. South African Medical Journal, 100(12):791-793. [ Links ]
BATEMAN C. 2011a. Wing and prayer days over for SA's healthcare system. South African Medical Journal, 101(12):859-861. [ Links ]
BATEMAN C. 2011b. Cutting-edge telemedicine venture freezes as official bodies frown. South African Medical Journal, 101(6):368-372. [ Links ]
BENNET A & BENNET D. 2004. Organizational survival in the new world: The intelligent complex adaptive system. Amsterdam: KMCI. [ Links ]
BEZUIDENHOUT MC. 2008. External factors influencing healthcare services management. In Booyens C (Ed.) Introduction to healthcare services management. Cape Town :Juta: 1-20. [ Links ]
BURGELMAN RA, CHRISTENSEN CM & WHEELWRIGHT SC. 2009. Strategic management of technology and innovation. 5th edition. New York: McGraw-Hill. [ Links ]
DEPARTMENT OF HEALTH. 2010. National Department of Health Strategic Plan 2010/11-2012/13. [http://hs.ukzn.ac.za/Libraries/Post-graduate_Administrative_Procedure/NDOH_STRATEGIC_PLAN_201011-201213_01_MARCH_2010_1_1.sflb.ashx ; downloaded on 2012-04-14] [ Links ]
DEPARTMENT OF HEALTH. 2011a. eHealth Draft Strategy 2010-2014 South Africa. Pretoria: National Department of Health. [ Links ]
DEPARTMENT OF HEALTH. 2011b. National Health Insurance in South Africa: Policy Paper. [https://www.pps.co.za/portal/Ditaba/NHI%20green%20paper.pdf; downloaded on 2012-03-14] [ Links ]
DEPARTMENT OF HEALTH. 2011c. Human resources for healthy South Africa: HRH strategy for the health sector: 2012/13-2016/17. [http://www.doh.gov.za/docs/stratdocs/2011/hrh_strategy.pdf; downloaded on 2012-03-14] [ Links ]
DEPARTMENT OF HEALTH. 2011d. National core standards for health establishments in South Africa. Pretoria: National Department of Health. [http://www.sarrahsouthafrica.org/LinkClick.aspx?fileticket=YnbSHfR8S6Q%3D&tabid=2327; downloaded on 2012-04-5] [ Links ]
DEPARTMENT OF HEALTH. 2012. District Health Information System: Rapid information needs assessment provincial profiles. Pretoria: National Department of Health. [ Links ]
DESMET S, VAN LOOY B & VAN DIERDONCK R. 2003. The nature of services. In Van Looy B., Gemmel P & Van Dierdonck R. (Eds.). Services management: an integrated approach. London : Prentice Hall. pp. 1 -26. [ Links ]
EDWARDS J. 2006. Case Study: Denmark's achievements with healthcare information exchange. Gartner: Industrial Research. [http://www-03.ibm.com/industries/ca/en/healthcare/files/gartner-case_study-denmarks_achievementswHIE.pdf; downloaded on 2012-04-5] [ Links ]
ESHWARI RR. 2012. E-health systems. Verbal interview conducted with Dr Eshwari, Manager e-health and information technology, Department of Health, Kwazulu-Natal. [ Links ]
EUROPEAN COMMISSION. 2007. e-Health priorities and strategies in European countries. Luxemburg: European Communities. [http://ec.europa.eu/information_society/activities/health/docs/policy/ehealth-era-full-report.pdf; downloaded on 2012-04-12] [ Links ]
EYSENBACH G. 2001. What is e-health? Journal of Medical Internet Research, 3(2):e20. [ Links ]
FLIEß S & KLEINALTENKAMP M. 2004. Blueprinting the service company: Managing service processes efficiently. Journal of Business Research, 57(4):392-404. [ Links ]
FITZSIMMONS JA & FITZSIMMONS MJ. 2010. Service Management: Operations, Strategy, Information Technology, 7th edition. London: McGraw-Hill. [ Links ]
HEALTH24. 2011. Sinking ship for SA interns. [http://www.health24.com/printarticle.htm; downloaded on 2012-03-29. [ Links ]]
ILUYEMI A & CROUCHER RE. 2006. E-Health as an appropriate technology in primary health care. IET Digest, 2006(11370):89-95. [ Links ]
KHALIL T. 2000. Management of technology: The key to competitiveness and wealth creation. Boston: McGraw-Hill. [ Links ]
LESSEM R & SCHIEFFER A. 2009. Transformation management: Towards the integral enterprise. Burlington: Gower. [ Links ]
LOURENS G. 2012. The national core standards and evidence-based nursing. Professional Nursing Today, 16(1):3-4. [ Links ]
LOVEDAY M, SMITH J & MONTICELLI F. 2006. Healthcare information audit report South Africa. [http://www.hst.org.za/sites/default/files/NatHIS_audit.pdf; downloaded 2012-04-12] [ Links ]
MARS M. Undated. Telemedicine in South Africa. [http://web.idrc.ca/en/ev-137471-201-1-DO_TOPIC.html; downloaded on 2012-04-30] [ Links ]
MARS M. 2010. Health capacity development through telemedicine in Africa. IMIA Yearbook of Medical Informatics, pp75-81. [ Links ]
MARS M. 2011. Building the capacity to build capacity in e-health in sub-Saharan Africa: The KwaZulu-Natal experience. Telemedicine and e-Health, 18(1):32-36. [ Links ]
MARS M & JACK C. 2010. Why is Telemedicine a challenge to the regulators? South African Journal of Bioethics and Law, 3(2):55-58. [ Links ]
MARS M & SCOTT RE. 2010. Global e-health policy: A work in progress. Health Affairs, 29(2):239-245. [ Links ]
MCCORMICK BA. 2008. What's responsible for business success or failure? Its... the organization's culture. Amherst: HRD. [ Links ]
MUNCK B. 2002. Changing a culture of face time. In Harvard Business Review on culture and change. Boston: Harvard, p21-36. [ Links ]
NATIONAL CONSULTATIVE HEALTH FORUM 2011. National Health Insurance Conference: Lessons for South Africa. Conference on National Health Insurance: Lessons for South Africa, Department of Health, Tshwane, South Africa. [ Links ]
PRETORIUS MW. 2000 Technology assessment in the manufacturing enterprise: a holistic approach. Proceedings of the 9th International Conference on Management of Technology, 21-25 February, Miami, Florida, USA. [ Links ]
RATHA D. 2012. The game changer: Informatics researchers study how to get genetic information to the point of care. Healthcare Informatics, [http://www.healthcare-informatics.com/article/game-changer-0#node-15691; downloaded on 2012-4-14] [ Links ]
SNOWDEN D. 2002. Being efficient does not always mean being effective: A new perspective on cultural issues in organisations. [http://www.cognitive-edge.org/; downloaded on 2010-03-05] [ Links ]
SOM CV. 2004. Clinical governance: a fresh look at its definition. Clinical Governance, 9(2):87-90. [ Links ]
STEYN L. 2010. Telemedicine wonderful, in theory. [http://mg.co.za/article/2010-09-27-telemedicine-wonderful-in-theory; downloaded on 19 April 2012) [ Links ]
STROETMANN KA, ARTMANN J, STROETMANN VN, PROTTI D, DUMORTIER J, GIESTS S, WALOSSEK U & WHITEHOUSE D. 2011. European countries on their journey towards national eHealth infrastructures: Final European progress report. European Commission, Brussels, Belgium. [ Links ]
TROMPENAARS F & PRUD'HOMME P. 2004. Managing change across corporate cultures. Chichester: Capstone. [ Links ]
WEEKS RV. 2010. Organisational culture: A contemporary management perspective. Acta Commercii, 10:43-58. [ Links ]
WEEKS RV & BENADE SJ. 2010. Technological and management skills development: a foundation for economic growth in developing countries. Paper presented at the IAMOT International Conference on Management of Technology, 7-11 March, Cairo, Egypt. [ Links ]
WEEKS RV & BENADE SJ. 2011. Service science: A servitization systems perspective. Paper presented at ISEM international conference on Industrial Engineering, System Engineering and Engineering Management for Sustainable Global Development, Spier, Stellenbosch, South Africa, 21-23 September. [ Links ]
WHITTAKER S, SHAW C, SPIEKER N & LINEGAR A. 2011. Quality standards for healthcare establishments in South Africa. [http://www.sarrahsouthafrica.org/LinkClick.aspx?fileticket=YnbSHfR8S6Q%3D&tabid=2327; downloaded on 2011-4-12] [ Links ]
WILSON A, ZEITHAML AV, BITNER MJ & GREMLER DD. 2008. Services marketing: Integrated customer focus across the firm. Maidenhead: McGraw-Hill. [ Links ]
WORLD HEALTH ORGANISATION. 2005. World Health Assembly concludes: Adopts key resolutions affecting global public health. [http://www.who.int/mediacentre/news/releases/2005/pr_wha06/en/; downloaded on 2012-04-14] [ Links ]
WORLD HEALTH ORGANISATION. 2008. Health systems governance. [http://www.who.int/healthinfo/statistics/toolkit_hss/EN_PDF_Toolkit_HSS_Governance.pdf; downloaded on 2012-5-3] [ Links ]
WORLD HEALTH ORGANISATION. 2011. M-Health: New horizons for health through mobile technologies. World Health Organization, Geneva Switzerland. [ Links ]














