Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.23 n.1 Centurion 2024
http://dx.doi.org/10.17159/2309-8309/2024/v23n1a6
TRAUMA AND GENERAL ORTHOPAEDICS
Measurement of functional acetabular column sizes using a 3D CT model, for guiding percutaneous screw fixation of acetabular fractures using fluoroscopy
Sven StrydomI, ; Ryan BooyseI; Anith ChackoII; Philip MostertIII; Christian H SnyckersI
IEugene Marais Hospital, Pretoria, South Africa
IIRadhiant Diagnostic Imaging SA, East London, South Africa
IIIWilgeheuwel Hospital, Roodepoort, South Africa
ABSTRACT
BACKGROUND: Percutaneous acetabular screw fixation remains a technically challenging procedure, despite good outcomes being reported with appropriate patient selection. In the developing world, where intraoperative computer tomography (CT) guidance (O-arm) and dedicated screws are not readily available, this procedure becomes even more challenging, as surgeons often place screws under fluoroscopic guidance only. Additionally, incorrect screw sizing can lead to cortical breaching with catastrophic vascular damage and other serious consequences. This study aimed to demonstrate how surgeons working with intraoperative fluoroscopy can use preoperative three-dimensional (3D) reconstructed CT scans to plan and safely insert screws into these 'functional fluoroscopic corridors', and to compare column sizes for screw selection in the South African population to existing literature.
METHODS: A retrospective study using data obtained from CT scans of adult patients was performed. Three-dimensional reconstructions of the pelvis were used to create a novel technique of simulating the 'functional' bone corridors used during fluoroscopic surgery in order to take the measurements of the anterior and posterior acetabular columns in 301 patients (163 male and 138 female). Exclusion criteria were: any previous trauma and fractures of the pelvis, congenital abnormalities and tumours involving the bony pelvis. We also demonstrate the use of this technique in a clinical case.
RESULTS: Our study confirmed that column sizes in the South African population are in keeping with previous publications. We demonstrate how this novel preoperative 3D-CT planning technique can be used to identify intraoperative surgical corridors using fluoroscopy.
CONCLUSION: Although column sizes in the South African population are shown to be in keeping with international literature, our study demonstrates a novel technique for using 3D CT reconstructions preoperatively, in the same orientation used intraoperatively with fluoroscopy, to help guide screw size choice and placement. This technique shows promise for reducing cortical breaches in settings where intraoperative O-arms are not available, as appropriately sized screws can be preselected on an individualised basis.
Level of evidence: Level 3
Keywords: acetabular fractures, percutaneous fixation, acetabular columns, acetabular column sizes, 3D CT reconstruction
Introduction
Percutaneous screw fixation of acetabular fractures was described in 19981 and has since gained popularity due its minimally invasive nature and good outcomes.2 Unfortunately, this technique is not without potential complications, most of which are caused by cortical breaching that damages surrounding neurovascular and other vital structures.3 This led to the development of intraoperative computer tomography (CT) guidance with O-arms to improve the accuracy of screw placement and improve outcomes when compared to traditional fluoroscopic screening.4,5 These advanced imaging systems are not readily available in developing countries, such as South Africa, which may explain why this surgical technique does not share the same popularity as in America and Eurasia.
Comparisons of American and Chinese populations vary widely with regard to screw size, with additional significant differences between male and female populations.6,7 Complicating the process are the varying recommendations that have been made regarding the safe diameter of screws to be used in the fixation.7-11 Dedicated instrumentation is not currently available in South Africa and logistics and costs involved in pre-ordering and obtaining the correct screws from abroad leaves little room for error. Incorrect sizing can potentially lead to cortical breach when traversing the osseous columns, which can then lead to catastrophic vascular damage.3 Therefore, the correct selection of a screw with a safe diameter is vital for patient safety. Adequate intraoperative radiological guidance is also necessary to ensure correct screw trajectory.1,3
The purpose of our study was to determine accurate 'functional' measurements of the lengths and widths of the anterior and posterior columns of the acetabulum and thereby guide selection of appropriate lengths of screws for external percutaneous fixation of the pelvis. This technique can be applied in settings where intraoperative CT guidance is not available to help guide screw placement by using the same views on intraoperative fluoroscopy as on the preoperative three-dimensional (3D) CT reconstructions.
Methods and materials
A retrospective study using data obtained from sequential CT scans of adult patients was used. Three-dimensional volume reconstructions of the pelvis were used to take the various measurements of the anterior and posterior acetabular columns.
Adult patients, 20 years and older, undergoing pelvis CT scans for non-orthopaedic indications were sequentially selected. Patients with previous fractures of the lumbar spine or pelvis, congenital abnormalities, tumours of the bony pelvis or other lesions involving the bony pelvis were excluded.
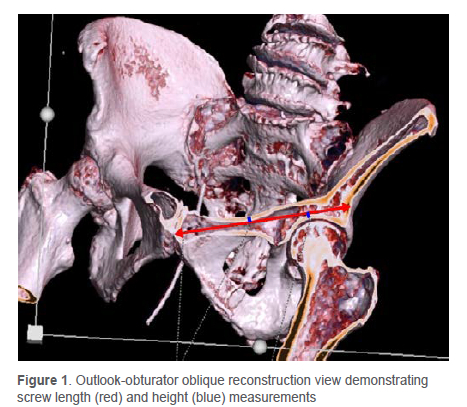
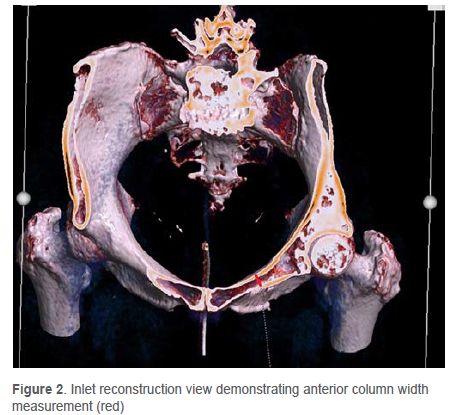
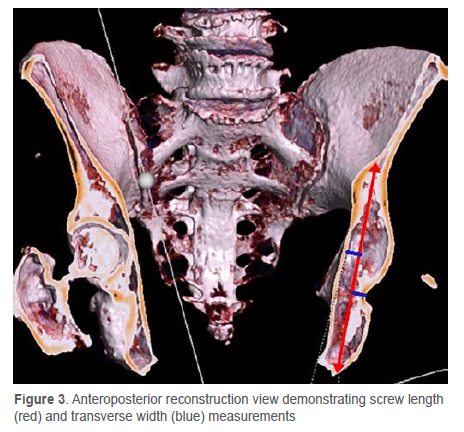
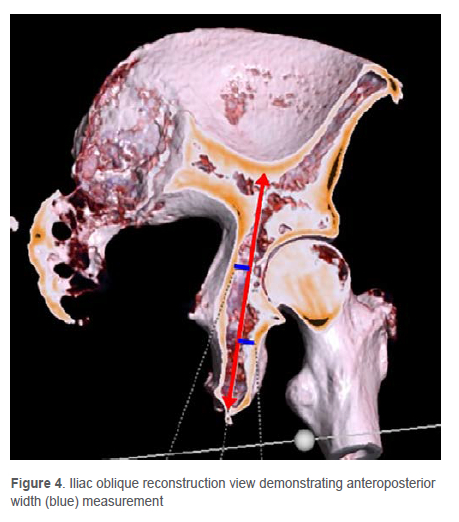
Three-dimensional volume reconstruction of the surface anatomy of the bony pelvis was performed. The images were then turned to simulate the fluoroscopic views used during surgery (Figures 1 to 4). Once the images were aligned to the correct fluoroscopic view, the bone was virtually cut to reveal the available 'functional' bone corridor. Since the screw trajectory does not always pass through the centre of the column, the perpendicular distance from the predicted screw trajectory to the cortex is used in some of the views, as will be described below.
For the anterior column views, the beam is rotated approximately 30° to 45° until the view is from inferiorly looking upwards at the pelvic outlet. Next the view is rotated roughly 30° to the affected side so that the anterior column is seen in profile, the outlook-obturator oblique view (Figure 1). A virtual cut is made into the pelvis to divide the anterior column in half, with the pubic symphysis and half of the acetabulum still showing. A line is drawn from the entry point at the pubis past the acetabulum until the opposite pelvic cortex. The entry point is then marked. Measurements of anterior column length and height were then performed as follows:
• Length: measured from the entry point to the posterior acetabular margin, on the obturator oblique view; this correlates with the intended screw trajectory
• Height: measured as the narrowest point from the cortex, either at the mid-acetabular roof or medial wall of the superior pubic ramus, to the screw trajectory line; this corresponds to screw radius and should thus be doubled to get screw diameter
The pelvis is then rotated until the pelvic inlet view from superior is seen and a new virtual cut is made to divide the anterior column in half again at the level of the entry point (Figure 2). During screw placement, although some adjustment of the entry point can occur, the screw must pass central at this point of the pubic rami, as this is the most restricted section of the column.
• Width: the anterior column width is measured at the narrowest point of the pubic ramus on the pelvic inlet view; this corresponds to screw diameter
For the posterior column, an anteroposterior reconstruction is used which represents a standard AP pelvis view. A virtual cut in the coronal plane through the posterior column is made (Figure 3) and the following measurements taken:
• Length: measured from the intended entry point at the most inferior aspect of the ischial tuberosity to the sciatic notch; this corresponds to the intended screw trajectory
• Transverse width: measured as the narrowest point from the cortex to the screw trajectory line; this corresponds to screw radius and should thus be doubled to get screw diameter
Lastly the iliac oblique view is performed by rotating the 3D reconstruction approximately 45° away from the affected side until the pelvis shows the posterior column with a sagittal cut, at the level of the entry point. A virtual cut is made dividing the posterior column in half to show the anteroposterior width (Figure 4).
• Anteroposterior width: measurement is taken from the nearest cortex to the screw trajectory line and must thus be doubled for the functional screw diameter in the posterior columns
For standardisation purposes, all measurements were done by a single qualified radiologist. Collected data was collated in a spreadsheet, with each CT scan assigned a study number for anonymity. Means and standard deviations were determined for the column measurements.
Results
A sample size of 301 patients was obtained with 163 (54%) males and 138 (46%) females. This was expected to yield a power of greater than 95%. The measurements of the anterior and posterior columns vary as expected. Sex differences are marked, with male pelvis measurements being larger than female pelvis measurements.
Table I shows the average age for males and females as well as the means and standard deviations for each measurement in both sexes. The overall sample size was calculated to give a power of greater than 95%.
The narrowest portion of the anterior column in both sexes was the height from the projected screw trajectory to the superior cortex in the oblique sagittal plane (Figure 1). This measurement was used to calculate the diameter and recorded as the height of the anterior column; the narrowest portion of the posterior column was recorded as the diameter calculated from the transverse width from the projected screw trajectory to the medial cortex of the ischium (Figure 3).
There were several CT scans having pelvic and acetabular measurements that fell outside the expected averages. These outliers were statistically excluded but bear clinical significance, as these would be difficult cases for percutaneous pelvic screw fixation. This novel CT measurement technique provides a simple method to identify these patients and is easy to perform.
In Figure 5 we demonstrate the postoperative pelvic radiograph of the patient whose preoperative CT scans (Figures 1 to 4) were first measured and found to be favourable for percutaneous fixation.

Discussion
Characterisation of acetabular fractures can be difficult because of the complex acetabular anatomy and the many possible fracture patterns.12 Accurate classification of acetabular fractures is important for determining the proper surgical treatment.13 Because of the complex acetabular anatomy, various classifications have been suggested, but the Judet-Letournel classification system remains the most widely accepted.14-17 The addition of CT with multi-planar reconstruction and 3D surface rendering is helpful in understanding and classifying acetabular fractures and their management.16,18,19
The objective of surgery for acetabular fractures is to reconstruct the joint congruency, fixate the bone fragments, prevent further fracture displacement and allow rapid mobilisation and rehabilitation.20
Percutaneous fixation of fractures involving the anterior and posterior acetabular columns, although still a relatively new concept in South Africa, has been described previously.1,9 Percutaneous fixation of the sacroiliac joint has long been considered the gold standard of treatment for posterior element instability of the pelvis and is well-established treatment.3,21,22 Currently the fixation of unstable fractures of the acetabulum with percutaneous screws introduced through small incisions is gaining popularity.6,8 These procedures are less invasive as compared to open fixation and are more beneficial in terms of early mobilisation, especially for the elderly.3
The major advantage is the immediate stability obtained which leads to early full weight-bearing. Additional advantages over open procedures are the decreased operative morbidity, blood loss and time to perform the procedure. Wound healing, infection and blood loss are all complications that are more attributable to open procedures rather than the actual fractures.3,20
Where fractures are amenable and/or patients have contraindications for major procedures, percutaneous procedures should ideally be used. Giannoudis et al. found in the early results of many studies that patients had a shorter hospital stay and decreased morbidity when treated with percutaneous techniques.3
Anatomical reduction of the fractures with a gap of 2 mm or less is found to be a favourable prognostic indicator of good joint function and reduced risk of post-traumatic osteoarthritis. The percutaneous technique is, however, more technically challenging than open reduction and fixation due to acetabular geometry.20 The technique is recommended with the use of cannulated intramedullary screws to treat non-displaced to slightly displaced fractures, especially in the elderly who cannot receive total joint arthroplasty, and in osteoporotic and/or obese patients.20
This study demonstrates how preoperative CT scans can be used to determine 'functional' bone corridors to help guide fluoroscopic screw choice and placement. In addition, it attempts to generate an average measurement of the male and female pelvis and specifically the anterior and posterior columns prevalent in the local population (Table I). In keeping with available literature, there is significant difference between male and female measurements.23,24 Also, to be expected, there were a number of outliers with significant variability to the mean. These outliers bear clinical significance, as these would be difficult cases for percutaneous pelvic screw fixation using fluoroscopy.
It was found that the narrowest measurement of the pelvis in both sexes was the anterior column height within the middle of the pubic ramus (Figure 1). This is in keeping with intraoperative experiences at our institution as well as in findings of previous image-guided and cadaveric studies.6,7,20,25,26 This is the region of greatest concern for potential breaches into the superior cortex, thus such extra care should be taken when approaching the mid-acetabular roof in the anterior column where breach is either into the femoral head or the neurovascular femoral bundle superiorly. Likewise, for the posterior column, the area of concern is the medial cortex of the ischium.27
It is also found clinically that, due to the narrower female pelvic diameter and high carrying angle of certain female pelvises, it may not be possible to pass a percutaneous screw though the entire length of a fracture. This is especially of importance in the anterior columns where the fracture site may need to be bridged with two screws: one retrograde from the pubis and one anterograde via the iliac wing in order to prevent cortical breach of the screws where the risk of vascular injury is high (Figure 6a). The other possibility is the use of minimally invasive subcutaneous anterior pelvic fixation techniques, such as the Bridging Infix described by Strydom and Snyckers28 to stabilise the fracture site (Figure 6b). Use of this CT measurement technique can aid greatly in identifying these outlier patients and avoid screw breaching intraoperatively.22
There is sparse literature to help guide the selection of appropriate screw lengths in the South African population. Also limiting the widespread rollout of this procedure is the lack of hybrid theatres with intraoperative O-arms, as is utilised in United States and other countries.5,22,29 The purpose of our study was to provide accurate average measurements of the anterior and posterior columns and hence determine appropriate lengths and diameters of screws for percutaneous fixation of the pelvis using a novel technique that is readily available. Pre-selection of appropriately sized screws is essential for a technically successful fixation and safe outcome. Smaller screw sizes are vital to ensure safety due to the lack of O-arms, where only fluoroscopic guidance in two planes is available, and will prevent devastating cortical breaches.30 We also demonstrate how CT film cuts, based on the required described fluoroscopic views,1,29 can be used to better plan for this surgical technique. This can help guide surgeons in resource-limited countries like South Africa.
Cutting through the columns in the plane of the screw trajectory avoids any misrepresentation of measurements by only using the surface anatomy, and minimises errors of measurement due to natural curvature of bone elements of the anterior and posterior columns. These views also represent the intraoperative fluoroscopic views that are used to guide screw placement. This process can be repeated on any CT scan machine with a program capable of performing 3D reconstructions; hence it is a novel technique that is readily available in most settings where pelvic column fractures are diagnosed to give the functional diameter of the pelvic columns. Intraoperatively, the surgeon then uses the same views with fluoroscopy to guide screw placement according to the template they now have from pre-planning the operation. This saves time and ensures the correct diameter screws are placed at roughly the correct angles to avoid cortical breach.
Potential limitations of our study are that measurements were only done by a single author and the technique described to obtain the measurements has not yet been validated.
Conclusion
Our study shows that screws with diameters of 6.5 mm (males) and 5.0 mm (females) would be deemed safe for most pelvic anterior columns.
Additionally, we demonstrate the need for even tighter control of screw sizes than previously thought, particularly in the anterior columns of females. In the posterior columns, screws with an even larger diameter would be safe to use for percutaneous fixation of acetabular fractures when using functional measurements using fluoroscopic guidance. Hence the commercially available 6.5 mm screws will provide acceptable reductions without breach in most female posterior columns, whereas in males the 7.3 mm or even occasionally 8.0 mm screw will pass for the posterior column.
Although intraoperative CT guidance can aid in safe screw passage, surgeons have been using fluoroscopic views to guide screw fixation as intraoperative CT guidance is not widely available in our setting. This technique demonstrates how reconstructed 3D CT views can be used to preoperatively determine appropriate trajectory, entry point, screw diameter and length, combined with the same views intraoperatively to guide screw fixation. It will also help to identify 'outlier' patients in which no safe 'functional corridor' can be attained with the standard views. The use of intraoperative O-arm CT scans remains a more precise technique; however, we would argue that in countries that do not have intraoperative CT, this hybrid technique is far safer than traditional fluoroscopy alone.
Future research can aim to validate this technique for preoperative screw selection and planning.
Ethics statement
The authors declare that this submission is in accordance with the principles laid down by the Responsible Research Publication Position Statements as developed at the 2nd World Conference on Research Integrity in Singapore, 2010.
Prior to commencement of the study, ethical approval was obtained from the University of Pretoria Faculty of Health Sciences Research Ethics Committee (ref: 187/2012). All procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Formal written consent was obtained for the use of patient radiographs, and is available on request.
Declaration
The authors declare authorship of this article and that they have followed sound scientific research practice. This research is original and does not transgress plagiarism policies.
Author contributions
SS: data analysis and manuscript revision
RB: data analysis and manuscript revision
AC: data capture, analysis and first draft preparation
PM: data analysis and first draft preparation
CHS: study conceptualisation, data analysis, first draft preparation and manuscript revision
ORCID
Strydom S https://orcid.org/0000-0002-6288-4388
Booyse R https://orcid.org/0000-0003-4576-033X
Chacko A https://orcid.org/0000-0002-1036-2959
Snyckers CH https://orcid.org/0000-0002-6297-894X
References
1. Starr AJ, Reinert CM, Jones AL. Percutaneous fixation of the columns of the acetabulum: a new technique. J Orthop Trauma. 1998;12(1):51-58. https://dx.doi.org/10.1097/00005131-199801000-00009 [ Links ]
2. Chacko A, Mostert P, Snyckers C, Ismail F. Measurement of acetabular column sizes for guiding percutaneous fixation of acetabular fractures in the South African population. ERC 2013. C-0758. https://dx.doi.org/10.1594/ecr2013/C-0758 [ Links ]
3. Giannoudis PV, Tzioupis CC, Pape HC, Roberts CS. Percutaneous fixation of the pelvic ring: an update. J Bone Joint Surg Br. 2007;89(2):145-54. https://dx.doi.org/10.1302/0301-620X.89B2.18551 [ Links ]
4. Ciolli G, Caviglia D, Vitiello C, et al. Navigated percutaneous screw fixation of the pelvis with O-arm 2: two years experience. Med Glas (Zenica). 2021 Feb 1;18(1):309-15. https://dx.doi.org/10.17392/1326-21 [ Links ]
5. Gay SB, Sistrom C, Wang G, et al. Percutaneous screw fixation of acetabular fractures with CT guidance: preliminary results of a new technique. AJR 1992; 158:819-22. https://dx.doi.org/10.2214/ajr.158.4.1546599 [ Links ]
6. Shahulhameed A, Roberts CS, Pomeroy CL, et al. Mapping the columns of the acetabulum-implications for percutaneous fixation. Injury. 2010;41(4):339-42. https://dx.doi.org/10.1016/j.injury.2009.08.004 [ Links ]
7. Chen KN, Wang G, Cao LG, Zhang MC. Differences of percutaneous retrograde screw fixation of anterior column acetabular fractures between male and female: a study of 164 virtual three-dimensional models. Injury. 2009;40(10):1067-72. https://dx.doi.org/10.1016/j.injury.2009.01.014 [ Links ]
8. Kazemi N, Archdeacon MT. Immediate full weightbearing after percutaneous fixation of anterior column acetabulum fractures. J Orthop Trauma. 2012;26(2):73-79. https://dx.doi.org/10.1097/BOT.0b013e318216b3e3 [ Links ]
9. Routt ML, Jr., Simonian PT, Grujic L. The retrograde medullary superior pubic ramus screw for the treatment of anterior pelvic ring disruptions: a new technique. J Orthop Trauma. 1995;9(1):35-44. https://dx.doi.org/10.1097/00005131-199502000-00006 [ Links ]
10. Parker PJ, Copeland C. Percutaneous fluoroscopic screw fixation of acetabular fractures. Injury. 1997;28(9-10):597-600. https://dx.doi.org/10.1016/s0020-1383(97)00097-1 [ Links ]
11. Grossterlinden L, Nuechtern J, Begemann PG, et al. Computer-assisted surgery and intraoperative three-dimensional imaging for screw placement in different pelvic regions. J Trauma. 2011;71(4):926-32. https://dx.doi.org/10.1097/TA.0b013e31820333dd [ Links ]
12. Goulet JA, Bray TJ. Complex acetabular fractures. Clin Orthop Relat Res. 1989(240):9-20. [ Links ]
13. Brandser E, Marsh JL. Acetabular fractures: easier classification with a systematic approach. AJR Am J Roentgenol. 1998;171(5):1217-28. https://dx.doi.org/10.2214/ajr.171.5.9798851 [ Links ]
14. Judet R, Judet J, Letournel E. Fractures of the acetabulum: classification and surgical approaches for open reduction. Preliminary report. J Bone Joint Surg Am. 1964;46:1615-46. [ Links ]
15. Harris JH, Jr., Lee JS, Coupe KJ, Trotscher T. Acetabular fractures revisited: part 1, redefinition of the Letournel anterior column. AJR Am J Roentgenol. 2004;182(6):1363-66. https://dx.doi.org/10.2214/ajr.1826.1821363 [ Links ]
16. Harris JH, Jr., Coupe KJ, Lee JS, Trotscher T. Acetabular fractures revisited: part 2, a new CT-based classification. AJR Am J Roentgenol. 2004;182(6):1367-75. https://dx.doi.org/10.2214/ajr.182.6.1821367 [ Links ]
17. Hunter JC, Brandser EA, Tran KA. Pelvic and acetabular trauma. Radiol Clin North Am. 1997;35(3):559-90 [ Links ]
18. Falchi M, Rollandi GA. CT of pelvic fractures. Eur J Radiol. 2004;50(1):96-105. https://dx.doi.org/10.1016/j.ejrad.2003.11.019 [ Links ]
19. Durkee NJ, Jacobson J, Jamadar D, et al. Classification of common acetabular fractures: radiographic and CT appearances. AJR Am J Roentgenol. 2006;187(4):915-25. https://dx.doi.org/10.2214/AJR.05.1269 [ Links ]
20. Caviglia H, Mejail A, Landro ME, Vatani N. Percutaneous fixation of acetabular fractures. EFORT Open Rev. 2018;3(5):326-34. https://dx.doi.org/10.1302/2058-524L3.170054 [ Links ]
21. Tsiridis E, Upadhyay N, Gamie Z, Giannoudis PV. Percutaneous screw fixation for sacral insufficiency fractures: a review of three cases. J Bone Joint Surg Br. 2007;89(12):1650-53. https://dx.doi.org/10.1302/0301-620X.89B12.19058 [ Links ]
22. Attias N, Lindsey RW, Starr AJ, et al. The use of a virtual three-dimensional model to evaluate the intraosseous space available for percutaneous screw fixation of acetabular fractures. J Bone Joint Surg Br. 2005;87(11):1520-23. https://dx.doi.org/10.1302/0301-620X.87B11.16614 [ Links ]
23. Dienstknecht T, Muller M, Sellei R, et al. Screw placement in percutaneous acetabular surgery: gender differences of anatomical landmarks in a cadaveric study. Int Orthop. 2013;37(4):673-79. https://dx.doi.org/10.1007/s00264-012-1740-1 [ Links ]
24. Gras F, Gottschling H, Schroder M, et al. Sex-specific differences of the infraacetabular corridor: a biomorphometric CT-based analysis on a database of 523 pelves. Clin Orthop Relat Res. 2015;473(1):361-69. https://dx.doi.org/10.1007/s11999-014-3932-z [ Links ]
25. Jacob AL, Suhm N, Kaim A, et al. Coronal acetabular fractures: the anterior approach in computed tomography-navigated minimally invasive percutaneous fixation. Cardiovasc Intervent Radiol. 2000;23(5):327-31. https://dx.doi.org/10.1007/s002700010061 [ Links ]
26. Dienstknecht T, Muller M, Sellei R, et al. Percutaneous screw placement in acetabular posterior column surgery: gender differences in implant positioning. Injury. 2014;45(4):715-20. https://dx.doi.org/10.10164.injury.2013.10.007 [ Links ]
27. Ochs BG, Stuby FM, Ateschrang A, et al. Retrograde lag screw placement in anterior acetabular column with regard to the anterior pelvic plane and midsagittal plane - virtual mapping of 260 three-dimensional hemipelvises for quantitative anatomic analysis. Injury. 2014;45(10):1590-98 [ Links ]
28. Strydom S, Snyckers CH. Minimally invasive subcutaneous anterior fixation of pelvic fractures in the elderly: case report and literature review. SA Orthop J 2021;20(4):240-45. http://dx.doi.org/10.17159/2309-8309/2021/v20n4a8 [ Links ]
29. Rommens PM, Wagner D, Hofmann A. Minimal invasive surgical treatment of fragility fractures of the pelvis. Chirurgia (Bucur). 2017 Sept-Oct;112(5):524-37. https://dx.doi.org/10.21614/chirurgia.112.5.524 [ Links ]
30. Khan JM, Lara DL, Marquez-Lara A, et al. Intraoperative CT and surgical navigation for iliosacral screws: technique for patients with sacral dysmorphism. J Orthop Trauma. 2018 Aug;32 Suppl 1:S24-S25. https://dx.doi.org/10.1097/BOT.0000000000001213 [ Links ]
Received: June 2023
Accepted: August 2023
Published: March 2024
Editor: Dr Luan Nieuwoudt, University of KwaZulu-Natal, Durban, South Africa
Funding: No funding was received for this study.
Conflict of interest: The authors declare they have no conflicts of interest that are directly or indirectly related to the research.
* Corresponding author: svenstrydom@gmail.com














