Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SA Orthopaedic Journal
versión On-line ISSN 2309-8309
versión impresa ISSN 1681-150X
SA orthop. j. vol.23 no.1 Centurion 2024
http://dx.doi.org/10.17159/2309-8309/2024/v23n1a5
ORTHOPAEDIC ONCOLOGY AND INFECTIONS
A radiological assessment of tibia shaft fractures stabilised with intramedullary nails by trainee surgeons
Alexis S Whitehead; Jurek RT Pietrzak; Jason du Plessis; Anthony Robertson
Charlotte Maxeke Johannesburg Academic Hospital, Department of Orthopaedics, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
BACKGROUND: This retrospective cohort study analysed patient files and radiographs of 158 patients who underwent tibial nail surgery between April 2016 and March 2018 at a level one trauma centre in South Africa. The aim was to evaluate the radiological adequacy of reduction of tibial fractures treated by intramedullary nailing at our institution, and to identify factors associated with poor reduction and the causes of early loss of reduction.
METHODS: Demographic and injury data were collected, and radiographs were digitally measured at two time points. The data were analysed to determine the success rate of adequate reductions and identify any factors associated with unacceptable reductions.
RESULTS: Out of 163 tibial fractures, the majority showed adequate reductions that were maintained until follow-up. Motorised vehicle accidents were the most common cause of fracture (64%), and the majority of fractures were closed injuries (60%). A malalignment rate of 32% was found overall, with the bulk of these being minor deviations of a few degrees. Fractures in the proximal third were most likely to be malaligned. However, fractures in the distal third were most likely to displace after surgery. Surgeon level of experience and time of day the surgery occurred were associated with rates of malalignment.
CONCLUSION: This study demonstrates a high rate of acceptable reduction that is in keeping with international standards. These procedures were commonly performed by trainee orthopaedic surgeons, and the results demonstrate that trainee orthopaedic surgeons can perform tibial nail surgery to an acceptable standard. Factors correlated with poor reductions were proximal third fractures requiring three proximal screws, and complex cases done during daytime hours.
Level of evidence: Level 3
Keywords: tibia fractures, alignment, trainee surgeon
Introduction
Tibial fractures are among the most common long bone fractures, and frequently occur in young, healthy patients who are of working age. There are no published epidemiological data specific to South Africa (SA), but international studies show tibial shaft fractures to be the second most frequent long bone fracture after humeral fractures and the most common long bone fracture in young adults.1 Additionally, SA has a high burden of trauma, particularly interpersonal violence and motorised vehicle accidents, which disproportionately affect young, working age men.2,3
Many orthopaedic trauma procedures are performed independently by junior registrars in SA, that would be performed by qualified specialists in more well-resourced settings.4 This is due to the high number of trauma patients presenting to state hospitals, as well as a lack of fully trained medical specialists in SA, with only 0.1 specialists per 1 000 population in the state hospital sector. Thus, registrars are rapidly trained to operate independently without direct consultant supervision.5 It is, therefore, of interest to evaluate if these procedures are being done to a technical standard in line with international norms. Many of the international authors who have published their results have included detailed information on their specific findings, allowing for comparison with our findings.4,6-9
The aim of this study was to evaluate the radiological adequacy of reductions of tibial fractures treated by tibial nailing at our institution. Furthermore, we aimed to identify factors correlated with poor reductions and identify potential causes of early loss of reduction.
Patients and methods
A retrospective record and radiograph review was performed on patients treated with intramedullary nails for tibial shaft fractures at our institution - a large level one trauma centre. Ethics approval was obtained prior to data collection, and for this study formal consent was not required. Data were collected over a two-year period, from 2016 to 2018. Digital images of the radiographs of patients who met the entry criteria were retrieved from the hospital's Picture Archiving and Communication System (PACS), and their hospital files reviewed.
All skeletally mature patients treated with intramedullary nailing of the tibia were included, provided they had adequate pre- and postoperative radiographs available on the PACS, and at least one follow-up radiograph taken at least six weeks post surgery available on the PACS. All patterns of shaft fracture were included, provided the initial treatment was with an intramedullary nail.
Patients with intra-articular fractures, patients who underwent exchange nailing after an initial treatment with a different fixation method, and those with previous fractures of the tibia that may have affected alignment were excluded.
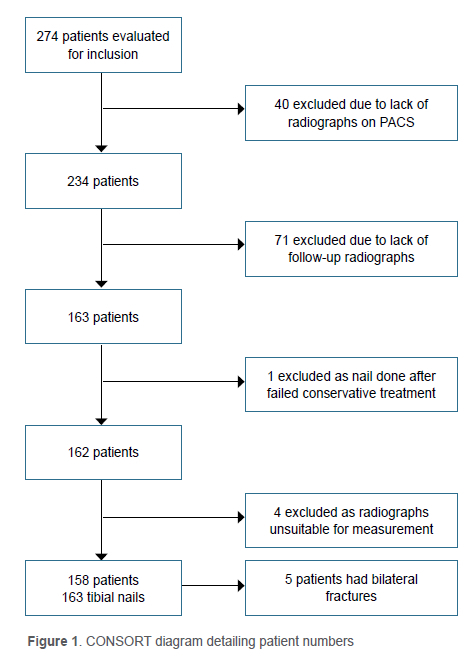
A total of 274 patients were evaluated for inclusion in the study. A significant percentage did not meet the inclusion criteria, predominantly due to inadequate radiographs available (Figure 1).
Age, sex, the mechanism of injury, as well as the Gustilo and Anderson (GA) classification of the soft tissue component of the injury were retrieved from the records. The details of the surgery were recorded, including time of day at which surgery occurred, duration of surgery and whether this was a single surgery or part of multiple surgeries performed at one sitting. Surgeon experience was categorised as either medical officer, which is a doctor who has completed a minimum of three years of practice post obtaining their medical degree, or registrar, which is a specialist trainee with more experience in orthopaedics than a medical officer. Registrars were further divided by their year of study, from first to fourth year.
The nailing system used was recorded from the notes as well as the approach used. During this time, the unit protocol was for a suprapatellar approach to be used for proximal third fractures, and an infrapatellar approach for midshaft and distal fracture patterns.
The nailing systems used were Smith+Nephew Trigen Meta-nail 129, 81% (Smith+Nephew, Watford England); Stryker T2 tibial nail 11, 7% (Stryker, MI USA); Synthes Expert Tibial Nail 2, 1% (Johnson & Johnson, NJ USA); not recorded 21, 13%.
The radiographs were then reviewed, and the fracture pattern was classified according to the Orthopaedic Trauma Association (OTA) classification.10
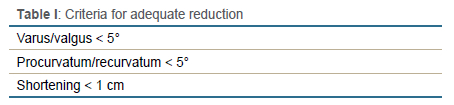
The postoperative alignment was measured using IMATRI software (imatri Medical - Johannesburg, South Africa) and the adequacy of reduction was assessed, according to the criteria in Table I.68,9,11-13 As rotation cannot be measured accurately on plain film radiographs, it was not included as a variable. These measurements were done on four radiographs, an anteroposterior and a lateral image on both the postoperative images, and follow-up images taken at least six weeks later. Shortening was measured on both views and the greatest amount of shortening was recorded. For those fractures too comminuted to measure accurately, shortening was estimated from the fibula. Unless all three of the measurable criteria were met, the reduction was deemed to be inadequate.
The data were captured using Excel 2016 (Microsoft, WA, USA) and analysed using Stata (Statacorp, TX, USA) version 15 software. Overall, patient characteristics were described using frequencies and percentages for categorical variables. Mean and standard deviation were used to describe normally distributed numeric variables, while median and interquartile range were used to describe non-normal data.
Alignment was also described using frequencies and percentages. We explored associations between loss of reduction (varus/valgus > 5° and procurvatum/recurvatum > 5°) and patient characteristics using Fisher's exact tests. A p-value of < 0.05 was considered to be statistically significant.
Results
In total we had 158 patients with 163 tibia fractures. There were 124 males (78%) and 34 females (22%). Polytrauma patients made up 48 (30%) of the cases, with the remaining 110 (70%) being isolated single tibia injuries. The age range of the patients was from 16 to 71 years of age with 128 (81%) at, or under, 40 years of age. A large number of the admissions took place over the weekend, with 22 (14%) on Fridays, 32 (20%) on Saturdays and 31 (20%) on Sundays. The four remaining weekdays accounted for 73 (46%) of the total admissions.
The most common mechanism of injury was motorised vehicle accidents (MVA) (102, n = 158; 64%), with pedestrian vehicle accidents (PVAs) accounting for 50% of injuries overall (79, n = 158), followed by car accidents (15, n = 158; 9%), and motorbike accidents (MBAs) (8, n = 158; 5%). Interpersonal violence accounted for a further 15% of fractures, including gunshot wounds (9, n = 158; 6%) and assault (15, n = 158; 9%). The remainder of the injuries were caused by falls from a height (17, n = 158; 11%), soccer injuries (12, n = 158; 8%) and a blunt object falling on the patient (2, n = 158; 1%).
The majority of fractures were closed injuries (97, 60%). Of the 66 open fractures, 25 were GA type 1 open fractures (38%), 26 were GA type 2 open fractures (39%), 14 were GA type 3A open fractures (21%), and 1 was a GA type 3B open fracture (2%). There were no GA type 3C fractures that were treated primarily with an intramedullary nail.
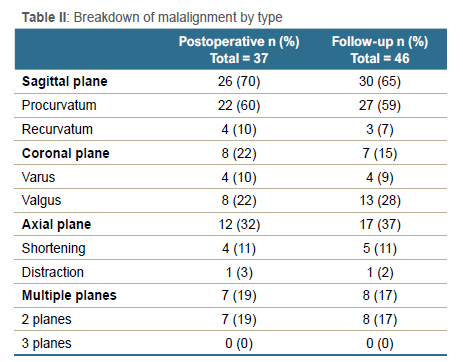
Overall, 52 (32%) patients were found to have inadequate reductions at any time point, 37 (23%) at their initial postoperative measurements and 46 (28%) at their follow-up measurements (Table II). Fractures that occurred in the proximal third were more likely to be malaligned; this was statistically significant postoperatively (p = 0.010) but not at follow-up (p = 0.862). The number of proximal screws was associated with procurvatum/ recurvatum postoperatively (p < 0.001) and at follow-up (p = 0.005), with patients who had three screws having the greatest procurvatum/recurvatum.
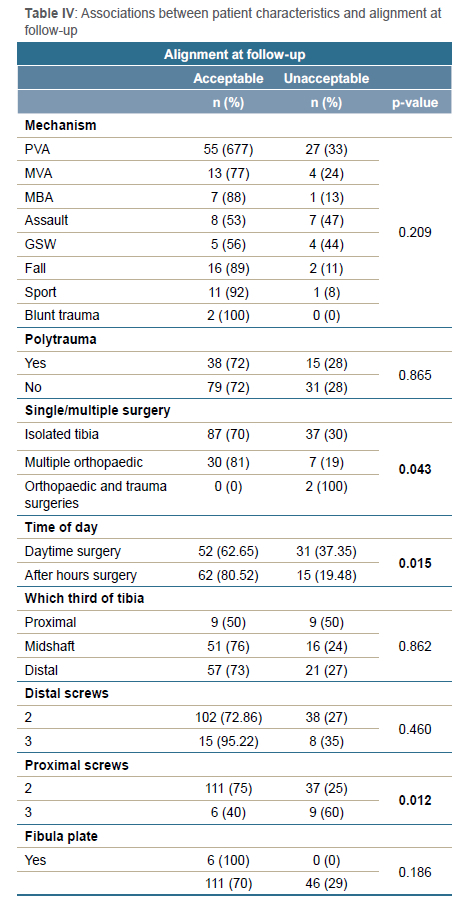
Patients who had both orthopaedic and general trauma surgeries, such as laparotomy for abdominal injuries, on the same occasion had the greatest procurvatum/recurvatum postoperatively (p = 0.029) and at follow-up (p = 0.001), and these associations were statistically significant. There was a trend towards these patients being at a higher risk of malalignment overall, but this did not reach statistical significance (p = 0.043).
Surgeon level of experience, time of day the surgery occurred, and number of proximal screws were associated with malalignment postoperatively and at follow-up (p = 0.012; p = 0.038). However, there were no statistically significant differences in mean or median degrees of malalignment between different levels of surgeon experience (Table III). Daytime surgeries had a higher rate of malalignment at both postoperative (p = 0.039) and follow-up measurements (p = 0.015). Higher numbers of proximal screws were also associated with a higher risk of malalignment postoperatively (p < 0.001) and at follow-up (p = 0.012) (Table IV). The number of patients who lost alignment between the postoperative measurement and the follow-up measurement was greatest in the distal third fractures, but this was not statistically significant (p = 0.175).
Discussion
The majority of patients in our study were young males, in keeping with other studies in the South African literature pertaining to traumatic injuries.2,3 Likewise this is similar to the international literature, as Williams et al. based in the United Kingdom (UK), Freedman et al. based in the United States of America (USA), Bhandari et al. based in Canada, and the large, multicentre, USA-based SPRINT trial all reported similar percentages.6,7,14,15 These studies also identified tibial fractures to be more common in younger patients, which is consistent with our findings.
This preponderance of young and male patients probably reflects the high levels of interpersonal violence in this group, as well as high levels of alcohol consumption and its resultant effects on high-risk behaviour.2 Likewise, the high number of admissions on weekends vs weekdays might reflect higher alcohol consumption on weekends vs weekdays. As this was a retrospective study, we were limited by the data already present in the file, and very few files had information regarding patient consumption of alcohol prior to the injury. Therefore, this was not a variable we could include in the present study, although it would be an interesting one to include in any future prospective studies on this topic.
Pedestrian vehicle accidents (PVA) were the most common mechanism of injury in our study at 50%. However, international studies report far lower levels of PVA. These differences may represent regional differences in road safety as well as pedestrian behaviour.16,17 We also found a lower rate of sports injuries and a higher rate of injuries resulting from interpersonal violence, as summarised in Table V.6,7,12,14,15
When classifying the fractures according to the OTA classification, we found that the most common fracture type in our series was a 42-A2-b, midshaft oblique, and a 42-B2-b, midshaft intact wedge. This is similar to our comparison studies with both Larsen et al. and the SPRINT trial, which reported intact wedge fractures as the most common group.4,15 Likewise, both Yoon et al. and Chan et al. reported a high number of intact wedge fractures.12,18 We believe that our findings can be compared to the abovementioned studies as we had broadly similar mechanisms of injury, and very similar groups of fracture patterns.4,6,7,12,15,18
Previous studies assessing malalignment following tibial nail insertion used lines drawn perpendicular to the joint surface to determine the axis of the bone.14 However, this approach has its drawbacks as the radiographs may not have been taken perfectly perpendicular to the joint and the tibial plateau is not perpendicular to the tibial shaft.19
Modern software tools allow for more sophisticated measurement of digital radiographs, such as IMATRI.20 IMATRI software uses circles placed in such a way that their curve is tangential to the outer cortex of the bone. The centre of the circle then falls on the centre of the bone. Joining two such centres produces a line down the central anatomical axis of the bone (Figure 2).20 This allows for accurate measurement of the angle formed between the two axes of the fragments.20 It has also been shown to have good inter- and intra-observer reliability.20 To the best of our knowledge this is the first paper to use this type of software for analysing tibial alignment.
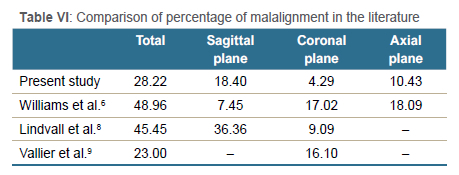
Overall, the rate of tibias that resulted in an unsatisfactory position at follow-up was 28%. This is in keeping with the literature (Table VI). There were 3% of patients with shortening at follow-up, 1% with distraction, 18% with sagittal plane malalignment, and 4% with coronal plane malalignment. Patients had malalignment in two planes in 5% of tibias, and none had malalignment in three planes.
There was no correlation between increasing surgeon experience and increasing or decreasing success in obtaining a good reduction identified. This is similar to Williams et al., Larsen et al. and Gaebler et al., who all reported no significant differences between senior surgeons and trainees in their studies.4,6,21 However, two of the mentioned studies compared qualified trauma super specialists with non-trauma specialised orthopaedic consultants, and only the dated study by Williams included registrars. Prior studies on the complications of trainees vs specialists in other orthopaedic trauma surgeries have produced mixed results, with Harris and Lin finding no difference, and Khunda et al. finding a higher risk of early mortality in cases done by unsupervised trainees.22,23
In contrast to many developed country training systems, registrars in SA are exposed to a high number of trauma cases and become skilled at performing the common trauma procedures unsupervised early in their training. Additionally, in our training system, trainee surgeons do the majority of tibial nails, with specialists handling more complex types of trauma. Thus, comparable results may not be achieved by trainees in systems where trainees do not get as much exposure to trauma or opportunity to operate independently.
The time of day when the surgery occurred was also significantly associated with malalignment, both postoperatively (p = 0.039) and at follow-up (p = 0.015). However, this relationship is opposite to what we expected, with cases done during the day having a higher risk of malalignment. A possible explanation for this phenomenon is that complicated cases that are predicted to be difficult are frequently postponed to daytime hours. This is borne out by the observation that 64% of segmental fractures, and 63% of all AO grade C fractures were operated on during the day. This finding contrasts with Larsen et al. and Williams et al., where both studies reported no difference in the accuracy of reduction for surgeries performed during the day vs those done after hours.4,6
Increasing numbers of proximal screws was also associated with a higher risk of malalignment postoperatively (p < 0.001) and at follow-up (p = 0.012). This is likely due to the fact that there was a higher rate of malalignment in proximal third fractures than in the study population as a whole (50% vs 28%), and the majority of cases (80%) in which three screws were used were segmental fractures involving the proximal third, or fractures of the proximal tibia. Thus, this finding most likely reflects the known tendency of these proximal fractures to displace into procurvatum, and the third screw being inserted to obtain greater stability in these unstable fracture patterns.24
As this was a retrospective review, we were limited by the data already documented in the files and the radiographs already taken. There was a high exclusion rate of 41% as many patients who received tibial nails during the study period did not have sufficient or adequate radiographs available on the PACS. Our institution is in an economic hub with a high number of migrant workers, many of whom return home to be cared for by their families following an injury, and who complete their care at a local hospital. However, the dropout rate was random and the patients who were included were representative of the whole group of eligible patients. We do not believe there was any correlation between dropout and clinical outcome.
Conclusion
This analysis of the adequacy of reduction of tibial fractures performed by trainee surgeons established that there was a rate of acceptable reduction that is in keeping with international standards. Most patients had reductions that were acceptable, and of the patients whose reductions were not satisfactory, the majority were minor deviations of a few degrees.
Factors correlated with poor reductions were proximal third fractures requiring three proximal screws and complex cases done during daytime hours. There was a small minority of patients who lost reduction between their initial postoperative radiographs and their follow-up radiographs. Most patients had satisfactory reductions that were maintained throughout the follow-up period.
Ethics statement
The authors declare that this submission is in accordance with the principles laid down by the Responsible Research Publication Position Statements as developed at the 2nd World Conference on Research Integrity in Singapore, 2010.
Prior to the commencement of the study ethical approval was obtained from the following ethical review board: University of the Witwatersrand Human Research Ethics Committee (Medical); Clearance number M181052.
All procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Informed written consent was not obtained from all patients for being included in the study, as it was a retrospective review.
Declaration
The authors declare authorship of this article and that they have followed sound scientific research practice. This research is original and does not transgress plagiarism policies.
Author contributions
ASW: study design, data capture, data analysis, manuscript preparation and revision
JRTP: study conceptualisation and design, data review and independent verification
JdP: data capture, manuscript revision
AR: guidance on study design and completion, manuscript revision
ORCID
Whitehead AS https://orcid.org/0000-0003-3642-8386
Pietrzak JRT https://orcid.org/0000-0001-5694-0016
Du Plessis J https://orcid.org/0000-0002-4617-9742
Robertson A https://orcid.org/0000-0003-3697-511X
References
1. Pasco JA, Lane SE, Brennan-Olsen SL, et al. The epidemiology of incident fracture from cradle to senescence. Calcif Tissue Int. 2015;97(6):568-76. [ Links ]
2. Nicol A, Knowlton LM, Schuurman N, et al. Trauma surveillance in Cape Town, South Africa: An analysis of 9236 consecutive trauma center admissions. JAMA Surg. 2014;149(6):549-56. [ Links ]
3. Hilton T, Kruger N, Wiese K, et al. Gunshot tibia fractures treated with intramedullary nailing: A single centre retrospective review. SA Orthop J. 2017;16:32-38. [ Links ]
4. Larsen P, Koelner-Augustson L, Elsoe R, et al. The long-term outcome after treatment for patients with tibial fracture treated with Intramedullary nailing Is not Influenced by time of day of surgery and surgeon experience. Eur J Trauma Emerg Surg. 2017;43(2):221-26. [ Links ]
5. Econex. Health Reform Note 7: Updated GP and specialist numbers for SA. Econex Health Reform Series [Internet]. 2010 27/10/2021. [ Links ]
6. Williams J, Gibbons M, Trundle H, et al. Complications of nailing in closed tibial fractures. J Orthop Trauma. 1995;9(6):476-81. [ Links ]
7. Bhandari M, Tornetta P, 3rd, Sprague S, et al. Predictors of reoperation following operative management of fractures of the tibial shaft. J Orthop Trauma. 2003;17(5):353-61. [ Links ]
8. Lindvall E, Sanders R, Dipasquale T, et al. Intramedullary nailing versus percutaneous locked plating of extra-articular proximal tibial fractures: comparison of 56 cases. J Orthop Trauma. 2009;23(7):485-92. [ Links ]
9. Vallier HA, Cureton BA, Patterson BM. Randomized, prospective comparison of plate versus intramedullary nail fixation for distal tibia shaft fractures. J Orthop Trauma. 2011;25(12):736-41. [ Links ]
10. Kellam JF, Meinberg EG, Agel J, et al. Introduction: Fracture and Dislocation Classification Compendium-2018: International Comprehensive Classification of Fractures and Dislocations Committee. J Orthop Trauma. 2018;32 Suppl 1:S1-S10. [ Links ]
11. Egol KA, Weisz R, Hiebert R, et al. Does fibular plating improve alignment after intramedullary nailing of distal metaphyseal tibia fractures? J Orthop Trauma. 2006;20(2):94-103. [ Links ]
12. Yoon RS, Bible J, Marcus MS, et al. Outcomes following combined intramedullary nail and plate fixation for complex tibia fractures: A multi-centre study. Injury. 2015;46(6):1097-101. [ Links ]
13. Githens M, Haller J, Agel J, Firoozabadi R. Does concurrent tibial intramedullary nailing and fibular fixation increase rates of tibial nonunion? A matched cohort study. J Orthop Trauma. 2017;31(6):316-20. [ Links ]
14. Freedman EL, Johnson EE. Radiographic analysis of tibial fracture malalignment following intramedullary nailing. Clin Orthop Relat Res. 1995(315):25-33. [ Links ]
15. Bhandari M, Guyatt G, Tornetta P, 3rd, et al. Randomized trial of reamed and unreamed intramedullary nailing of tibial shaft fractures. Study to Prospectively Evaluate Reamed Intramedullary Nails in Patients with Tibial Fractures. J Bone Joint Surg Am. 2008;90(12):2567-78. [ Links ]
16. Larsen P, Elsoe R, Hansen SH, et al. Incidence and epidemiology of tibial shaft fractures. Injury. 2015;46(4):746-50. [ Links ]
17. Phaff M, Aird J, Rollinson PD. Delayed implants sepsis in HIV-positive patients following open fractures treated with orthopaedic implants. Injury. 2015;46(4):590-94. [ Links ]
18. Chan DS, Serrano-Riera R, Griffing R, et al. Suprapatellar versus infrapatellar tibial nail insertion: a prospective randomized control pilot study. J Orthop Trauma. 2016;30(3):130-34. [ Links ]
19. Boulton C OTR. Tibia and Fibula Shaft Fractures. In: Court-Brown CM HJ, McQueen MM, Ricci WM, Tornetta P, McKee MD, editor. Rockwood and Green's Fractures in Adults. 2. Eighth ed. Philadelphia: Wolters Kluwer Health. p. 2415-68. [ Links ]
20. Dymond IW, Ashforth JA, Dymond GF, et al. The usage of image trigonometry in bone measurements. Hip Int. 2013;23(6):590-95. [ Links ]
21. Gaebler C, McQueen MM, Vecsei V, Court-Brown CM. Reamed versus minimally reamed nailing: a prospectively randomised study of 100 patients with closed fractures of the tibia. Injury. 2011;42 Suppl 4:S17-21. [ Links ]
22. Harris IA, Lin C. Orthopaedic trauma surgery performed by unsupervised and supervised trainees: complication rates compared. J Orthop Surg (Hong Kong). 2007;15(3):264-66. [ Links ]
23. Khunda A, Jafari M, Alazzawi S, et al. Mortality and re-operation rate after proximal femoral fracture surgery by trainees. J Orthop Surg (Hong Kong). 2013;21(1):87-91. [ Links ]
24. Franke J, Hohendorff B, Alt V, et al. Suprapatellar nailing of tibial fractures-Indications and technique. Injury. 2016;47(2):495-501. [ Links ]
Received: May 2023
Accepted: July 2023
Published: March 2024
Editor: Dr Luan Nieuwoudt, University of KwaZulu-Natal, Durban, South Africa
Funding: No funding was received for this study.
Conflict of interest: The authors declare they have no conflicts of interest that are directly or indirectly related to the research.
* Corresponding author: alexis.whitehead@doctors.org.uk














