Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SA Orthopaedic Journal
versión On-line ISSN 2309-8309
versión impresa ISSN 1681-150X
SA orthop. j. vol.23 no.1 Centurion 2024
http://dx.doi.org/10.17159/2309-8309/2024/v23n1a4
SPINE
Thirty-day unplanned reoperation following spinal surgery: how does the South African private sector measure up?
Marcus van HeukelumI; Theresa N MannI, II; Robert N DunnIII; Adriaan J VlokIV; Johan H DavisI, II,
IInstitute of Orthopaedics and Rheumatology, Mediclinic Winelands Orthopaedic Hospital, Stellenbosch, South Africa
IIDivision of Orthopaedic Surgery, Department of Surgical Sciences, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
IIIDivision of Orthopaedic Surgery, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa
IVDivision of Neurosurgery, Department of Surgical Sciences, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
ABSTRACT
BACKGROUND: Thirty-day readmission rate and 30-day reoperation rate are recognised indicators of perioperative quality of care. While these indicators have been reported in numerous studies from developed countries, little is known about readmission and reoperation following spinal surgery in South Africa. The main aim of this study was to describe the overall rate of 30-day reoperation and 30-day readmission following spine surgery in a large open medical scheme. Secondary aims were to describe the reasons for 30-day reoperation and 30-day reoperation by spine region and for certain procedures.
METHODS: This retrospective cohort study was based on an anonymised dataset of spine surgeries funded by the largest open medical scheme in South Africa between 2008 and 2017. The dataset was processed to identify descriptors of each surgery, including the year of operation, patient demographics, spinal pathology, spine region and certain procedures. The primary outcome was reoperation within 30 days, which was identified based on the time to the second operation, diagnostic codes and procedure codes.
RESULTS: A total of 49 395 spine surgeries were included in the study, of which at least 38 218 (77%) were for degenerative pathology. Overall, 3 204 (6.5%) surgeries were associated with 30-day readmission for any cause and 415 (0.8%) patients underwent a second unplanned spine surgery within 30 days of the initial spine procedure. The most common reasons for the 415 reoperations were neural compression (n = 160, 39%) and infection (n = 79, 19%).
CONCLUSION: Spine surgery in the South African private sector is associated with low rates of 30-day readmission and reoperation, suggesting good quality of perioperative care. Furthermore, the findings compare favourably with those from developed countries. Future studies should investigate long-term reoperation following spinal surgery to provide more comprehensive insight into the quality of spinal surgery care in the South African private healthcare setting.
Level of evidence: Level 3
Keywords: spinal surgery, reoperation, readmission, private sector, South Africa
Introduction
Spine surgery has seen rapid advancement due to novel technological innovations, safety improvements, and increased understanding of the pathophysiology of spinal conditions.1 In 2017, the number of spine surgery procedures performed worldwide totalled approximately 5.2 million, with procedure numbers forecast to grow at 7.9%, approaching 7.6 million cases annually by 2022.2 As the number of surgeries continues to grow, surveillance and continuous improvement in the quality and safety of spine surgeries constitute important precautions, promoting both patient wellbeing and cost-effective care.
Measuring the safety, quality and outcome of clinical care has become a key research focus in recent years and may involve a variety of approaches and time frames.1 One approach that has become well established as a measure of perioperative quality of care is unplanned return to the operating theatre within 30 days of surgery. Thirty-day reoperation rate has been used to evaluate surgical performance and adverse events3-5 and has been validated across multiple surgical disciplines.6 It has been shown to be a better quality metric than other indirect perioperative outcome measures such as length of hospital stay, surgical site infection rate and mortality rate.3 Furthermore, 30-day reoperation rate has the advantage of being relatively easy to track, arising more frequently than mortality and being relevant to any surgical procedure, enhancing its broader applicability.7
Unplanned reoperation is detrimental to patients, providers and health systems, and has been associated with increased mortality rates and additional healthcare costs. Birkmeyer et al. reported a 6.9-fold increased risk of mortality and 4.6-fold higher costs associated with unplanned 30-day reoperation in general surgery.6 According to the Centers for Medicare and Medicaid Services (CMS), readmission within 30 days of post-surgical discharge cost $17.4 billion in 2008 and has been identified as a target for cost reduction.6 Both the American College of Surgeons' National Surgical Quality Improvement Program (NSQIP) and the Canadian Institute for Health Information monitor 30-day reoperation rates as a key measure of a hospital's quality of care.
Notably, there is sometimes a lack of clarity between the concepts of readmission and reoperation; the terms may be poorly defined and used interchangeably. Readmission refers to 'all cause' readmission and may include medical, surgical, psychological and even social reasons for readmission post surgery. These factors may or may not be related to the initial surgery. Reoperation refers to an unplanned return to the operating room, where the second procedure was not scheduled or planned before the primary surgery and was not related to the disease's natural course.5 Naturally there is an overlap between the two concepts as one would be readmitted to undergo reoperation, unless reoperation took place during the initial hospital stay.
Most previous studies investigating 30-day reoperation and readmission have been conducted in developed countries and have focused on specific pathologies or procedures.8,9 In contrast, relatively little is known about spine surgery outcomes in developing countries, including South Africa. This is an important knowledge gap to address as it would provide insight into perioperative quality of care in our setting and potentially identify areas for improvement. As a starting point, this study focused on the South African private healthcare sector, which serves approximately 16% of the population and is predominated by spinal surgery for degenerative pathologies in older adults. The main aim of the study was to describe the overall rate of 30-day reoperation and 30-day readmission following spine surgery in a large open medical scheme. The secondary aims were to describe the reasons for 30-day reoperation and 30-day reoperation by spine region and for certain procedures.
Methods
Design
This retrospective review was based on inpatient spine surgeries funded by the largest open medical scheme in South Africa between 1 January 2008 and 31 December 2017. The investigation of 30-day reoperation was based on the member's first spine surgery within the study period with included surgeries intended to represent index surgeries.
Patients
All members of the medical scheme > 18 years of age who underwent inpatient spinal procedures in South Africa during the study period were included. Diagnostic and procedure codes for each event were reviewed. Members were excluded from the analysis if: 1) procedure codes indicated medical management only, 2) the 'index' spine surgery was identified as a revision procedure based on diagnostic and/or procedure codes or, 3) the diagnostic code was not related to spine surgery and the procedure codes failed to confirm that a spinal surgery had taken place, 4) data indicating whether reoperation had taken place was missing.
Variables
The data was provided by the medical scheme in the form of an anonymised dataset. Variables related to the index surgery included: member demographics, comorbidity ICD-10 codes, surgery ICD-10 code, surgery Complete Current Procedural Terminology for South Africa (CCSA) codes (procedure codes), surgeon specialisation and year of surgery. Each surgeon had been assigned a unique, anonymous study code by the scheme such that it was possible to distinguish surgeries by the same surgeon. The dataset also indicated whether there had been a 30-day readmission and whether a second spine surgery had taken place within the study period. Readmission ICD-10 codes, second surgery ICD-10 and procedure codes, and the time to the second surgery were included.
Comorbidity ICD-10 codes were assessed for conditions included in the Charlson Comorbidity Index (CCI)10 and CCI scores were calculated as described by Quan et al.11 Surgery ICD-10 code descriptions were analysed and each surgery was categorised according to pathology type, using the ICD-10 code description terminology as far as possible. Spine region was also identified from the surgery ICD-10 code. When the ICD-10 code did not specify a spine region, procedure codes were checked for this information. Spine regions were categorised as cervical, thoracic, lumbar or unspecified.
CCSA codes are used between hospitals and funders to provide details of the medical procedures performed. A licence to access the description associated with each CCSA code was purchased from the South African Medical Association to enable further analysis. Each spinal CCSA code description was evaluated and key surgical elements (e.g. decompression, instrumentation, fusion) were categorised as present or absent. There were typically several CCSA codes associated with each surgery and codes were subsequently analysed collectively to determine the surgical elements present per surgery. This analysis was used to identify certain well-established spinal procedures, representing a range in surgical complexity, for inclusion in the study. These procedures, and the primary CCSA codes most commonly associated with them, are shown in Table I.
Outcomes
Readmission within 30 days was available directly from the dataset provided. In the event of a return to theatre within 30 days, the ICD-10 code and procedure codes associated with the second surgery were evaluated by a fellowship-trained spine surgeon to identify surgeries that took place at the same spine region and were suggestive of a complication of the initial procedure; these were considered 30-day reoperations. The ICD-10 code and procedure codes were also assessed in combination to determine the reason for reoperation, which was categorised accordingly. The category 'neural compression' included both nerve root compression and spinal cord compression as indications and involved decompression surgeries with no concomitant arthrodesis. The category 'instability' included instability resulting from fractures and involved arthrodesis surgeries with no concomitant decompression. The category 'implant issue' referred to surgeries involving the removal or reinsertion of implants only with no concomitant decompression or arthrodesis. The remaining reoperation reason categories included infection, cerebrospinal fluid (CSF) leak and haematoma evacuation.
Data analysis
Descriptive categorical data was presented as frequencies and percentages. Unplanned 30-day reoperation and 30-day all-cause readmission were presented as a cumulative percentage of all surgeries. Unplanned reoperation was also investigated as a cumulative percentage by year and within certain categories of interest: by spine region and by selected surgeries.
Univariate associations between 30-day reoperation and patient- and surgery-related variables were investigated using chi-squared tests. Multivariate associations between surgery characteristics and surgeon specialisation were investigated using binomial logistic regression, and correction for clustering was applied due to the presence of multiple surgeries per surgeon in the dataset. Associations were reported as odds ratios (OR) and were presented with 95% confidence intervals (CI). Analyses were conducted using jamovi version 1.6 (www.jamovi.org), GraphPad Prism version 9.2.0 for Mac OS, GraphPad Software, San Diego, California USA, www.graphpad.com, and Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC with significance accepted at p < 0.05.
Results
In total, 54 998 adult scheme members underwent inpatient spinal procedures during the study period. However, 5 602 surgeries were excluded on the following basis: medical management only (n = 200), revision spine surgery (n = 4 686), insufficient evidence that a spine surgery had taken place (n = 537) and missing data regarding 30-day reoperation (n = 180). The remaining 49 395 surgeries were included in the analysis. Clinical and demographic details of the scheme members who underwent spine surgery are shown in Table II and selected surgeon and surgery characteristics in Table III. The majority of surgeries were for degenerative pathologies such as disc disorders (n = 18 542, 38%) and stenosis (n = 14 315, 29%) in older adults. The mean age at the time of surgery was 54 years (SD 14 years) and, in most cases, individuals were not severely obese (BMI < 35 n = 45 379, 92%), nor did they suffer from serious comorbidities (CCI = 0, n = 39 639, 80%). Spine surgeries were performed predominantly by neurosurgeons (n = 35 409, 72%) and typically involved 2-4 hours of theatre time (n = 24 559, 50%).
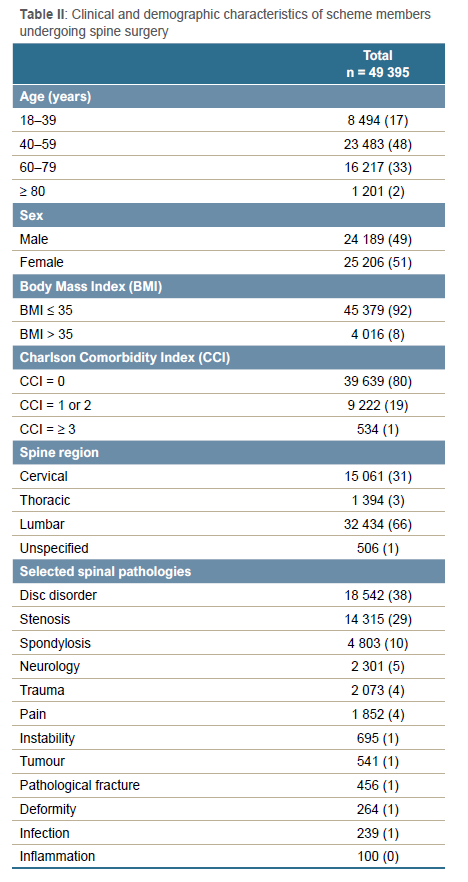
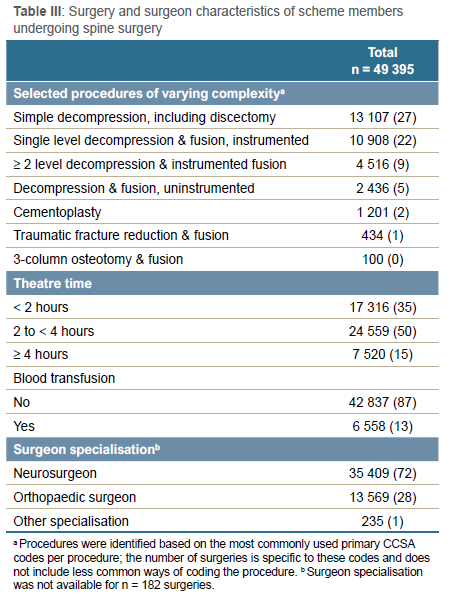
Incidence of 30-day reoperation
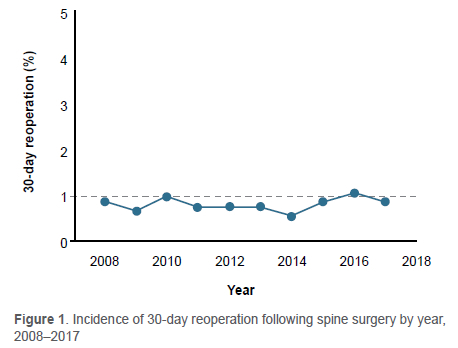
Of the 49 395 members who underwent surgery, 3 204 (6.5%) were readmitted for any cause within 30 days. Furthermore, 415 (0.8%) of the 49 395 members had an unplanned second spine surgery within 30 days. These 415 reoperations comprised 18 members who underwent reoperation as part of the initial admission and 397 members who were readmitted for surgery. The incidence of 30-day reoperation showed no notable trend over the ten-year study period, ranging between 0.6% and 1.1% each year (Figure 1).
When examining the distribution of the 415 reoperations over the 30-day period, notable peaks included day 1 (n = 19, 5%), day 5 (n = 25, 6%) and day 11 (n = 21, 5%) (Figure 2a). When taken in weekly intervals, the number of reoperations was very similar in week 1 and week 2 before declining in week 3 and 4 post index surgery (Figure 2b). The average number of reoperations per day in weeks 1-4 post index surgery was 17.0, 16.3, 12.9 and 10.3, respectively. Based on these values, it could be inferred that the risk of reoperation was 24% lower in week 3 versus week 1 and 39% lower in week 4 versus week 1.
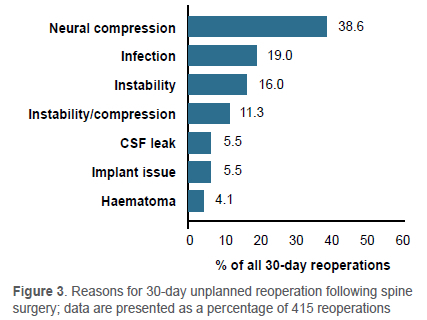
Reasons for 30-day reoperation are shown in Figure 3. Neural decompression was the most common reason (n = 160, 39%), followed by infection (n = 79, 19%) and arthrodesis (n = 66, 16%). Reoperation involving arthrodesis suggested instability as an indication. For a further 47 (11%) reoperations, both decompression and arthrodesis were performed, and it was not possible to distinguish the predominant indication. The distribution of reoperations for the three most common reoperation indications are shown in Figure 4. In all cases, reoperations occurred throughout the 30-day period with no clear pattern observed.
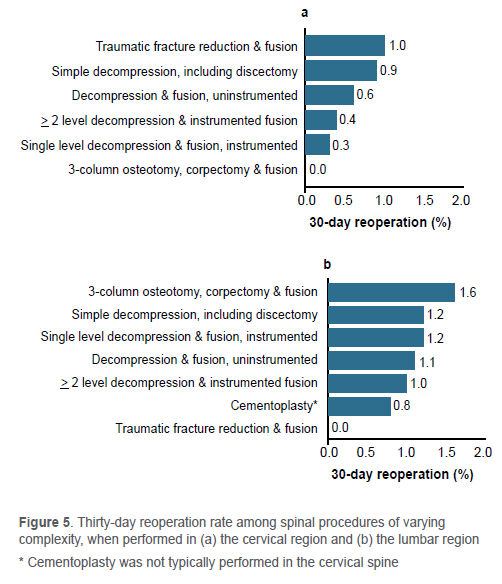
30-day reoperation by region and selected procedures
When investigating 30-day reoperation by spine region, the thoracic (13 of 1 394; 0.9%) and lumbar (337 of 32 434; 1.0%) regions had a very similar reoperation rates whereas the reoperation rate following cervical spine surgery was lower (60 of 15 061; 0.4%). Within the selected procedures of varying complexity, a similar pattern of higher reoperation rates in the lumbar versus cervical region was observed (Figure 5). However, overall the procedure-specific 30-day reoperation rates were < 1.6%. Although the most complex procedure, 3-column osteotomy, corpectomy and fusion, had the highest 30-day reoperation rate among the lumbar surgeries, no overall association between procedure complexity and 30-day reoperation was observed (Figure 5).
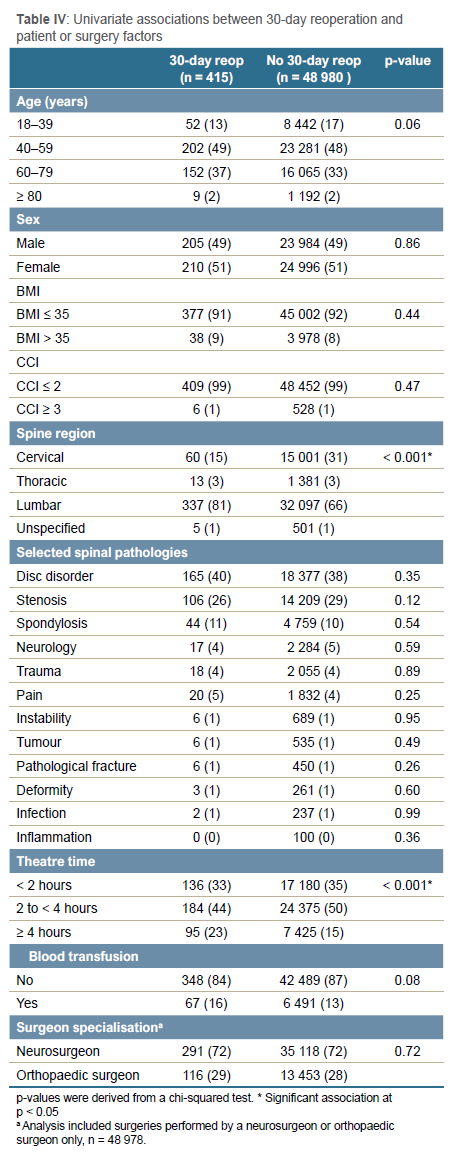
Factors associated with 30-day reoperation
Only spine region and theatre time were significantly associated with 30-day reoperation in univariate analyses, although age and receiving a blood transfusion showed a strong trend toward significance (Table IV). Variables with a univariate association at p < 0.20 were included in a multiple regression analysis with crude and adjusted odds ratios (aOR) presented in Table V. After adjusting for all the variables in the model, members 40-59 and 60-79 years of age had significantly higher odds of reoperation than those 18-39 years old. Furthermore, surgery to the lumbar spine had almost three times the odds of reoperation compared to surgery to the cervical spine, and theatre time of > 4 hours was associated with significantly higher odds of reoperation than theatre time of less than two hours. Finally, surgery for stenosis was associated with significantly lower odds of 30-day reoperation compared to other spinal pathologies.
Discussion
The first finding of the study was that adult members of the largest open medical scheme in South Africa had an all-cause 30-day readmission rate of 6.5% and an unplanned 30-day reoperation rate of 0.8% following spinal surgery. Many existing studies have investigated readmission and reoperation within the context of specific pathologies or procedures,9,12-14 rendering direct comparison with this study difficult. However, the current readmission rate was on par with the findings of a systematic review focusing on North American literature which reported a readmission rate of 5.5% (95% CI 4.2-7.4%) following spine surgery.15 The current findings were also similar to those from the American NSQIP database.16,17 One NSQIP study included 111 892 patients who underwent spinal surgery between 2012 and 2014 and found a readmission rate of 5.2% and 30-day reoperation of 3.1%.17 An earlier NSQIP study investigated 30-day reoperation following spine surgery between 2005 and 2010 and found an almost identical rate of 3.15%.16 Thus, it appears that the quality of spine surgery in the current private sector population, when assessed by acute complications, is comparable to developed countries in terms of readmission rates and possibly slightly superior in terms of 30-day reoperation rates. One possible explanation for this is that spine surgeries in the South African private healthcare sector are typically performed by fully qualified surgeons whereas other studies may have included spine surgeries performed at training institutions. In other words, the current data may reflect less of the steep learning curve associated with spinal surgery.
A second finding of the study was that neural decompression was the most common reason for a return to theatre, accounting for at least 39% of 30-day reoperations. This value may be a slight underestimate as a further 11% of reoperations included both decompression and arthrodesis and it was not possible to distinguish whether neural compression or instability was the original indication. Ongoing radicular pain after spine surgery may have multiple causes including inadequate decompression initially, ongoing compression at an unoperated but adjacent level, wrong level surgery, and screw malposition causing new radicular symptoms. Other reasons for 30-day reoperation were noticeably less prevalent at < 19% of reoperations and < 0.5% of all surgeries, suggesting that existing practices are largely effective for preventing these acute complications (e.g. infection). Comparison to the existing literature is challenging in that many previous studies have not provided the reasons for 30-day reoperation or have reported findings for a specific pathology or procedure.9,12,13,18 For example, one large study found a 30-day reoperation rate of 5% following adult spinal deformity surgery and reported that neurological compromise was the most common indication.20 In another study, unplanned 30-day reoperation following elective posterior lumbar spinal fusion was 3.4% with the most common reasons including haematoma drainage (9.9%), drainage of lumbar spine abscess (9.1%), exploration of spinal fusion (8.8%), and drainage of complex, postoperative wound infection (8.2%).9 These differences in reoperation reasons are likely related to marked differences in the patients and surgeries concerned.
Although the overall rate of 30-day reoperation was low, some variation was observed when evaluating reoperation by spine region. Unplanned 30-day reoperation rates for surgery performed on the thoracic (0.9%) and lumbar (1.0%) spine were more than double that of cervical surgery (0.4%). Lumbar spine surgery is known to have high complication rates and numerous studies have confirmed it as an independent risk factor for 30-day reoperation.9,15,17 There is a paucity of information regarding reoperation within the thoracic spine; however, a study that investigated posterior surgery for thoracic spinal stenosis in 1 948 patients, reported an unplanned 30-day reoperation rate of 3.95%.20 In contrast, a retrospective cohort study including 13 435 cervical spine surgeries reported a reoperation rate of 1.24%.21 While spine regions were seldom compared in the same study, our findings support the perceived lower risk of 30-day reoperation following cervical spine surgery. Furthermore, the current cervical spine reoperation rate was noticeably lower than that previously reported.
To our knowledge, no previous study compares 30-day reoperation rates across procedure types based on varying complexity. Assessment of the data within the specific procedure groups based on complexity further supports the lower risk of reoperation in the cervical spine. Although the most complex procedure, 3-column osteotomy and fusion had the highest 30-day reoperation rate among the lumbar surgeries; it was surprisingly not dramatically higher. There was no obvious trend of most complex procedures having the highest complication rate and simplest procedures the lowest; therefore, no overall association between procedure complexity and 30-day reoperation was observed. This is in keeping with a previous study assessing predictors of postoperative complications after surgery for lumbar spinal stenosis and degenerative lumbar spondylolisthesis: multilevel cases were not found to be significant predictors of 30-day complications.13 It is possible that patients with particularly high risk and complicated surgeries receive more intensive pre- and postoperative care, decreasing likelihood of reoperation. Another explanation may be that complex procedures are typically performed by experienced surgeons, which may lower the risk of complication.
A final finding of the study was that in patients aged 40-59 years and 60-79 years, surgery to the lumbar spine and theatre time of > 4 hours were associated with significantly higher odds of 30-day reoperation compared to the reference categories in multivariate analyses. Patients under 40 years of age would generally be expected to be healthier than those over 40, whereas patients > 80 may be associated with extra caution in patient screening and less extensive procedures. Thus, the age-related finding is reasonable. The association between lumbar surgery and reoperation has been mentioned previously.9,15,17 Longer theatre time may be associated with more complex, invasive procedures and increased risk of infection; thus this finding is also reasonable. Identifying factors associated with 30-day reoperation have been the primary objective of most previous studies on this topic, and significant risk factors identified have included obesity (body mass index > 35), American Society of Anaesthesiologists (ASA) score > 3, disseminated cancer, bleeding disorders, and multilevel fusion.9,16,17 While there has been variation in the risk factors investigated, one notable contrast was that the current study did not find an association between BMI > 35 and 30-day reoperation, unlike most previous studies.9,16,17 The finding of no association between surgeon specialisation and 30-day reoperation was in keeping with previous studies, which reported similar rates of mortality, 30-day readmission and surgical site infection following spine surgery by a neurosurgeon or orthopaedic surgeon.8,23
Limitations of the study include that it was based on retrospective data collected for administrative purposes and was dependent on the accuracy of the information recorded. ICD-10 codes did not always reflect the indication for reoperation, and it was necessary to rely on ICD-10 and procedure codes in combination for identifying a reoperation reason. Furthermore, the nature of the data precluded an in-depth understanding of the reasons for reoperation and limited the potential risk factors available for investigation. Although the largest open medical scheme provided a reasonable representation of the private sector, differences in member profiles between schemes may affect the generalisability of the findings.
Conclusion
Spine surgery among members of a large open medical scheme in South Africa was associated with low rates of 30-day readmission and reoperation. Furthermore, the rates compared favourably with those from developed countries. These initial findings suggest competent surgeons and good quality of perioperative care within the private sector setting. Future research should investigate long-term spinal surgery outcomes in the private sector as well as short-and long-term outcomes of spinal surgery in the public sector to provide comprehensive insight into the quality of spinal surgery care in South Africa.
Acknowledgements
The anonymised data analysed for the purposes of this study was obtained from Discovery Health Medical Scheme, registration number 1125, and with the support and assistance of Discovery Health (Pty) Ltd, an accredited administrator and managed care provider for medical schemes. Discovery Health Medical Scheme and Discovery Health (Pty) Ltd had no influence on the methodology used, analysis completed and conclusions drawn in this research, and the outcome of the research is entirely independent from Discovery Health Medical Scheme and Discovery Health (Pty) Ltd.
Compliance with ethical guidelines
The authors declare that this submission is in accordance with the principles laid down by the Responsible Research Publication Position Statements as developed at the 2nd World Conference on Research Integrity in Singapore, 2010.
Prior to the commencement of the study, ethical approval was obtained from the following ethical review board: Stellenbosch University Health Research Ethics Committee, reference number N19/10/152.
All procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
A waiver of informed consent was granted by the ethics committee due to the use of retrospective, anonymised data.
Declaration
The authors declare authorship of this article and that they have followed sound scientific research practice. This research is original and does not transgress plagiarism policies.
Author
MvH: study conceptualisation, data capture, data analysis, first draft preparation, manuscript preparation and revision
TNM: study conceptualisation, data capture, data analysis, first draft preparation, manuscript preparation and revision
RND: study conceptualisation, design, manuscript revision
AJV: study conceptualisation, design, manuscript revision
JHD: study conceptualisation, data capture, data analysis, manuscript revision
ORCID
Van Heukelum M https://orcid.org/0000-0001-9160-7796
Mann TN https://orcid.org/0000-0002-9750-5106
Dunn RN https://orcid.org/0000-0002-3689-0346
Vlok AJ https://orcid.org/0000-0002-3202-2867
Davis JH https://orcid.org/0000-0002-1909-7629
References
1. Jiang F, Wilson JRF, Badhiwala JH, et al. Quality and safety improvement in spine surgery. Global Spine J. 2020;10:17S-28S. [ Links ]
2. Research and Markets. Spinal Surgery- Global trends. 2018 https://www.researchandmarkets.com/reports/4825317/spine-surgery-global-trends-and-opportunities (accessed 10 Aug 2022). [ Links ]
3. Schipmann S, Schwake M, Suero Molina E, et al. quality indicators in cranial neurosurgery: which are presently substantiated? A systematic review. World Neurosurg. 2017;104:104-12. [ Links ]
4. Birkmeyer JD, Dimick JB, Birkmeyer NJO. Measuring the quality of surgical care: structure, process, or outcomes? J Am Coll Surg. 2004;198:626-32. [ Links ]
5. Huang WC, Chen YJ, Lin MHC, Lee MH. Analysis of neurosurgical procedures with unplanned reoperation for quality improvement A 5-year single hospital study. Medicine (United States) 2021;100:e28403. [ Links ]
6. Birkmeyer JD. Is unplanned return to the operating room a useful quality indicator in general surgery? Arch Surg. 2001;136:405-11. [ Links ]
7. Birkmeyer JD, Dimick JB, Birkmeyer NJO. Measuring the quality of surgical care: structure, process, or outcomes? J Am Coll Surg. 2004;198:626-32. [ Links ]
8. McCutcheon BA, Ciacci JD, Marcus LP, et al. Thirty-day perioperative outcomes in spinal fusion by specialty within the NSQIP database. Spine (Phila Pa 1976) 2015;40:1122-31. [ Links ]
9. Durand WM, Eltorai AEM, Depasse JM, et al. Risk factors for unplanned reoperation within 30 days following elective posterior lumbar spinal fusion. Global Spine J. 2018;8:388-95. [ Links ]
10. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1987;40:373-83. [ Links ]
11. Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130-39. [ Links ]
12. Basques BA, Varthi AG, Golinvaux NS, et al. Patient characteristics associated with increased postoperative length of stay and readmission after elective laminectomy for lumbar spinal stenosis. Spine (Phila Pa 1976). 2014;39:833-40. [ Links ]
13. Turcotte JJ, Patton CM. Predictors of postoperative complications after surgery for lumbar spinal stenosis and degenerative lumbar spondylolisthesis. J Am Acad Orthop Surg Glob Res Rev. 2018;2:e085. [ Links ]
14. Martin I, Mirza K, Comstock A, et al. Reoperation rates following lumbar spine surgery and the influence of spinal fusion procedures. Spine (Phila Pa 1976);32:382-87. [ Links ]
15. Bernatz JT, Anderson PA. Thirty-day readmission rates in spine surgery: Systematic review and meta-analysis. Neurosurg Focus. 2015;39:E7. [ Links ]
16. Bekelis K, Desai A, Bakhoum SF, Missios S. A predictive model of complications after spine surgery: the National Surgical Quality Improvement Program (NSQIP) 2005-2010. Spine J. 2014;14:1247-55. [ Links ]
17. Piper K, DeAndrea-Lazarus I, Algattas H, et al. Risk factors associated with readmission and reoperation in patients undergoing spine surgery. World Neurosurg. 2018;110:e627-35. [ Links ]
18. De la Garza Ramos R, Nakhla J, Echt M, et al. Risk factors for 30-day readmissions and reoperations after 3-column osteotomy for spinal deformity. Global Spine J. 2018;8:483-89. [ Links ]
19. Scheer JK, Tang JA, Smith JS, et al. Reoperation rates and impact on outcome in a large, prospective, multicenter, adult spinal deformity database. J Neurosurg Spine. 2013;19:464-70. [ Links ]
20. Hu Y, Ouyang H, Ye K, et al. Thirty-day unplanned reoperations after posterior surgery for thoracic spinal stenosis: a single-center study based on 1948 patients. Spine (Phila Pa 1976). 2023;48:507-13. [ Links ]
21. Patel V, Metz A, Schultz L, et al. Rates and reasons for reoperation within 30 and 90 days following cervical spine surgery: a retrospective cohort analysis of the Michigan spine surgery improvement collaborative (MSSIC) registry. Spine J. 2023;23:116-23. [ Links ]
22. Seicean A, Alan N, Seicean S, et al. Surgeon specialty and outcomes after elective spine surgery. Spine (Phila Pa 1976). 2014;39:1605-13. [ Links ]
Received: June 2023
Accepted: August 2023
Published: March 2024
Editor: Prof. Nando Ferreira, Stellenbosch University, Cape Town, South Africa
Funding: No funding was received for this study.
Conflict of interest: The authors declare they have no conflicts of interest that are directly or indirectly related to the research.
* Corresponding author: jdavis@ior.health














