Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SA Orthopaedic Journal
versión On-line ISSN 2309-8309
versión impresa ISSN 1681-150X
SA orthop. j. vol.22 no.4 Centurion 2023
http://dx.doi.org/10.17159/2309-8309/2023/v22n4a4
TRAUMA AND GENERAL ORTHOPAEDICS
Soft tissue reconstruction of Gustilo-Anderson grade 3B open tibia fractures at a tertiary hospital: a retrospective case series
Dane MaiminI, *; Elyas BarouniII; Christopher PriceII; Donald HudsonII; Saleigh AdamsII; Maritz LaubscherI
IOrthopaedic Research Unit, Division of Orthopaedic Surgery, Groote Schuur Hospital, University of Cape Town, Cape Town, South Africa
IIDivision of Plastic and Reconstructive Surgery and Division of Orthopaedic Surgery, Groote Schuur Hospital, University of Cape Town, Cape Town, South Africa
ABSTRACT
BACKGROUND: The management of Gustilo-Anderson grade 3B open tibia fractures are challenging due to the high complication rates, including infection, non-union and amputation. Despite developing treatment options for these injuries, the optimal soft tissue cover option and timing of definitive surgery remains unclear and is often dictated by local context and available surgical expertise rather than the gold standard of care. The authors aimed to review the surgical techniques and outcomes for the management and reconstruction of the soft tissues in Gustilo-Anderson grade 3B tibia fractures treated at a tertiary hospital in South Africa.
METHODS: A retrospective study was conducted on 22 patients who underwent soft tissue reconstruction for grade 3B tibia fractures from January 2014 to July 2017. Patient demographics, medical comorbidities, injury characteristics and management practices such as time to debridement, relook time, use of negative pressure wound therapy (NPWT), soft tissue coverage techniques and complications were recorded and analysed.
RESULTS: Most patients were males (n = 18; 82%) with an average age of 39.3 years (range 15-69). Pedestrian vehicle accidents accounted for 45% (n = 10), followed by motor vehicle accidents (n = 6; 27%) and gunshot wounds (n = 2; 9%). Most patients (n = 18; 82%) were initially debrided within 24 hours. The mean time for NPWT usage prior to cover was 12.5 days. The mean time before soft tissue cover was attempted was 13.7 days (range 2-35). Fasciocutaneous flaps (n = 11; 50%) were the most common method used to achieve bony cover, followed by pedicled muscle flaps (n = 8; 36%), free flaps (n = 2; 9%) and skin grafts (n = 1; 5%). Most patients (n = 13; 59%) achieved satisfactory outcomes. Seven (32%) required soft tissue revisions. Additional complications included complete flap loss resulting in amputation, partial skin graft loss and soft tissue infection. Fewer complications were seen in patients who were first debrided within 24 hours from time of injury.
CONCLUSION: Due to a resource constraint in our working environment, it is not possible to accurately follow available treatment guidelines in our management of grade 3B open tibia fractures. Despite this, the outcomes seen in this small sample were in keeping with those seen in the literature.
Level of evidence: Level 4
Keywords: open tibia fracture, soft tissue reconstruction
Introduction
Open tibia fractures typically represent high-energy trauma that results in significant damage to adjacent soft tissues and neurovascular structures.1 Falls from height, road-traffic accidents, direct blows and sporting injuries are common causes of open tibia fractures. These injuries tend to occur in males with a peak incidence in the fourth decade of life.2 The annual incidence of open long bone fractures has been estimated at 3.4-11.5% per 100 000 population, with 40% occurring in the lower limb, most commonly the tibia diaphysis.1-3 The subcutaneous nature of the anteromedial midshaft tibia both increases the likelihood of fractures in this area communicating with the outside environment and poses soft tissue treatment challenges. Although irrigation and surgical debridement is a critical step in managing these injuries, the relevance of the timing of this first surgery remains debateable. Historically, it was thought that open fractures should have their first debridement in theatre within six hours of injury for best results.4,5 However, studies show no statistically significant increase in infection rates after a delay to irrigation and surgical debridement of between 12 and 24 hours, provided that antibiotic treatment was initiated early.6-8
The optimal timing of definitive soft tissue cover remains a source of ongoing debate. Earlier schools of thought advocated external fixation, surgical debridement (often multiple) and delayed closure.9 Godina et al. were the first to pioneer the use of microvascular free flaps to cover open fracture wounds in the acute (less than three days) setting.10 Expanding from this work, treatment options have shifted from external to internal fixation and immediate soft tissue coverage. This involves a surgical team with both orthopaedic and plastic surgeons, and the term 'fix and flap' was coined.
Early soft-tissue restoration may be undertaken using a variety of techniques including free flaps, pedicled flaps, muscle flaps and cross leg flaps. Studies have reported overall success rates of up to 90%.10-12 Of these options, muscle flaps and dorsalis pedis island flaps have been shown to have lower complication rates, shorter hospital stay and shorter theatre time.12-14 Gopal et al. reported a series of nine pedicle flaps and 75 free muscle flaps. They recorded a 3.5% flap failure rate after immediate internal fixation followed by soft tissue reconstruction if performed within 72 hours after injury.15 The choice of soft tissue reconstruction should be individualised and tailored to the specific clinical scenario.
In our local setting, the 'fix and flap' approach is often not practical due to a high trauma burden, lack of theatre time, and lack of surgeon expertise to perform these complicated soft tissue procedures.8 Negative pressure wound therapy (NPWT) has been shown to expedite wound healing time by 35-54% when compared to conventional wound dressings, and may decrease infection rates in open tibia fractures.16,17 NPWT may be used to achieve soft tissue coverage via secondary intention or alternatively as a temporising method which promotes wound bed granulation while definitive soft tissue procedures are planned.8,17 Although the WOLFF trial suggested no difference in outcomes at 12 months when comparing NPWT to standard dressings in open fractures of the lower limbs, the patients in their cohort all had wound closure within 48-72 hours and their findings are likely not applicable in our local context.18
Despite advances in both soft-tissue management and fracture fixation, it is extremely difficult to achieve satisfactory treatment outcomes in open fractures of the tibia, and complications are commonly reported. Wound infection, flap failure, osteomyelitis, non-union and delayed limb amputation are frequently seen.19
This study aimed to investigate the management strategy and outcomes of soft tissue reconstruction of Gustilo-Anderson grade 3B tibia fractures at a tertiary hospital in South Africa.
Methods
A retrospective study was conducted on patients who had had soft tissue reconstruction for Gustilo-Anderson grade 3B tibia fractures from January 2014 to July 2017 at a tertiary hospital in South Africa. All patients were above the age of 14 years old and had a minimum follow-up of 12 months.
Basic demographic information such as age, sex and comorbid conditions were collected. Factors related to injury such as mechanism of injury, site of fracture and type of soft tissue injury were also recorded. Data with respect to wound management such as time to first debridement, subsequent re-debridement times and frequencies, NPWT, dressing usage, method and timing of soft tissue coverage, soft tissue healing and complications were also recorded. A satisfactory outcome was defined as a healed, infection-free soft tissue reconstruction, with no bone uncovered.
Complications were recorded and grouped into one of the following options: amputation, complete flap loss, partial split skin graft (SSG) loss, soft tissue infection, soft tissue infection and SSG loss.
Data was analysed using descriptive statistics on the continuous data, with calculation of means (with minimum and maximum values), frequency and percentages for the dichotomous data. Categorical data was compared using the chi-squared test. STATA statistical package version 14 was used to analyse the data.
Results
A cohort of 60 patients with grade 3 open tibia fractures was analysed, but only 22 patients met the grade 3B inclusion criteria. The majority were males (n = 18; 82%), with a mean age of 33.9 years (15-69). Seventy-three per cent (n = 16) of patients were in the age range of 20-39 years (Table I). More than 50% of patients had no medical comorbidity.
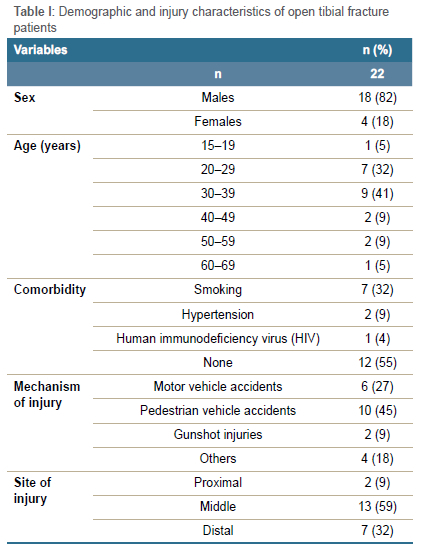
Pedestrian vehicle accidents (PVA) (n = 10; 45%) were the most common mechanism of injury, followed by motor-vehicle accidents (MVA) (n = 6; 27%) and gunshot wounds (GSW) (n = 2; 9%). The commonest site of injury occurred at the middle third of the tibia (n = 13; 59%), followed by the distal third (n = 7; 32%) and proximal third (n = 2; 9%).
Most patients were debrided within 24 hours (n = 13; 59%) of injury (Table II). Forty-five per cent of patients had a subsequent re-debridement after 48 hours (n = 10; 45%), and 68% (n = 15) of patients had one or more relooks in theatre.
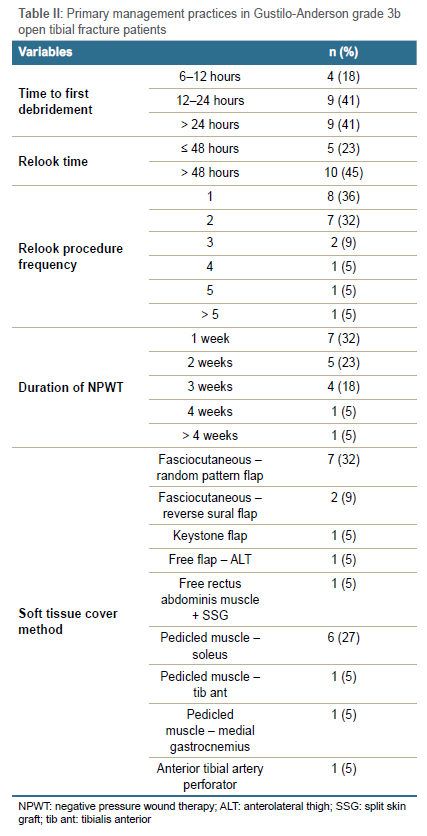
NPWT was used in 82% (n = 18) of patients. The average duration of NPWT was 12.5 days (range 2-42). Seven patients (32%) had NPWT for one week or less post injury, six patients (27%) for between one and two weeks, and nine patients (41%) for more than two weeks before definitive tissue cover. One patient had NPWT for more than four weeks post injury prior to definitive soft tissue cover.
Definitive soft tissue cover occurred at an average of 13.7 days post injury (range 2-35). A variety of techniques were used to achieve soft tissue coverage; random pattern fasciocutaneous flaps (n = 7; 32%) and pedicled muscle flaps (n = 6; 27%) predominated (Table II).
Random pattern fasciocutaneous flaps provided soft tissue coverage in seven patients (32%) with three used at the distal third of the tibia (14%) and four used at the middle third of the tibia (18%) (Figure 1). Pedicled muscle flaps were used in the middle third in four patients (18%) and proximal third (n = 2, 9%). The reversed sural flap was utilised distally in two patients (9%).
Most patients received satisfactory outcomes following soft tissue reconstruction (Table III). Seventeen patients (77%) achieved soft tissue coverage within three weeks post injury, while FIve achieved cover after three weeks. Seven patients (32%) required soft tissue revisions post initial cover. Nearly two-thirds of patients (n = 13; 59%) did not report any complications, whereas the remainder were found to have at least one of the FIve reported complications. Only one patient (5%) underwent an amputation following complete flap failure and fracture-related infection. Three patients (14%) had complete flap loss resulting in amputation, partial skin graft loss and soft tissue infection.
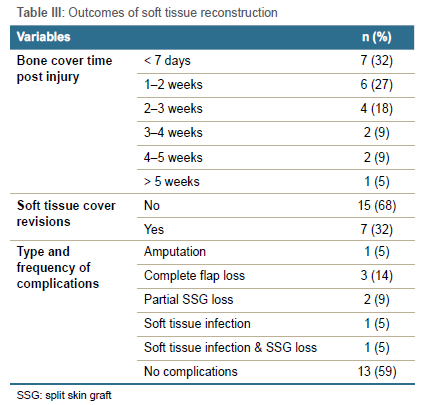
Complications occurred in three of the seven (43%) random pattern fasciocutaneous flaps with complete flap loss occurring in two patients and partial skin graft loss in the remaining patient. There were complications in two of the eight (20%) pedicled muscle flaps, namely partial skin graft loss and soft tissue infection with skin graft loss. The single anterolateral thigh (ALT) free flap that was performed ultimately resulted in flap failure, fracture-related infection and amputation (Figure 2).
Thirteen patients (59%) were debrided within the first 24 hours. Five of them (38%) experienced various complications. Interestingly, those patients who were debrided beyond 24 hours, reported fewer complications; 67% (n = 6) had no complications, and the only complication was one soft tissue infection (Figure 3).
There appeared to be better outcomes in the delayed relook time of greater than 48 hours (n = 10; 45%) with reduced revision requirements, earlier discharge time and fewer complications (Figure 4).
Discussion
This study reviews the outcomes of soft tissue reconstruction of Gustilo-Anderson grade 3B tibia fractures over a three-year period at a tertiary hospital in South Africa. Our cohort shared many similarities with contemporary literature from similar low-to-middle income countries, notably, age and sex, most common mechanism of injury, most common site of injury.
Seventy-three per cent were males aged 20-39 years old, and demonstrates that this demographic is at the highest risk for open tibial fractures.20-22 Road traffic accidents continue to be cited as the leading cause of these high energy fractures, as was the case with 70% of our cohort.20,23,24 Nearly two-thirds of all fractures occurred in the middle third of the tibia where the soft tissue anatomy predisposes to open fractures and potential soft tissue coverage problems.
The veracity of the 'six-hour rule' has been called into question in recent literature; however, it is still quoted in many treatment guidelines for open fracture management.25,26
The first debridement in our cohort was performed within 24 hours of initial presentation in approximately 60% of patients. The remaining approximately 40% of our cohort underwent their first debridement after 24 hours. Our outcomes were not in keeping with this reported benefit when debrided within six hours. We found that there was no statistically significant difference in complications when comparing patients debrided within 24 hours and those that were debrided more than 24 hours after initial presentation (x2[1, n = 22] = 1.2664, p = 0.26). In this cohort of patients, there was no benefit found if a patient was debrided within the first 24 hours post injury. Unexpectedly, those patients who were first debrided after 48 hours experienced fewer complications although it is noted that this is likely a type 2 statistical error due to our small sample size.
Early or delayed wound closure is debatable and local context and resources need to be considered. Many authors support delayed wound closure, while others promote early coverage, citing its potential advantages and benefits.8,12 It has, however, been shown that closure should be attempted within 72 hours to avoid higher rates of flap failure/loss and infection. When this is not possible, NPWT may be a useful temporising measure.8,16,17 Acceptable rates of infection can be achieved with closure beyond 72 hours.27 More than 50% of patients in our study had NPWT within the first two weeks post injury in our cohort, demonstrating no standardisation of treatment protocols.
Among the various types of soft tissue cover flaps used, the random pattern fasciocutaneous flap (32%) and pedicled muscle flap (27%) predominated. The potential advantages of using fasciocutaneous flaps include their simplicity, availability, versatility replacing 'like with like' and preserving underlying muscle function.28,29 This versatility has resulted in other studies reporting the use of fasciocutaneous flaps in up 85% of cases.30 This popular technique is, however, not free of complications, and revision flaps of soft tissue cover after fasciocutaneous flap have been reported by Hallock et al. in 15-43% of cases due to peripheral vascular insufficiency.29 Similar rates (14%) of random fasciocutaneous flap complications were found in our cohort which include complete flap loss (9%) and soft tissue infection (5%). This cohort confirms the high failure rate in random pattern fasciocutaneous flaps in a traumatic setting where there is often extensive damage to the soft tissue. It should be noted that, during the study period, our institution had limited access to a microvascular service and free tissue transfer was not available for most cases.
The major study limitations were its retrospective nature with a small sample size insufficient for statistical and quantitative subgroup analysis. Nevertheless, this preliminary study revealed the pattern of primary and surgical management practices performed within a tertiary hospital setting, and it assessed the outcomes of commonly used practices which may lead to the potential standardised protocol being developed for our facility after evaluation of a larger sample size.
Conclusion
We found a high rate of complications associated with soft tissue cover of grade 3B open tibia fractures. Based on our outcomes it is not possible to extrapolate a protocol-based treatment algorithm for these devasting injuries. It remains clear that these challenging injuries require early specialised intervention for optimal outcomes. Future studies with a larger sample size and longer follow-up are recommended from which a standard working protocol may be developed for this facility.
Ethics statement
The authors declare that this submission is in accordance with the principles laid down by the Responsible Research Publication Position Statements as developed at the 2nd World Conference on Research Integrity in Singapore, 2010. Prior to commencement of the study, ethical approval was obtained from the following ethical review board: 511/2018 (University of Cape Town Human Research Ethics Committee).
All procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Informed written consent was not obtained from all patients for being included in the study; however, the data was collected retrospectively and anonymised.
Declaration
The authors declare authorship of this article and that they have followed sound scientific research practice. This research is original and does not transgress plagiarism policies.
Author contributions
DM: data analysis, manuscript preparation and finalisation EB: study conceptualisation, study design, data capture, data analysis, first draft preparation
CP: case contribution, manuscript review
DH: manuscript review
SA: study design, manuscript review
ML: study design, data analysis, manuscript review
ORCID
Maimin D https://orcid.org/0000-0002-1106-9930
Barouni E https://orcid.org/0000-0002-6392-0133
Price C https://orcid.org/0000-0002-9083-2462
Adams S https://orcid.org/0000-0002-0552-9400
Laubscher M https://orcid.org/0000-0002-5989-8383
References
1. Giannoudis PV, Papakostidis C, Roberts C. A review of the management of open fractures of the tibia and femur. J Bone Jt Surg - Ser B. 2006;88:281-89. https://doi.org/10.1302/0301-620X.88B3.16465/FORMAT/EPUB [ Links ]
2. Court-Brown CM, Bugler KE, Clement ND, et al. The epidemiology of open fractures in adults. A 15-year review. Injury. 2012;43:891-97. https://doi.org/10.1016/jJnjury.2011.12.007 [ Links ]
3. Larsen P, Elsoe R, Hansen SH, et al. Incidence and epidemiology of tibial shaft fractures. Injury. 2015;46:746-50. https://doi.org/10.1016/jinjury.2014.12.027 [ Links ]
4. Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am. 1976;58:453-58. [ Links ]
5. Werner CML, Pierpont Y, Pollak AN. The urgency of surgical débridement in the management of open fractures. J Am Acad Orthop Surg. 2008;16:369-75. https://doi.org/10.5435/00124635-200807000-00002 [ Links ]
6. Schenker ML, Yannascoli S, Baldwin KD, et al. Does timing to operative debridement affect infectious complications in open long-bone fractures? A systematic review. J Bone Joint Surg Am. 2012;94:1057-64. https://doi.org/10.2106/JBJSK.00582 [ Links ]
7. Li J, Wang Q, Lu Y, et al. Relationship between time to surgical debridement and the incidence of infection in patients with open tibial fractures. Orthop Surg. 2020;524-32. https://doi.org/10.1111/os.12653 [ Links ]
8. Manjra M, Basson T, Du Preez G, et al. Current concepts in the management of open tibia fractures. SA Orthop J. 2019;18(4):52-62. https://doi.org/10.17159/2309-8309/2019/v18n4a7 [ Links ]
9. Gopal S, Giannoudis P V, Murray A, et al. The functional outcome of severe, open tibial fractures managed with early fixation and flap coverage. J Bone Jt Surg [Br]. 2004;86:861-68. https://doi.org/10.1302/0301-620X.86B6 [ Links ]
10. Godina M. Early microsurgical reconstruction of complex trauma of the extremities. Plast Reconstr Surg. 1986;78:285-92. https://doi.org/10.1097/00006534-198609000-00001 [ Links ]
11. Yazar S, Lin C-H, Wei F-C. One-stage reconstruction of composite bone and soft-tissue defects in traumatic lower extremities. Plast Reconstr Surg. 2004;114:1457-66. https://doi.org/10.1097/01.prs.0000138811.88807.65 [ Links ]
12. Gopal S, Majumder S, Batchelor AGB, et al. Fix and flap: the radical orthopaedic and plastic treatment of severe open fractures of the tibia. J Bone Joint Surg Br. 2000;82-B:959-66. https://doi.org/10.1302/0301-620x.82b7.0820959 [ Links ]
13. Riegels-Nielsen P, Krag C, Medgyesi S, Pers M. The repair of soft tissue defects in the lower leg: a comparison of different flap techniques. Acta Orthop Scand. 1983;54:772-76. https://doi.org/10.3109/17453678308996628 [ Links ]
14. Chan JK-K, Cantab M, Harry L, et al. Soft tissue reconstruction of open fractures of the lower limb: muscle versus fasciocutaneous flaps. Plast Reconstr Surg. 2012 Aug;130(2):284e-295e. https://doi.org/10.1097/PRS.0b013e3182589e63 [ Links ]
15. Gopal S, Majumder S, Batchelor AGB, et al. Fix and flap: the radical orthopaedic and plastic treatment of severe open fractures of the tibia. J Bone Joint Surg Br. 2000 Sep;82(7):959-66. [ Links ]
16. Kumaar A, Shanthappa AH, Ethiraj P. A comparative study on efficacy of negative pressure wound therapy versus standard wound therapy for patients with compound fractures in a tertiary care hospital. Cureus. 2022;14:1-7. https://doi.org/10.7759/cureus.23727 [ Links ]
17. Kim JH, Lee DH. Negative pressure wound therapy vs. conventional management in open tibia fractures: Systematic review and meta-analysis. Injury. 2019;50:1764-72. https://doi.org/10.1016/j.injury.2019.04.018 [ Links ]
18. Costa ML, Achten J, Bruce J, et al. Effect of negative pressure wound therapy vs standard wound management on 12-month disability among adults with severe open fracture of the lower limb: the WOLLF Randomized Clinical Trial. J Am Med Assoc. 2018;319:2280-88. https://doi.org/10.1001/jama.2018.6452 [ Links ]
19. Harris AM, Althausen PL, Kellam J, et al. Complications following limb-threatening lower extremity trauma. J Orthop Trauma. 2009;23:1-6. https://doi.org/10.1097/BOT.0b013e31818e43dd [ Links ]
20. Gichuhi K, Glasgow O. Injury pattern among non-fatal road traffic crash victims. East African Orthop J. 2010;1:23-25. https://doi.org/10.4314/eaoj.v1i1.49454 [ Links ]
21. National Trauma Data Base, second report. January to December 2007. Ministry of Health Malaysia. Accessed 18 Oct 2022. https://www.yumpu.com/en/document/read/53924328/second-report [ Links ]
22. Singh A, Hao JTJ, Wei DT, et al. Gustilo IIIB open tibial fractures: an analysis of infection and nonunion rates. IJOO. 2018;52:406-410. https://doi.org/10.4103/ortho.IJOrtho_369_1623 [ Links ]
23. Court-Brown CM, Rimmer S, Prakash U, McQueen MM. The epidemiology of open long bone fractures. Injury. 1998;29:529-34. https://doi.org/10.1016/s0020-1383(98)00125-9 [ Links ]
24. Ikem IC, Oginni LM, Bamgboye EA. Open fractures of the lower limb in Nigeria. Int Orthop. 2001;25:386. https://doi.org/10.1007/S002640100277 [ Links ]
25. Prodromidis AD, Charalambous CP. The 6-hour rule for surgical debridement of open tibial fractures: a systematic review and meta-analysis of infection and nonunion rates. J Orthop Trauma. 2016;30:397-402. https://doi.org/10.1097/BOT.0000000000000573 [ Links ]
26. Crowley DJ, Kanakaris NK, Giannoudis PV. Debridement and wound closure of open fractures: the impact of the time factor on infection rates. Injury. 2007;38:879-89. https://doi.org/10.1016/j.injury.2007.01.012 [ Links ]
27. Qiu E, Kurlander DE, Ghaznavi AM. Godina revisited: a systematic review of traumatic lower extremity wound reconstruction timing. J Plast Surg Hand Surg. 2018;52:259-64. https://doi.org/10.1080/2000656X.2018.1470979 [ Links ]
28. Hallock GG. Complications of 100 consecutive local fasciocutaneous flaps. Plast Reconstr Surg. 1991;88:264-68. https://doi.org/10.1097/00006534-199108000-00015 [ Links ]
29. Hallock GG. Lower extremity muscle perforator flaps for lower extremity reconstruction. Plast Reconstr Surg. 2004;114:1123-30. https://doi.org/10.1097/01.prs.0000135847.49178.f2 [ Links ]
30. Karikalan T. Flaps in the management of open tibial fractures. Int J Res Orthop. 2019;5(3):504. https://doi.org/10.18203/ISSN.2455-4510.IntJResOrthop20191792 [ Links ]
Received: February 2023
Accepted: March 2023
Published: November 2023
* Corresponding author: danemaimin@gmail.com
Editor: Dr Luan Nieuwoudt, University of KwaZulu-Natal, Durban, South Africa
Funding: No funding was received for this study.
Conflict of interest: The authors declare they have no conflicts of interest that are directly or indirectly related to the research.














