Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SA Orthopaedic Journal
versão On-line ISSN 2309-8309
versão impressa ISSN 1681-150X
SA orthop. j. vol.22 no.4 Centurion 2023
http://dx.doi.org/10.17159/2309-8309/2023/v22n4a1
PAEDIATRIC ORTHOPAEDICS
Paediatric distal radius fractures: risk factors for redisplacement
Gadi Z EpsteinI; Jacques du ToitI, *; Nando FerreiraI; Marilize C BurgerI; Tonya M EsterhuizenII
IDivision of Orthopaedic Surgery, Department of Surgical Sciences, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
IIDivision of Epidemiology and Biostatistics, Department of Global Health, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
ABSTRACT
BACKGROUND: Redisplacement of paediatric distal radius fractures is a common problem that may require surgical intervention to avoid suboptimal functional outcomes. Several individual risk factors are known to increase the risk for redisplacement. The aim of this study was to explore and evaluate potential risk factors for redisplacement of the distal radius after closed reduction and plaster cast immobilisation.
METHODS: A retrospective cohort study included paediatric patients between the ages of 2 and 14 years who presented with distal radius fractures and underwent closed reduction and plaster cast immobilisation. Data was evaluated for patient-, fracture- and treatment-related risk factors for redisplacement. Predictor variables were individually tested against the outcome of redisplacement using univariate logistic regression analysis. A p-value < 0.2 was used to select variables to take forward into a multivariable model, including categorised risk factors.
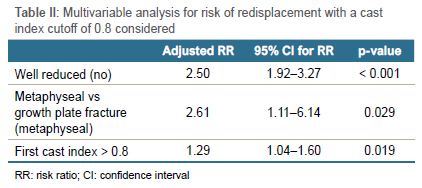
RESULTS: Redisplacement occurred in 40% (n = 59) of the 146 included patients. Independent factors associated with increased risk for redisplacement included: age < 10 years (p = 0.002), sagittal plane angulation < 20° (p = 0114), a first cast index of > 0.8 (p = 0.002), metaphyseal fractures as opposed to growth plate injuries (p < 0.001), the absence of an associated ulna fracture (p = 0.026), and poor initial reduction (p < 0.001). Three independent variables were Anally included into a multivariable model and remained significant risk factors for redisplacement. Poor reduction (risk ratio [RR] 2.5 p < 0.001), metaphyseal fracture location (RR 2.6 p < 0.029), and first cast index > 0.8 (RR 1.3 p < 0.019) collectively influenced the risk of redisplacement.
CONCLUSION: Analysis of risk factors for redisplacement revealed that poor reduction, metaphyseal injuries and a cast index > 0.8 are associated with an increased risk of redisplacement of distal radius fractures in children.
Level of evidence: Level 3
Keywords: trauma, distal radius, fracture, Salter-Harris, redisplacement
Introduction
The anatomy of the distal radius is unique. It is an area of rapid growth and remodelling, but is also vulnerable to fracture.1 Of all forearm fractures in children, approximately 30% occur at the wrist, and distal radius fractures account for 75% of these injuries.2 Despite the tremendous remodelling potential of the distal radius, controversy exists regarding the degree of angulation that is acceptable in the growing child. With increasing age, the degree of acceptable sagittal plane angulation decreases, with recommendations to accept up to 10-15° in children aged 9 to 13 years, and 5-10° in children aged 13 to 15 years.3 Other literature suggested that dorsal angulation deformities of up to 35° will remodel adequately in children that have at least five years of growth remaining.4 However, remodelling does not always occur as predicted, especially in children nearing skeletal maturity.
Various methods of treatment have been used to manage distal radius fractures in children, of which closed reduction and cast immobilisation with or without percutaneous Kirschner wire (K-wire) fixation is the most frequently employed.5,6 The incidence of redisplacement following cast immobilisation is reported as being between 12 and 34%.7,8 Because of this, an increased trend towards K-wire fixation for these injuries has been observed.3,9 A recent meta-analysis revealed that redisplacement of distal radius fractures occurred in only 3.8% of the patients that received K-wire fixation, compared to 45.7% in the closed reduction and casting group.10 Notwithstanding the fact that K-wire fixation reliably decreases redisplacement, this treatment modality has various potential drawbacks and/or complications. K-wire fixation is associated with complications including pin-site infection, neuropraxia, K-wire migration, permanent nerve damage, physeal injury and secondary growth disturbances.11,12 K-wires also need removal after bony union, and although the majority of wires can be removed in the outpatient setting, some wires need removal in theatre under sedation or general anesthaesia.10 Finally, K-wire fixation is also associated with higher costs than cast immobilisation. Crawford et al. reported the costs of K-wire fixation as being almost twice that of cast immobilisation alone (US$8742 vs US$4846).13 However, controversy exists regarding the exact financial implications of cast treatment when considering the costs of treatment of redisplacement.10
Factors leading to redisplacement can be divided into fracture-, patient- and treatment-related factors.14 Known factors leading to redisplacement include: fracture distance from the growth plate, fracture comminution, initial fracture displacement, poor initial fracture reduction, poor casting technique, as well as muscle atrophy and resolution of swelling.14 Many studies have focused on independent risk factors for redisplacement. Procter et al. identified initial displacement and failure to achieve reduction as important predictors of redisplacement.7 Haddad and Williams reported anatomical reduction as an important prognostic factor.8 Casting indices have been extensively studied with a suggestion that a three-point index (a radiographic measurement as an indicator of plaster cast technique) might be predictive of success or failure.14 Evidence suggests that many factors are responsible for the redisplacement of distal radius fractures in children. Unfortunately, risk factors and treatment guidelines are ambiguous regarding the management of distal radius fractures in children.
The aim of this study was to evaluate potential risk factors for redisplacement of the distal radius after closed reduction and plaster cast immobilisation.
Materials and methods
A retrospective cohort study of paediatric patients presenting with distal radius fractures at a Level 1 trauma centre between January 2015 and April 2019 was performed. All patients between the ages of 2 and 14 years, presenting with a fracture of the distal third of the radius that were treated with closed reduction and plaster cast immobilisation, were included. Patients that failed treatment in plaster casts and required K-wire fixation later were also included. Institutional ethics approval as well as hospital board approval was obtained prior to data collection.
Patients presenting with open or pathological fractures, those treated by open reduction and internal fixation or percutaneous K-wire fixation and patients who had poor quality post reduction radiographs were excluded.
Data was collected retrospectively from the hospital notes as well as the institutional Picture Archiving and Communication System (PACS) electronic X-ray database. All radiographs at presentation to the hospital, as well as post-reduction and follow-up, were evaluated. The type of plaster cast used, and the cast placement (i.e., above elbow vs below elbow) were not reliably recorded in the hospital notes and thus not included and reported on in this study.
Recorded information consisted of patient demographics as well as fracture characteristics including side, fracture location, Salter-Harris classification15 where applicable, the presence or absence of dorsal comminution, the presence or absence of an associated ulna fracture, the obliquity of the fracture line on anteroposterior radiograph, and the degree of displacement on the anteroposterior and lateral radiograph. Displacement was quantified in terms of translation and angulation. Translation was quantified as a percentage on anteroposterior and lateral radiographs. The direction of translation to which the fracture displaced was recorded as radial, ulnar, volar or dorsal. Angulation was recorded in degrees in the sagittal plane, i.e. volar or dorsal apex angulation. The presence of rotation was evaluated by differences in the width of the radius and ulna on the anterior-posterior (AP) and lateral radiographs. At initial presentation, the quality of reduction was noted, as well as the casting indices. Given the conflicting definitions that exist with regard to successful reduction,9,11 reduction was considered acceptable for the purposes of the present study if all the following criteria were met:
• < 10° sagittal plane angulation on lateral radiograph
• No angulation AP radiograph
• No rotation
• > 50% apposition of the bony fragments
At each follow-up visit, postreduction radiographs were evaluated for quality of reduction, redisplacement and casting technique using various evidence-based casting indices including: i) the cast index,16 ii) the gap index,17 and iii) the padding index.18
The cast index, proposed by Chess et al.,16 is calculated as the inner diameter of the cast on lateral radiograph divided by the inner diameter of the cast on anteroposterior radiograph at the level of the fracture; a value of < 0.7 is an indication of a well-moulded cast. A cast index of < 0.8 was also measured and recorded based on the study by Kamat et al.19 The gap index, proposed by Malviya et al.,17 is based on the ratio of the gaps in the cast, at the level of the fracture to the inner width of the cast in two planes; the acceptable gap index is < 0.15. The padding index described by Bhatia and Housden18 is calculated as the dorsal gap on lateral divided by the maximum interosseous distance on anteroposterior; the acceptable limit is < 0.3.
At each follow-up visit radiographs were also evaluated for union and fracture alignment. Given the difference in the remodelling potential in children reaching skeletal maturity vs younger children,3 we decided to separate the criteria by age group. Redisplacement was considered to have occurred if any of the following was seen on follow-up X-rays:
• < 9 years: > 15° of sagittal plane angulation, any malrotation, < 50 % apposition on the AP/lateral radiograph
• > 10 years: > 10° of sagittal plane angulation, any malrotation, < 50% apposition on the AP lateral radiograph
The sample was determined using the rule of thumb of ten events per predictor variable considered. Approximately ten predictor variables were considered, thus 100 events were required. Based on the rate of redisplacement, being approximately one-third of fractures, a total of 300 participants were required. After X-ray evaluations were performed, data was analysed using Stata v15. Data was tested for normality. Quantitative predictor variables were individually tested against the outcome of redisplacement of the fracture using an independent t-test while the Mann-Whitney U test was used for non-normally distributed data. A chi-squared test was used to detect associations between categorical predictors and the outcome of redisplacement. A p-value of < 0.2 was used to select independent variables to take forward into a multivariable log binomial model. The model was specified with a log link to produce relative risk estimates and 95% confidence intervals. Age was categorised into those younger than 10 versus 10 years and older, saggital plane angulation on presenting X-rays was categorised into < 20° versus > 20°, while the first cast index was grouped into those < 0.8 versus 0.8 and above. A backward stepwise selection method was used in conjunction with likelihood ratio testing to determine a final log binomial regression model which included only predictors with p-values < 0.05.
Results
Of the 300 potential participants initially screened for inclusion, 154 were excluded due to treatment with K-wire fixation, inability to accurately analyse the radiographs, poor follow-up, or lack of confirmation of the outcome. The final cohort included 112 male (77%) and 34 female (23%) patients with a mean age of 9.5 ± 2.9 years (95% CI 9.0-9.9).
Redisplacement occurred in 59 patients (40%), a median of 13.0 days (interquartile range [IQR] 7.0-22.0) after initial treatment. Patients with redisplaced fractures were significantly younger (8.6 ± 3.0 years) compared to those that did not redisplace (10.0 ± 2.7, p = 0.002) Other factors associated with increased risk for redisplacement include: fracture displacement on initial X-rays prior to reduction with sagittal plane angulation of < 20° (p = 0114); a first cast index of > 0.8 (p = 0.002); metaphyseal fractures as opposed to growth plate injuries (p < 0.001); the absence of an associated ulna fracture (p = 0.026); and a poor initial reduction (p < 0.001) (Table I).
Univariate log binomial regression analysis with categorised variables identified six associations (Table I) which were carried forward into the multivariable model. Three independent multivariable predictors remained in the model to predict risk of redisplacement, when a cast index of 0.8 was considered (Table II). The final accepted equation was where a fracture that was not well reduced, was metaphyseal and had a first cast index of > 0.8 increased the risk of redisplacement. Risk of redisplacement
= 0.918 (not well reduced) + 0.958 (metaphyseal)
+ 0.257 (first cast index > 0.8) - 2.0
More specifically, not reducing the fracture sufficiently initially increased the risk of redisplacement 2.5 times while a metaphyseal fracture increased the risk by 2.6 times. The risk of redisplacement in patients with a first cast index of > 0.8 was 1.3 times greater compared to those with a first cast index of < 0.8 (Table II). When considering a cast index cutoff value of 0.7, two multivariable predictors remained in the model to predict risk of redisplacement including whether the fracture was well reduced initially and whether the fracture was classified as being metaphyseal (data not presented).
Discussion
The aim of this study was to evaluate risk factors for redisplacement of distal radius fractures in children, to possibly predict redisplacement with more precision. Patients at increased risk of redisplacement are potential candidates for closed reduction and K-wire fixation as the initial treatment modality of choice.
The risk factors associated with redisplacement of distal radius fractures in children include patient-specific factors, fracture-related factors as well as treatment-related factors.14 The first main finding of our study was that the location of the fracture, the quality of the initial reduction, and the first cast index can be used in a multivariable model to predict the risk of redisplacement. No patient-specific factors were associated with increased risk of redisplacement following the multivariable regression analysis, and the only fracture-related factor included in the multivariable model was fracture location. This study illustrates that metaphyseal fractures have a 2.6 times higher risk for redisplacement versus physeal fractures. This fracture-related risk is supported in the literature.20
Treatment-related factors included poor reduction at the initial treatment as well as the first cast index. Poor initial reduction was associated with a 2.5 times increased risk for redisplacement, while a first cast index > 0.8 illustrated a 1.3 times increased risk for redisplacement, with other factors held constant. These findings were similarly reported by Zamzam et al. and Proctor et al.5,7 Two independent cast index cutoff values were used in the current study. Chess et al. originally described the cutoff value for the cast index as being 0.7,16 while a cutoff of 0.8 has been suggested by Kamat et al.19 as the optimum threshold. Therefore, both cast index cutoff values, 0.7 and 0.8, were considered in this study. A value of > 0.8 was a stronger predictor of redisplacement in our study. Several studies have reported on which casting index is the better predictor of redisplacement; however, controversy still exists.17,20 In the current study, the padding and gap indices were also considered, but the only predictor of redisplacement of the indices used was the cast index. In addition to this, the cast index was a much simpler index to measure. A recent study by Ravier et al. argued that the cast index, unlike other indices, is a simple ratio, easily measured on radiographs, with a high intra-rater and inter-rater reliability.21
Three other factors investigated in the current study could be used independently to predict redisplacement, being age, fracture displacement (angulation) on the lateral radiograph, and ulna involvement. Age, although it cannot be controlled, is associated with an increased risk for redisplacement in children younger than 10 years, if considered independently. Redisplacement in children so young does not usually change clinical practice as the remodelling potential in this age group is so great. The association with age, however, remains an interesting observation, considering that clinicians tend to be more cautious with children over the age of 10 years due to their decreased remodelling potential.3,4 Despite the great remodelling potential children in children under 10 years of age, the exact amount of displacement that is considered acceptable is still being investigated.2 Fracture displacement and ulna involvement were independently associated with an increased risk of redisplacement. Greater displacement has previously been shown to be an increased risk factor for redisplacement.5 However, the current series found sagittal plane angulation of less than 20° was associated with an increased risk for redisplacement. A possible explanation for this could be that radiographs with angulations of less than 20° were possibly not reduced since they might have been considered to be acceptable deformities. This, combined with our strict definition of redisplacement, would categorise these children into the redisplaced group. This is, therefore, a recognised limitation of the current study. This study reports that an associated ulna fracture did not increase the risk for redisplacement. The role of an associated ulna fracture is controversial in the literature. Gibbons et al.22 observed that an intact ulna is a risk for redisplacement whereas Zamzam et al.5 observed that the presence of an ulna fracture was a significant risk factor for redisplacement. McLauchlin et al. showed that an intact ulna had no influence on outcome.23
Treatment-related factors that did not influence the risk for redisplacement included the padding index and gap index. Several studies have proposed other indices to be of value in predicting redisplacement.17,20 Specific indices such as the three-point index, Canterbury and padding index have shown good inter- and intraobserver reliability; however, there is disparity in the literature.17,20,24 Although inter- and intraobserver reliability were not considered in the current study, previous investigations by Williams et al.24 and more recently Ravier et al.,21 suggested that the casting index is a simple ratio, easy to calculate and has a high intra- and interobserver relationship.
Despite our findings, this study has several limitations. This is a retrospective study and the sample of patients was determined by the availability of cases complying with the inclusion criteria. Radiological measurements were performed only once for each radiograph so the presence of inter-rater or intra-rater reliability was not considered. Lateral angulation of < 20° was found to be a risk factor for redisplacement which is unusual and contradicts the literature. Future prospective studies with larger sample sizes and randomisation would provide better evidence.
Conclusion
Redisplacement of paediatric distal radius fractures remains a common problem facing clinicians. A metaphyseal fracture location, first cast index of greater than 0.8, and poor initial reduction were all associated with increased risk of redisplacement. These risk factors can be used to guide clinical decision-making processes to determine initial treatment approaches in order to potentially decrease the prevalence of redisplacement.
Acknowledgements
We acknowledge and extend our sincere gratitude to Mr Ben Wiese who assisted with data collection.
Ethics statement
The authors declare that this submission is in accordance with the principles laid down by the Responsible Research Publication Position Statements as developed at the 2nd World Conference on Research Integrity in Singapore, 2010. Prior to commencement of the study, ethical approval was obtained from the Stellenbosch University Ethics Committee, HREC reference number: S17/10/262. All procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Informed consent was not required due to the retrospective nature of the study and the deidentification of data.
Declaration
The authors declare authorship of this article and that they have followed sound scientific research practice. This research is original and does not transgress plagiarism policies.
Author contributions
GZE: study conceptualisation, data capture, data analysis, manuscript preparation, manuscript revision, approval of final manuscript
JdT: study conceptualisation, data analysis, manuscript preparation, approval of final manuscript
NF: manuscript preparation, approval of final manuscript
MCB: data analysis, design of testing set up, manuscript preparation, manuscript revision, approval of final manuscript
TME: data analysis, manuscript preparation, approval of final manuscript
ORCID
Epstein GZ https://orcid.org/0000-0002-4753-5024
Du Toit J https://orcid.org/0000-0002-0958-5450
Ferreira N https://orcid.org/0000-0002-0567-3373
Burger MC https://orcid.org/0000-0003-2831-4960
Esterhuizen TM https://orcid.org/0000-0002-8703-1664
References
1. Herring JA. Tachdjian's Pediatric Orthopaedic from the Texas Scottish Rite Hospital for Children. In: 5th ed. Philadelphia: Elsevier Saunders; 2014. pp. 1326-47. [ Links ]
2. Sharma S, Bowe D, Walters SJ, Flowers MJ. Dorsal cortical comminution as a predictor of redisplacement of distal radius fractures in children. Injury. 2011;42(2):173-77. http://dx.doi.org/10.1016/j.injury.2010.07.409 [ Links ]
3. Hove LM, Brudvik C. Displaced paediatric fractures of the distal radius. Arch Orthop Trauma Surg. 2008;128:55-60. http//dx.doi.org/10.1007/s00402-007-0473-x [ Links ]
4. Roth KC, Denk K, Colaris JW, Jaarsma RL. Think twice before re-manipulating distal metaphyseal forearm fractures in children. Arch Orthop Trauma Surg. 2014;1699-707. http//dx.org/10.1007/s00402-014-2091-8 [ Links ] Arial, Helvetica, sans-serif" size="2">5. Zamzam MM, Khoshhal KI. Displaced fracture of the distal radius in children. J Bone Jt Surg - Ser B. 2005;87(6):841-43. http//dx.org/10.1302/0301-620X.87B6 [ Links ]
6. Rodríguez-Merchan EC. Pediatric fractures of the forearm. Clin Orthop Relat Res. 2005 Mar 1;432:65-72. https://doi:10.1097/01.blo.0000156480.76450.04 [ Links ]
7. Proctor MT, Moore DJ, Paterson JMH. Redisplacment after manipulation of distal radial fractures in children. J Bone Jt Surg - Ser B. 1993. https://doi.org/10.1302/0301-620X/75B3.8496221 [ Links ]
8. Haddad FS, Williams RL. Forearm fractures redisplacement. Science (80- ). 1995;26(10):691-92. https://doi.org/10.1016/0020-1383(95)00136-0 [ Links ]
9. Miller BS, Taylor B, Widmann RF, et al. Cast immobilization versus percutaneous pin fixation of displaced distal radius fractures in children: A prospective, randomized study. J Pediatr Orthop. 2005;25(4):490-94. https://doi.org/10.1097/01.bpo.0000158780.52849.39 [ Links ]
10. Sengab A, Krijnen P, Schipper IB. Displaced distal radius fractures in children, cast alone vs additional K-wire fixation: a meta-analysis. Eur J Trauma Emerg Surg [Internet]. 2019;45(6):1003-11. http://dx.doi.org/10.1007/s00068-018-1011-y [ Links ]
11. Colaris JW, Allema JH, Biter LU, et al. Re-displacement of stable distal both-bone forearm fractures in children: A randomised controlled multicentre trial. Injury [Internet]. 2013;44(4):498-503. http://dx.doi.org/10.1016/j.injury.2012.11.001 [ Links ]
12. Boyden EM, Peterson HA. Partial premature closure of the distal radial physis associated with Kirschner wire fixation. Orthopedics. 1991;14(5):585-88. https://doi.org/10.3928/0147-7447-19910501-13 [ Links ]
13. Crawford SN, Lee LSK, Izuka BH. Closed treatment of overriding distal radial fractures without reduction in children. J Bone Joint Surg Am. 2012;94(3):246-52. https://doi:10.2106/JBJS.K.00163 [ Links ]
14. Pretell Mazzini J, Rodriguez Martin J. Paediatric forearm and distal radius fractures: Risk factors and re-displacement-role of casting indices. Int Orthop. 2010;34(3):407-12. https://doi:10.1007/s00264-009-0904-0 [ Links ]
15. Salter RB, Harris WR. JBJS classics: Injuries involving the epiphyseal plate. J Bone Joint Surg Am. 2001;83(11):1753. [ Links ]
16. Chess DG, Hyndman JC, Leahey JL, Brown DC, Sinclair AM. Short arm plaster cast for distal pediatric forearm fractures. J Pediatr Orthop. 1994;14(2):211-13. https://doi:10.1097/01241398-199403000-00015 [ Links ]
17. Malviya A, Tsintzas D, Mahawar K, et al. Gap index: A good predictor of failure of plaster cast in distal third radius fractures. J Pediatr Orthop Part B. 2007;16(1):48-52. https://doi:10.1097/01.bpb.0000236232.57269.ec [ Links ]
18. Bhatia M, Housden PH, Hospitals EK. Redisplacement of paediatric forearm fractures : Role of plaster moulding and padding. Injury. 2006;259-268. https://doi.org/10.1016/j.injury.2005.10.002 [ Links ]
19. Kamat AS, Pierse N, Devane P, et al. Redefining the cast index: The optimum technique to reduce redisplacement in pediatric distal forearm fractures. J Pediatr Orthop. 2012;32(8):787-91. https://doi:10.1097/BPO.0b013e318272474d [ Links ]
20. Alemdaroglu KB, Ilter S, Çimen O, et al. Risk factors in redisplacement of distal radial fractures in children. J Bone Joint Surg Am. 2008;90(6):1224-30. https://doi:10.2106/JBJS.G.00624 [ Links ]
21. Ravier D, Morelli I, Buscarino V, et al. Plaster cast treatment for distal forearm fracturesin children. J Pediatr Orthop B. 2020;29(2):179-86. https://doi:10.1097/BPB.0000000000000678 [ Links ]
22. Gibbons CL, Woods DA, Pailthorpe C, et al. The management of isolated distal radius fractures in children. J Pediatr Orthop. 1994;14(2):207-10. doi:10.1097/01241398-199403000-00014. https://doi:10.1097/01241398-199403000-00014 [ Links ]
23. McLauchlan GJ, Cowan B, Annan IH, Robb JE. Management of completely displaced metaphyseal fractures of the distal radius in children. A prospective, randomised controlled trial. J Bone Joint Surg Br. 2002;84(3):413-17. https://doi.org/10.1302/0301-620X.84B3.0840413 [ Links ]
24. Williams ND, Rush JK, Schmitz MR, Johnson AE. Reliability of casting indices among members of an orthopaedic surgery residency. J Paediatr Orthop. 2017 Jun 1;37(4):e238-42. https://doi.org/10.1097/BPO.0000000000000908 [ Links ]
Received: February 2023
Accepted: May 2023
Published: November 2023
* Corresponding author: jdtt@sun.ac.za
Editor: Dr Greg Firth, Royal London Hospital, London, England
Funding: No funding was received for this study.
Conflict of interest: The authors declare they have no conflicts of interest that are directly or indirectly related to the research.