Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SA Orthopaedic Journal
versión On-line ISSN 2309-8309
versión impresa ISSN 1681-150X
SA orthop. j. vol.22 no.2 Centurion 2023
http://dx.doi.org/10.17159/2309-8309/2023/v22n2a3
SURGICAL TECHNIQUE TRAUMA AND GENERAL ORTHOPAEDICS
The Bridging Infix: a modified, minimally invasive subcutaneous anterior pelvic fixation technique
Sven StrydomI, *; Christian H SnyckersII
IDepartment of Orthopaedics, University of Pretoria, Kalafong Tertiary Hospital, Pretoria, South Africa
IIPrivate Practice, Eugene Marais Hospital, Pretoria, South Africa
ABSTRACT
Various methods for anterior pelvic ring fixation have been described in the literature, each with specific advantages and disadvantages. We describe a modified minimally invasive subcutaneous technique for anterior fixation: the Bridging Infix.
It combines the benefits of internal plate fixation with external fixator principles. We merged and modified features of the existing INFIX and Pelvic Bridge techniques during the design. Similar to these techniques, we use plate-rods typically used during occipitocervical fusions. The design changes allow for less discomfort due to prominent hardware in thin patients and eliminate the need for an intact medial pubic rami for fixation. There is also no risk of bladder injury due to accidental screw perforation through the pubic rami.
The Bridging Infix is ideal for patients who are physiologically too frail for extensive open reduction and plate osteosynthesis, such as elderly patients with pelvic fragility fractures who are failing to mobilise due to pain. It can also be used for patients in whom external fixators may be impractical or poorly tolerated, such as obese patients or those with increased nursing demands. This technique does not provide adequate posterior pelvic ring stability, thus it requires an intact posterior tension band or the addition of separate posterior fixation.
Patients can commence in-bed mobilisation the same day as the procedure, with weight-bearing as tolerated allowed for most cases, and toe-touching reserved for highly unstable injury patterns only. The implants are not routinely removed unless requested by the patient, especially in the elderly to avoid additional anaesthetic exposure. Potential complaints include lateral thigh pain, due to lateral femoral nerve compression, and mechanical discomfort during exercise activities.
Level of evidence: Level 5
Keywords: anterior pelvic fixation, minimally invasive, elderly, pelvic fragility fracture, anterior column fracture
Introduction
Early treatment with appropriate surgery for complex or unstable pelvic fractures is essential. Transiliac/sacral screw fixation is an effective treatment for most posterior injuries. At the same time, stabilisation with external fixation, open reduction and internal fixation with submuscular plating (ORIF), retrograde pubic rami screw fixation, or newer subcutaneous techniques are possible for anterior instability.1 External fixation, being a minimally invasive technique, serves to preserve the fracture site's biology and allows for easy removal.2 Despite its convenience for the surgeon, it is often unsightly and cumbersome for the patient and has an associated complication rate as high as 62%.3,4 The most significant benefits of ORIF include allowing for anatomic reduction and no need for removal of any implants at a later stage. It also remains biomechanically the most rigid construct at the symphysis pubis.5,6 Despite these advantages, ORIF is associated with a high surgical morbidity rate.4 Retrograde pubic rami screw fixation has grown in popularity because it provides a minimally invasive internal fixation option. These screws are, however, not suitable for all fracture types and have a reported loss of reduction in 15% of cases, with advanced age and female sex being major predictors of failure.7 These drawbacks have led to the development of newer subcutaneous fixation techniques.
The application of minimally invasive subcutaneous fixation requires minimal soft tissue dissection, which reduces operating time, intraoperative blood loss and length of stay when compared to ORIF.2,4,8 The subcutaneous location also decreases the risk of surgical site infection, eases the burden of nursing care, and avoids interference with rehabilitation and daily activities.2,3,8 We propose using a modified internal bridge plate-and-rod technique, which combines the extra-pelvic fixation methods of an external fixator with the low profile advantages of the pelvic bridge and ORIF. Successful use of the Bridging Infix technique was first described by Strydom and Snyckers.9 The aim is to limit complications associated with external fixator use, while retaining the advantages of using internal implants, but using the same external fixation principles.2,3,10 Our technique also aims to reduce the described complications of other minimally invasive subcutaneous fixation methods, such as lateral cutaneous femoral nerve (LCFN) neuropraxia, heterotopic ossification and patient discomfort.
Indications and contraindications
As this technique is a modification of existing constructs, some of the indications and contraindications are similar. We do, however, include additional indications where use of the Bridging Infix may be preferred.
Indications
• Unstable pelvic ring injuries with an isolated anterior fracture, with an intact posterior tension band
• To enhance anterior stability after adequate posterior fixation
• Elderly or frail patients with fragility fractures of the pelvis who are unable to mobilise due to pain; failed conservative management trial
• Obese patients
• Minimally invasive anterior pelvis fixation when open reduction and internal fixation is contraindicated
• Patients with increased nursing demands, i.e., ICU patients, where external fixators may impede nursing care
• Thin patients in whom the pedicle screws of the INFIX may cause irritation/discomfort
• Medial pubic rami fractures, which limits medial fixation for the Pelvic Bridge
Contraindications
• Iliac wing dissociation or pubic symphysis diastasis (purely ligamentous injuries)
• Degloving wounds or open fractures over the iliac crest
• Open pelvic injuries with peritoneal contamination
• Haemodynamically unstable patients requiring rapid pelvis stabilisation
• Used in isolation for combined anterior and posterior instability
Surgical technique
Preoperative planning
Fixation of posterior instability should be prioritised; the options available will not be discussed in this article and are left to each surgeon's discretion. We recommend including a computed tomography (CT) scan of the pelvis in the workup, due to the large number of posterior injuries missed on plain radiographs alone.
It is important to take both the patient's physiological status and radiological findings into consideration when choosing the appropriate management. Elderly patients with fragility fractures can first undergo a two- to three-day trial of conservative management involving adequate analgesia and physiotherapy, to determine if surgery is required.
Patient positioning and draping
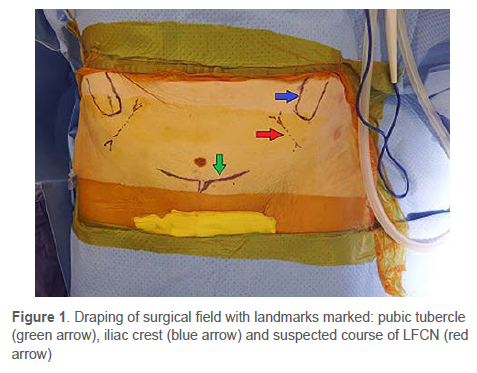
The patient is positioned supine and centrally on a radiolucent table. The patient's arms should be placed on arm boards and abducted no more than 90°, to allow entry for the C-arm. Confirm that adequate fluoroscopic images can be acquired before draping the patient. Prepare and drape the surgical field, ensuring adequate access to the iliac crest and pubic symphysis for the Bridging Infix, as well as adequate access to allow for the chosen posterior fixation. Shave the pubic region as needed and isolate the groin with an occlusive dressing. A surgical marker can be used to mark the relevant landmarks (Figure 1).
Approach
The incisions for the lateral windows are made from the anterior superior iliac spine (ASIS), extending 4 cm proximally along the crest. Both a scalpel and cautery are used to dissect down to the external oblique fascia. The musculature is carefully elevated directly off the crest to create a bare area for fixation. A third horizontal incision of 6-8 cm is made centrally, approximately 1 cm superior to the pubic symphysis, similar to a Pfannenstiel incision. The scalpel or cautery is used to dissect down to the rectus abdominis fascia, to complete the middle window.
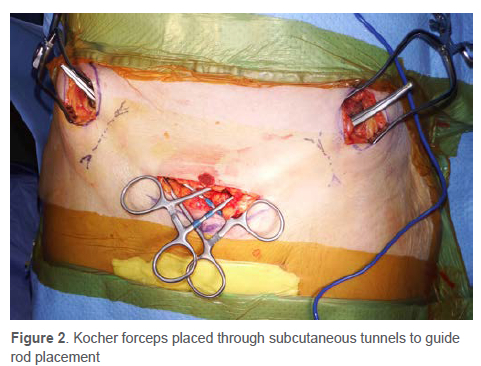
A subcutaneous tunnel is then made between the medial and two lateral windows by passing a curved Kocher forceps to bluntly dissect through the tissue. Care must be taken to pass the forceps superficial and parallel to the inguinal ligament and to create only a single tunnel. Each tunnel can be made from either the lateral or middle window. Digital palpation of the tunnel can assist with identifying fascial tears which are a cause of concern. Dissection is complete once the forceps can easily pass between windows. The Kocher forceps are placed from the middle to the lateral window (Figure 2) to later guide and pull the plate-rod through the tunnel.
Contouring the construct
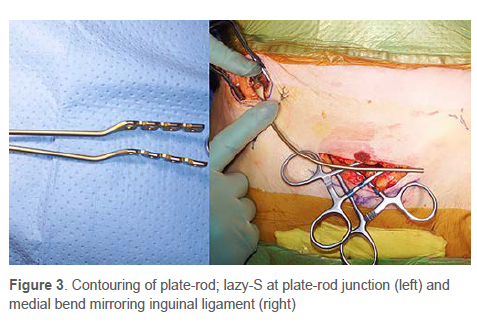
Instrumentation used is the 4 mm plate-rod construct used in occipital cervical fusion, with a 6 mm straight rod and two rod-to-rod clamps. Contouring the plate-rod is patient specific, but the basic principles remain the same. The plate is gently bent, using spinal rod benders, to lie passively on the iliac crest. The second contour is a lazy-S bend at the plate-rod junction. Lastly the rod portion is then bent medially to align superiorly with the inguinal ligament, without compressing it, with the distal portion lying parallel and 1 cm superior to the pubic symphysis (Figure 3). A templating plate-rod can be used to assist with contouring the implant.
Placing the construct
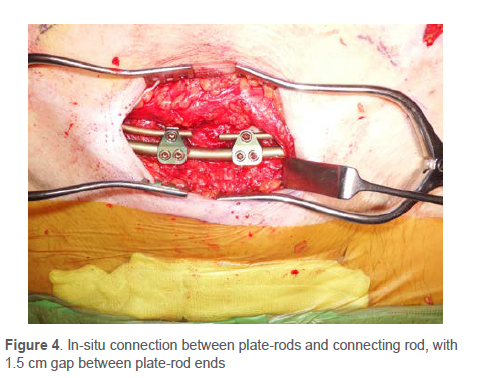
The tip of the rod is clamped with the Kocher and gently pulled from the lateral to the medial window. Care must be taken not to force the rod through, as this can result in neurovascular complications. Both direct visualisation and fluoroscopy should be used to assess the adequacy of the plate-rod construct contour. Remove the plate-rod if significant additional contouring is required, while in-situ rod benders can be used to make minor correction to the contour with the construct in-situ. Placing a single temporary screw in the plate section can assist with assessing the plate positioning before definitive fixation is done. The rod ends are cut to allow a 1.5 cm gap between the two rod ends. Definitive fixation is done once the rod-plate construct is positioned satisfactorily. We use a 50 mm, 45 mm and a 40 mm cortical 3.5 mm screw (from proximal to distal) as standard screw lengths on each side; however, longer sizes can be used if the pelvis morphology allows. Fluoroscopy should be used to access screw position using views both parallel and perpendicular to the iliac wing. A 6 mm connector rod is connected to each plate-rod with rod-to-rod connectors (Figure 4).
Fracture reduction
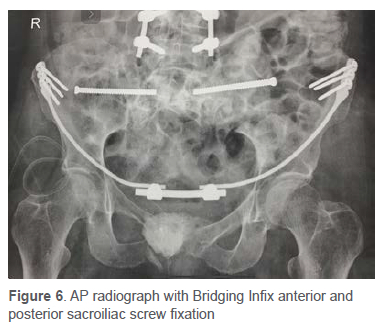
Posterior unstable injuries should be reduced and stabilised before anterior fixation is done. The aim of the reduction is to achieve a position as close to anatomic as possible to facilitate proper fracture healing. Various methods are available to assist with reduction. Rotational and vertical translation can be reduced using Schanz pins in the crest, placed just posterior to the plate, as joysticks to control each hemi-pelvis. A distal femoral traction pin can be used for vertical misalignment that is resistant to manipulation with the Schanz pins. Final fracture reduction can often be adequately reduced by using the connecting rod to compress or distract the anterior pelvis. The connecting rod is secured to the tip of one platerod, while the connector to the other plate-rod is applied loosely. Distraction or compression instruments are then used to reduce the anterior pelvis (Figure 5), before securing the second rod-to-rod connector. Fracture reduction and final construct positioning is confirmed with intraoperative fluoroscopy and postoperative radiographs, using anterior-posterior (Figure 6), inlet and outlet views.
Wound closure
The wounds are irrigated with 0.9% saline solution and haemostasis is reconfirmed. Although we do not make routine use of drains, a drain can be inserted at the surgeon's discretion. Additionally, a gentamycin-impregnated collagen sponge should be placed over the connecting rod and connectors in the middle window, if available. Closure is done in layers, with number 2.0 Vicryl (Ethicon) used for dead space and subcutaneous tissue and number 3.0 Monocryl (Ethicon) for the subcuticular layer. The wounds are then sealed with Dermabond (Ethicon) and a transparent occlusive dressing.
Rehabilitation
The goal of this procedure is to allow early mobilisation. Physiotherapy can be started the same day as the procedure, beginning with in-bed mobilisation. Patients are encouraged to weight-bear as tolerated but can remain toe-touch weight-bearing for the first six weeks in highly unstable pelvic injuries or depending on the modality of posterior fixation chosen. There are no restrictions to hip motion post surgery.
Discussion
Minimally invasive anterior fixation is gaining appeal, especially for elderly patients with osteoporotic bone, as it provides rapid pain relief and allows for early mobilisation.2,11 Their application requires minimal soft tissue dissection, which reduces operating time, intraoperative blood loss, and length of stay when compared to ORIF.2,4,8 The subcutaneous location also decreases the risk of surgical site infection, eases the burden of nursing care, and avoids interference with rehabilitation and daily activities.2,3,8
The INFIX was the first of these minimally invasive fixation techniques to be described by Vaidya et al.12 A cadaver study by Reichel et al., however, noted several challenges with its application.13 First, its application was variable and highly dependent on the pedicle screw's placement and curvature of the rod, which results in an increased risk of impingement due to the patient's body habitus or when greater flexion is attempted at the waist. Since the connecting rod did not mirror static anatomic structures, there also remained the risk of the rod twisting or being misplaced while securing the locking caps. Lastly the pedicle screw depth is a subjective measure as it lies several centimetres above the bone; placement at the incorrect depth can lead to either impingement of underlying structures or patient discomfort from prominent hardware, especially in thin patients. One of the most common complications is impingement of the LFCN; neuropraxia was noted to be as high as 55-57% of cases.14,15
The Pelvic Bridge was described more recently by Hiesterman et al. in an attempt to improve on the INFIX.16 Its anatomical course followed static anatomic landmarks, which reduced the risk of misapplying the construct and impinging neurovascular structures.13 Reichel et al. found greater safety margins from the LFCN when compared to the INFIX.13 They did, however, note a theoretical risk of bladder injury with erroneous drilling and screw placement into the pubic symphysis. Another potential drawback is the inability to get adequate medial screw purchase if the pubic rami fracture involves the Nakatani zone I. Fractures in this zone accounted for 15% of the fractures in the study by Starr et al.7
Biomechanically these constructs provide sufficiently rigid fracture fixation to facilitate bone healing, with several studies conclusively demonstrating superior stiffness at the pubic symphysis compared to external fixators.2,5
This 'Bridging Infix' technique described above, and used by Strydom and Snyckers, is a modification of both the abovementioned techniques and we propose that it can be used as an alternative anterior fixation method in an attempt to address the potential complications and drawbacks described.9 It follows the same anatomical course as the Pelvic Bridge, hence should have a similar incidence of LFCN neuropraxia. The lack of medial fixation negates the risk of bladder injury with screw placement and allows for its application in patients with Nakatani zone I fractures.
A potential drawback to our technique is one shared with the other anterior fixation techniques mentioned, in that surgical removal may be required. This is simply because the long-term consequences of leaving the hardware in-situ are unknown in the literature. In our practice however, we only remove the hardware if the patient complains of persistent discomfort or presents with a complication such as LFCN neuropraxia. This practice is mainly to avoid additional surgery, especially in elderly patients. We can report that very few patients who received this fixation desired removal at the one-year follow-up. Another theoretic drawback is due to the modification which forgoes the medial fixation; this increases the lever arm between the lateral fixation points compared to other subcutaneous techniques. This has the potential to decrease the overall stability of the construct. Considering that some physiological movement does occur at the pubic symphysis, this can explain why a less rigid construct still provides adequate stability to allow union.
Conclusion
The Bridging Infix is a technique through which anterior pelvic fixation can be achieved. Its minimally invasive approach makes it an especially attractive option to consider in the elderly population. With this technique, we have built upon and modified previously described minimally invasive techniques, in order to expand potential indications and limit the occurrence of some of the described complications.
Ethics statement
The authors declare that this submission is in accordance with the principles laid down by the Responsible Research Publication Position Statements as developed at the 2nd World Conference on Research Integrity in Singapore, 2010. Formal written consent was obtained from the patient for the use of radiographs and clinical photos (available on request).
Declaration
The authors declare authorship of this article and that they have followed sound scientific research practice. This research is original and does not transgress plagiarism policies.
Author contributions
SS: contributed to technique development and manuscript preparation CS: contributed to conceptualisation, patient treatment, technique development and manuscript preparation
ORCID
Strydom S https://orcid.org/0000-0002-6288-4388
Snyckers CH https://orcid.org/0000-0002-6297-894X
References
1. Oberkircher L, Ruchholtz S, Rommens P, et al. Osteoporotic pelvic fractures. Dtsch Arztebl Int. 2018;115(5):70-80. https://dx.doi.org/10.3238/arztebl.2018.0070 [ Links ]
2. Cole P, Dyskin E, Gilbertson J. Minimally invasive fixation for anterior pelvic ring disruptions. Injury. 2015;46(S3):S27-34. https://dx.doi.org/10.1016/S0020-1383(15)30008-5 [ Links ]
3. Vaidya R, Kubiak E, Bergin P, et al. Complications of anterior subcutaneous internal fixation for unstable pelvis fractures: A multicenter study. Clin Orthop Relat Res. 2012;470(8):2124-31. https://dx.doi.org/10.1007/s11999-011-2233-z [ Links ]
4. Steer R, Balendra G, Matthews J, et al. The use of anterior subcutaneous internal fixation (INFIX) for treatment of pelvic ring injuries in major trauma patients, complications and outcomes. SICOT J. 2019;5:22. https://dx.doi.org/10.1051/sicotj/2019019 [ Links ]
5. Vigdorchik J, Esquivel A, Jin X, et al. Biomechanical stability of a supra-acetabular pedicle screw internal fixation device (INFIX) vs external fixation and plates for vertically unstable pelvic fractures. J Orthop Surg Res. 2012;7(1):31. https://dx.doi.org/10.1186/1749-799X-7-31 [ Links ]
6. Vaidya R, Woodbury D, Nasr K. Anterior subcutaneous internal pelvic fixation/INFIX: A systematic review. J Orthop Trauma. 2018;32(S6):S24-30. https://dx.doi.org/10.1097/BOT.0000000000001248 [ Links ]
7. Starr A, Nakatani T, Reinert C, Cederberg K. Superior pubic ramus fractures fixed with percutaneous screws: What predicts fixation failure? J Orthop Trauma. 2008;22(2):81-87. https://dx.doi.org/10.1097/BOT.0b013e318162ab6e [ Links ]
8. Scheyerer M, Zimmermann S, Osterhoff G, et al. Anterior subcutaneous internal fixation for treatment of unstable pelvic fractures. BMC Res Notes. 2014;7:133. https://dx.doi.org/10.1186/1756-0500-7-133 [ Links ]
9. Strydom S, Snyckers CH. Minimally invasive subcutaneous anterior fixation of pelvic fractures in the elderly: case report and literature review. SA Orthop J 2021;20(4):240-45. http://dx.doi.org/10.17159/2309-8309/2021/v20n4aXXX [ Links ]
10. Yin Y, Luo J, Zhang R, et al. Anterior subcutaneous internal fixator (INFIX) versus plate fixation for pelvic anterior ring fracture. Sci Rep. 2019;9(1). https://dx.doi.org/10.1038/s41598-019-39068-7 [ Links ]
11. Cole P, Hesse D, Dugarte A, Dyskin E. The Pelvic Bridge. JBJS Essent Surg Tech. 2017;7(3):e20. https://dx.doi.org/10.2106/JBJS.ST.15.00085 [ Links ]
12. Vaidya R, Colen R, Vigdorchik J, et al. Treatment of unstable pelvic ring injuries with an internal anterior fixator and posterior fixation: Initial clinical series. J Orthop Trauma. 2012;26(1):1-8. https://dx.doi.org/10.1097/BOT.0b013e318233b8a7 [ Links ]
13. Reichel L, MacCormick L, Dugarte A, et al. Minimally invasive anterior pelvic internal fixation: An anatomic study comparing Pelvic Bridge to INFIX. Injury. 2018;49(2):309-14. https://dx.doi.org/10.1016/j.injury.2017.12.009 [ Links ]
14. Dahill M, McArthur J, Roberts G, et al. The use of an anterior pelvic internal fixator to treat disruptions of the anterior pelvic ring. Bone Joint J. 2017;99-B(9):1232-36. https://dx.doi.org/10.1302/0301-620X.99B9.BJJ-2016-1025.R2 [ Links ]
15. Hoskins W, Bucknill A, Wong J, et al. A prospective case series for a minimally invasive internal fixation device for anterior pelvic ring fractures. J Orthop Surg Res. 2016;11(1):135.https://dx.doi.org/10.1186/s13018-016-0468-9 [ Links ]
16. Hiesterman T, Hill B, Cole P. Surgical technique: A percutaneous method of subcutaneous fixation for the anterior pelvic ring: The Pelvic Bridge. Clin Orthop Relat Res. 2012;470(8):2116-23. https://dx.doi.org/10.1007/s11999-012-2341-4 [ Links ]
Received: September 2022
Accepted: January 2023
Published: May 2023
* Corresponding author: svenstrydom@gmail.com
Editor: Prof. Sithombo Maqungo, University of Cape Town, Cape Town
Funding: No funding was received for this study.
Conflict of interest: The authors declare they have no conflicts of interest that are directly or indirectly related to the research.














