Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SA Orthopaedic Journal
versión On-line ISSN 2309-8309
versión impresa ISSN 1681-150X
SA orthop. j. vol.22 no.2 Centurion 2023
http://dx.doi.org/10.17159/2309-8309/2023/v22n2a1
TRAUMA AND GENERAL ORTHOPAEDICS
Complications of surgically managed pelvic and acetabular fractures
Sandile T MbathaI, *; Mlekeleli TN DumaI; Sithombo MaqungoII; Leonard C MaraisIII
IDepartment of Orthopaedic Surgery, Grey's Hospital, School of Clinical Medicine, University of KwaZulu-Natal, South Africa
IIOrthopaedic Trauma Division of Orthopaedic Surgery, Groote Schuur Hospital, University of Cape Town, South Africa
IIIDepartment of Orthopaedic Surgery, School of Clinical Medicine, University of KwaZulu-Natal, South Africa
ABSTRACT
BACKGROUND: High energy pelvic and acetabular fractures frequently occur in conjunction with multiple system injuries and have been associated with morbidity and mortality. We aimed to identify the risk factors associated with complications in patients with pelvic and/or acetabular fractures treated surgically in a resource-constrained clinical setting.
METHODS: We performed a retrospective review of adult patients younger than 65 years treated surgically over a three-year period at a tertiary and regional hospitals in South Africa. Epidemiological data as well as trauma-, fracture- and treatment-related factors were compared in patients who developed complications and those who did not, at a mean follow-up of ten months (interquartile range 4-14 months; range 0-31.
RESULTS: Eighty-eight patients were included. Complications were encountered in 41% of the cohort. Factors associated with adverse events were age above 35 years (p = 0.008); transverse sacral fractures (p = 0.008); partial articular acetabular fractures with isolated column and/or wall involvement (p = 0.014); Kocher-Langenbeck approach (p = 0.001); posterior acetabular wall fixation (p = 0.002); fixation with plate and screws (p = 0.012); and follow-up period more than 6 months (p = 0.025). Complications encountered were heterotopic ossification, postoperative sepsis, unplanned reoperation, implant failure, postoperative neurological deficit, venous thromboembolism, femoral head osteonecrosis, osteoarthritis and limb length discrepancy. No association was found between adverse events and injury severity score, comorbidities or other associated injuries.
CONCLUSION: Complications were common within three years in patients with pelvic and acetabular fractures treated surgically in a developing setting. While an increased Injury Severity Score was not associated with complications, certain fracture- and surgery-related factors may be associated with an increased risk. Heterotopic ossification was the most common adverse event despite formal gluteus minimus debridement and the use of NSAIDs. Further studies are needed to determine the medium- to long-term complications as well as the functional outcome of surgery and the complications of surgery.
Level of evidence: Level 4.
Keywords: acetabular fracture, pelvic fracture, complication, surgical
Introduction
Pelvic and acetabular fractures commonly occur following high energy trauma and have been reported to account for approximately 0.3-25% of all fractures encountered in the emergency department, especially in the polytraumatised patient.1-5 They frequently occur in conjunction with injuries that affect multiple systems and are associated with a mortality rate of up to 31%.4-8 Patient selection for operative management can be challenging; however, in cases with instability, operative intervention has been shown to improve functional outcomes but has inherent risks.9-16
The outcomes and complications of operative management in pelvic and acetabulum fractures have been shown to be influenced by multiple factors, including: female sex, chest injury, severe traumatic brain injury, increased body mass index (BMI), open fractures, use of surgical low pressure vacuum drains and surgical approach.4,6,10,11,17,18 Another factor that has previously been associated with complications in patients with pelvic and acetabular fractures is an increased Injury Severity Score (ISS).10,18,19 Complications within three years include wound infection 2-13%, deep venous thrombosis (DVT) 27%, metalware failure 1.5%, unplanned reoperation, iatrogenic neurological injuries 5.3%, heterotopic ossification and mortality of 5-15% but can be as high as 50% with open fractures.10,11,17,20
There are few reports in the literature looking at the surgical management of acetabular and pelvic fractures in a developing world clinical setting. Much of the above-mentioned epidemiological data and clinical outcome data are mainly from reports emanating from developed world settings. The patient profile and outcome may be different in the developing world due factors such increased waiting time to surgery, high prevalence of human immunodeficiency virus (HIV), hypoalbuminemia and comorbidities.21 Previous studies performed in low- and middle-income countries (LMICs) have looked at factors associated with mortality and the classification of certain fracture patterns. 4,22,23 There are, however, no studies that reported on the risk factors associated with complications following surgical intervention or their association with ISS.
The primary aim of our study was to identify the risk factors associated with complications in patients with pelvic and/or acetabular fractures treated surgically. Secondarily, we aimed to determine if an increased ISS is associated with an increased rate of postoperative complications.
Patients and methods
After ethical approval from our institution's research ethics committee, we used total enumerative sampling to identify all patients with pelvic and/or acetabular fractures treated surgically by an orthopaedic trauma fellowship-trained surgeon between 1 November 2017 and 30 April 2020. All data were obtained from medical records and radiographs. Inclusion criteria were all patients aged 13 years to 65 years at the time of injury, that sustained a pelvic and/or acetabular fracture and that were treated surgically. Fractures were classified using either the Tile, AO/OTA, Young-Burgess, and the Judet and Letournel classification systems.16,24-26 Exclusion criteria were abdominal surgery four weeks prior to fracture surgery that developed postoperative sepsis and patients referred for postoperative care that were treated at another institution.
Of the 120 surgically treated patients identified to meet the inclusion criteria, 88 patients were eligible for analysis (54 acetabular fractures, 45 pelvic fractures). Overall, 32 patients were excluded. Twenty-one patients were excluded due to missing medical records. We currently have no electronic patient database, and our medical records are hard copies. An additional 11 patients were lost to follow-up and were also excluded from the final analysis.
With regard to the indication for operative treatment, all pelvic fractures that were classified as rotationally and/or vertically unstable, according to the Tile AO/OTA classification, underwent operative stabilisation.24,25 In addition, patients with sacral fractures through and medial to the foramina, sacroiliac joint displacement of more than 1 cm and open pelvic fractures were treated operatively. For acetabular fractures the following criteria were used for operative management: intra-articular displaced fractures (> 2 mm), non-displaced intra-articular fractures assessed using roof arc angles on plain imaging and/or computer tomography (CT) subchondral arc (< 10 mm) to be within the weight-bearing zone, posterior wall fragment of a significant size (50% or more), posterior wall fragment size < 50% associated with instability of the hip joint as demonstrated by examination under anaesthesia (EUA) and finally, fracture dislocations with a noncongruent hip joint or incarcerated fragment. We categorised the methods of fracture fixation as follows: plate fixation (implying the use of plate and screws), screw fixation (referring to percutaneous screws plus infix) and sacral rods.
We assessed complications occurring within three years of surgical intervention. Early fracture-related infection (FRI) was defined according to the international consensus guidelines as infection that occurred within four weeks of surgery, whereas late FRI was defined as infection occurring four weeks or more post surgery.27,28 Superficial surgical site infection (SSI) was defined according to the Centers for Disease Control and Prevention (CDC) definition, as onset of infection within 30 days of the operative procedure and involving only the skin and/or subcutaneous tissue. In addition, it must have one of the following: purulent discharge or an isolated organism, from an aseptically taken specimen.29 Implant failure was defined as mechanical failure of the implant in one of the following manners: plastic failure (inability to maintain original shape resulting in clinical failure), brittle failure (failure caused by defect in design) and fatigue failure (caused by repetitive loading on the implant). Patients with venous thromboembolism (VTE) were those who had an acute first-time pulmonary embolism and/or lower-extremity deep vein thrombosis, diagnosed on duplex Doppler ultrasound, ventilation/perfusion (VQ) scan or CT angiogram. Heterotopic ossification (HO) was seen as the formation of lamellar bone inside soft-tissue structures where bone normally does not exist.30 Lastly fracture union was defined using clinical and radiographic parameters as: the absence of pain or tenderness during weight bearing and/or physical examination and palpation, combined with a radiographic appearance of bridging callus, trabeculae and/or obliteration of the fracture line with cortical continuity.31
We had no standard follow-up protocol after the initial six weeks post surgery. Patients had variable follow-up periods and number of visits, possibly being reviewed by a different clinician at each follow-up. Thus, radiographs taken at one day, six weeks, three months, six months, and any period thereafter during study period, were assessed postoperatively. This was done by using the Picture Archiving and Communication Systems (PACS - Carestream Vue Motion version 11.4.1.0) for fracture union, signs of infection, HO and/or metalware failure. Data extracted from medical records included date of injury, age at time of injury, mechanism of injury, fracture type, associated injuries, comorbidities, Morel-Lavallee lesion, number of days from injury to surgery, duration of surgery, surgical approach, type of fixation, site fixated, intraoperative blood loss, intravenous antibiotic usage, closed suction drain use, need for blood transfusion, need for intensive care unit (ICU), length of hospital stay (LOS), follow-up period and complications. After all the data points were collected, the ISS was calculated.32 Complications recorded included early/late FRI, postoperative neurological injury, SSI, unplanned reoperation, VTE, metalware failure, HO, femoral head avascular necrosis (AVN), post-traumatic osteoarthritis and mortality.
Statistical analysis
Statistical analysis was performed using Stata 15.0 (StataCorp. College Station, Texas). Continuous variables were reported as mean (with standard deviation [SD] and range) or median (with interquartile range [IQR] and range), and categorical variables as frequencies and percentages. The Shapiro-Wilk test was used to analyse the distribution of data. Normally distributed data were compared with the use of the unpaired Student's t-test, whereas the Mann-Whitney U test was used for non-parametric data. Categorical data were analysed using the chi-squared test unless the value in any cell was below 5 when Fisher's exact test was used. Binomial logistic regression was used to determine the odds ratio (ORs) and 95% confidence interval (95% CI) of the association of individual risk factors with the development of complications. A multivariable logistic regression model was developed using a forward stepwise approach to assess independently associated variables. All tests were two-sided, and the level of significance was set at p < 0.05.
Results
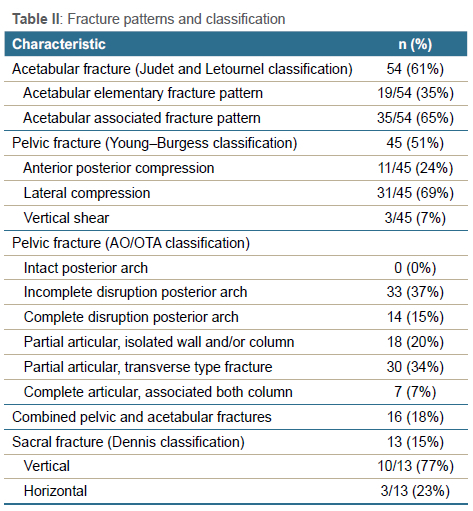
Of the 88 patients eligible for inclusion in the analysis, 54 were males (61%) and 34 females (39%). The mean age was 35 years (SD 14.1 years; range 13-65). Combined pelvic and acetabular fracture was found in 19% (16/88) of patients, with acetabular fractures accounting for 45% (40/88) and pelvic fractures accounting for 35% (31/88). Sacral fractures were found in 13 patients, one patient of which had an isolated sacral fracture 1% (1/88). Descriptive data relating to patient and injury characteristics are summarised in Tables I and II. The mean follow-up period was ten months (interquartile range [IQR] 4-14 months; range 0-31). There was an association with longer follow-up duration and the development of complications (OR 1.1; p = 0.003; 95% CI 1.03-1.17).
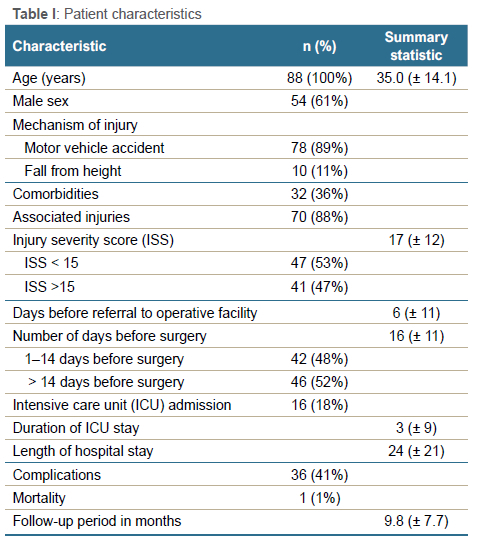
Complications were encountered in 41% (36/88) of the patients and those older than 35 years of age had a higher likelihood of developing complications (OR 1.04; p = 0.008; 95% CI 1.00-1.07). More than one complication occurred in 11 patients, of which three patients experienced more than two complications. The most encountered complication was HO 20% (18/88), which was associated with the use of a Kocher-Langenbeck approach (p < 0.001). We graded HO using the Brooker classification with 44% (8/18) having grade 3 HO, grade 2 in 27% (5/18), 16% (3/18) with grade 4 and 11% (2/18) had grade 1. Other complications included infection 10% (9/88), implant failure 4% (4/88), femoral head necrosis 4% (4/88), postoperative neurological deficit 2% (2/88), VTE 2% (2/88), osteoarthritis 1% (1/88) and leg length discrepancy 1% (1/88). There was one mortality, a polytraumatised patient with severe traumatic brain injury. Eleven patients (12%) required reoperation. The indications for reoperation were for infection (5/11), HO (2/11), implant failure (2/11) and avascular necrosis of the femoral head (2/11). The median time to reoperation was 14 days (range 4-220 days) and the median time to development of infection was 15 days (range 3-198 days).
Postoperative complications were associated with increasing age (OR 1.04; p = 0.014; 95% 1.01-1.07), but not with sex (p = 0.968). Thirty-two patients had pre-existing comorbidities but none of these variables were associated with complications (Table III). The most commonly encountered associated injuries were long bone fracture 47% (41/88) and chest injury 31% (28/88); however, no association was found between the presence of associated injuries and the development of early complications. The median ISS was 13 (IQR 9-25; range 4-75) and increased ISS was found not to be associated with an increased risk of complications (p = 0.641). Table IV summarises the adverse events in relation to the fracture pattern. Most fracture types had no correlation with complications except for vertical sacral fractures (OR 0.09; p = 0.008; 95% CI 0.01-0.76) and partial articular acetabular fractures with isolated column and/or wall involvement (AO/OTA type 62A fractures) (OR 3.75; p = 0.014; 95% CI 1.25-11.24).
Descriptive data relating to management of the fractures are provided in Table V. When excluding two patients that were referred more than one year from the time of injury, the mean time to surgery was 15 days (SD 11; range 2-60). A variety of surgical approaches was used. Plate and screw fixation was used in 69 patients, and this was associated with the development of complications. The mean duration of surgery was 139 minutes (SD 61; range 45-323) with a median blood loss of 300 ml (IQR 150-475; range 5-1500). Sixteen patients were admitted to ICU with a median ICU stay of 11 days. Blood transfusion was required in 50% (44/88) patients, and intraoperative transfusion was significantly associated with complications (OR 2.75; p = 0.042; 95% CI 1.02-7.45). Median hospital stay was 19 days (IQR 11-26.5; range 5-138).
Treatment-related factors associated with the development of complications on univariate analysis were Kocher-Langenbeck approach (OR 4.68; p = 0.001; 95% CI 1.87-11.70); plate fixation (OR 4.89; p = 0.018; 95% CI 1.3-18.31); posterior wall fixation (OR 4.17; p = 0.002 95% CI 1.66-10.47); and intraoperative blood transfusion (OR 2.76; p = 0.042; 95% CI 1.02-7.45).
Multivariate regression modelling (p < 0.001) revealed that only older patient age (OR 1.04; p = 0.040; 95% CI 1.00-1.08), Kocher-Langenbeck surgical approach, (OR 4.72; p = 0.003; 95% CI 1.67-13.28) and increased duration of follow-up (OR 1.1; p = 0.005; 95% CI 1.03-1.19) remained independently associated with the occurrence of complications.
Discussion
Our study aimed at identifying the risk factors associated with complications in patients with pelvic and/or acetabular fractures treated surgically in the developing world. The risk factors which were found to be associated with complications were either patient, injury or treatment related. Patient and injury characteristics were identified as having a pelvic fracture with an associated sacral fracture, a partial articular (isolated column and/or wall) acetabular fracture and increasing age. The treatment-related factors were Kocher-Langenbeck approach, posterior wall fixation, intraoperative blood transfusion and increased duration of follow-up. The most frequent complication found was HO. The ISS had no correlation with the development of complications; however, on post-hoc analysis we found that our study was not adequately powered to detect a difference.
The overall complication rate for our patient cohort was 41%, which was higher than the 31% reported by Jindal et al. but lower than the 58% reported by Russell et al.; however, our acetabular fracture group had a complication rate of 50% which was similar to that of Russell et al.1,11 In the pelvic fracture group our complication rate was 53%, which is lower than the 65% reported by Lundin et al.33 The pertinent factors which could account for this are, first, our mean follow-up period was ten months whereas theirs was 4.9 years. We found longer follow-up to be associated with increasing complications in our cohort. It is likely our complication rate would be higher than the 53% if our follow-up period were more than 12 months. Secondly, they set their primary objective as assessing reoperation rate, which was 25%, and higher than the 12% in our cohort. The factors that we considered reasons for reoperation were similar to their reasons for reoperation. Thirdly, they had 194 patients, which is more than twice the number of patients in our study and about four times that of the pelvic fracture cohort. Lastly, they included adverse events such as pneumonia, urinary tract infection and kidney failure, which we did not report on.
The incidence of associated injuries in patients with pelvic fractures was reported by Palmcrants et al. to be 99%, with the commonest associated injuries being those of the chest and lung.4 Chest injuries seem also to have been a commonly encountered associated injury in a cohort of patients with acetabular fractures.6 However, in our study, associated long bone fractures occurred more frequently (41/88). We found that 61% of patients with acetabular fractures (33/54) had concomitant long bone fracture, which is higher than the 40% reported in a meta-analysis by Giannoudis et al.34 Our mortality rate was surprisingly low at 1%, despite 89% of the patients having an associated injury; this is likely due to only two patients having combined chest, abdominal and head injuries and five having a combination of chest and head injury. Of those patients with an associated injury, 59% (41/70) had a high ISS of more than 15; however, contrary to previous reports, we found this not to be associated with an increased risk of early complications or mortality.4,18
There are several factors that previously have been noted to be associated with poor outcomes or complications, namely: female sex, chest injuries, traumatic brain injuries as well as having a combined pelvic and acetabular fracture.6,11,18 Age has been correlated with an increased risk of developing complications, with patients in the fourth decade of life being more at risk likely due to the mechanism of injury.6,18,19,35 The mean age of the aforementioned studies ranged from 31-38, which was similar to our mean age of 35 years. In our series, patients older than 35 years were more prone to develop complications (p = 0.008). We excluded patients that were older than 65 years as this population group has been shown to have higher complication rates than younger patients with the same ISS; they have also been shown to have a higher mortality rate.36,37
Combined pelvic and acetabular fractures are receiving increasing attention in literature, because of their complexity and the challenge they pose to management.6,9,35,38 The incidence of combined pelvic and acetabular fracture has been reported to range from 5-15%, which is similar to our incidence of 19%.9,34,35 These injuries have been correlated with increased ISS and mortality rate as well as haemodynamic instability and a greater blood transfusion rate.9,34,35 Our findings were comparable in terms of blood loss and ISS; however, we found that patients with a combined pelvic and acetabular fracture did not have any association with the development of complications.
We found that AO/OTA type 62A fractures of the acetabulum (posterior patterns including posterior wall and posterior column with or without associated wall fracture) had a correlation with an increased risk of complications (12 of 18; p = 0.014). One case developed a sciatic nerve palsy which has been commonly reported in literature. Seven patients developed HO.
Heterotopic ossification was the most frequent complication in our patient cohort and occurred in 17 of the 37 cases where the Kocher-Langenbeck approach was used. Several risk factors for the development of HO have been identified and these include craniocerebral trauma, abdominal trauma, posterior hip fracture dislocation, prolonged ventilatory requirements, race, American Society of Anesthesiologists physical status class, iliofemoral approach, Kocher-Langenbeck and gluteus minimus muscle necrosis.38-41 We treated two patients through the iliofemoral approach with one patient developing HO, and the correlation of the Kocher-Langenbeck approach has been stated above. We found no association with development of complications or HO with head and abdominal trauma. Routine gluteus minimus debridement was done for all patients undergoing the Kocher- Langenbeck approach; however, further study is required to determine which preventive measures are effective in our population. Previous reports have stated that gluteus minimus debridement, postoperative NSAID usage and/or single-dose radiotherapy are effective in reducing the rates of HO.41-44
Lastly, plate fixation was associated with increased complications which could possibly be due to the fact that these patients may have presented with more complex fracture patterns.45,46 Other authors, however, have not found this to be true.33,47,48 The correlation with plate fixation and complications in our patient cohort is possibly linked to the use of the Kocher-Langenbeck approach and HO.
Limitations of our study include poor documentation and missing medical records which led to the exclusion of several patients. Other limitations to the study included a small sample size and a short follow-up period. None of the patients in our cohort had weight and height measurements, and BMI association with complications could not be assessed. Our findings show that a longer follow-up is associated with an increased risk of complications and therefore it may be valuable for future studies to also look at medium- and long-term complications. Our study design did not include patients treated nonoperatively to determine if there is a true effect on outcomes of patients requiring surgical intervention. We also did not assess the adequacy of our surgical intervention, which could have been a contributing factor to adverse events. The most common complication was HO which was statistically significant, but we did not assess the functional outcomes; we are therefore not certain whether HO posed a clinically significant functional impairment.
treated nonoperatively to determine if there is a true effect on outcomes of patients requiring surgical intervention. We also did not assess the adequacy of our surgical intervention, which could have been a contributing factor to adverse events. The most common complication was HO which was statistically significant, but we did not assess the functional outcomes; we are therefore not certain whether HO posed a clinically significant functional impairment.
Conclusion
We found a high incidence of early complications in patients with pelvic and acetabular fractures treated surgically in a developing world setting. While an increased ISS was not associated with early complications, certain fracture- and surgery-related factors may be associated with an increased risk. Heterotopic ossification was the most common adverse event despite formal debridement and the use of NSAIDs. Further studies are needed to determine the medium- to long-term complications as well as the functional outcome of surgery and the complications of surgery.
Acknowledgements
The authors wish to thank Dr Christian Makita for his contribution in assisting with calculation of the Injury Severity Score.
Ethics statement
The authors declare that this submission is in accordance with the principles laid down by the Responsible Research Publication Position Statements as developed at the 2nd World Conference on Research Integrity in Singapore, 2010.
Prior to the commencement of the study, ethical approval was obtained from the University of KwaZulu-Natal Biomedical Research Ethics Committee BREC/00002159/2020. All procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Informed written consent was not obtained from all patients for being included in the study.
Declaration
The authors declare authorship of this article and that they have followed sound scientific research practice. This research is original and does not transgress plagiarism policies.
Author contributions
STM: study conceptualisation, data collection, data analysis, manuscript preparation and revision
MTND: study conceptualisation, study design, data review, manuscript review and revision
SM: data review, manuscript review and revision
LCM: study design, data analysis, manuscript review and revision
ORCID
Mbatha ST https://orcid.org/0000-0002-9027-283X
Duma MTN https://orcid.org/0000-0003-3854-2481
Maqungo S https://orcid.org/0000-0002-8735-8341
Marais LC https://orcid.org/0000-0002-1120-8419
References
1. Jindal K, Aggarwal S, Kumar P, Kumar V. Complications in patients of acetabular fractures and the factors affecting the quality of reduction in surgically treated cases. J Clin Orthop Trauma. 2019;10(5):884-89. [ Links ]
2. Pereira GJ, Damasceno ER, Dinhane DI, et al. Epidemiology of pelvic ring fractures and injuries. Revista Brasileira de Ortopedia (English Edition). 2017;52(3):260-69. [ Links ]
3. Gänsslen A, Pohlemann T, Paul CH, et al. Epidemiology of pelvic ring injuries. Injury. 1996;27:3-20. [ Links ]
4. Palmcrants J, Hardcastle TC, Naidoo SR, et al. Pelvic fractures at a new level 1 trauma centre: who dies from pelvic trauma? The Inkosi Albert Luthuli Central Hospital experience. Orthop Surg. 2012;4(4):216-21. [ Links ]
5. Pisanis A, Pohleman T, Burkhardt M, et al. Emergency stabilisation of the pelvic ring: clinical comparison between three different techniques. Injury. 2013;44(12):1760-64 [ Links ]
6. Phruetthiphat OA, Willey M, Karam MD, et al. Comparison of outcomes and complications of isolated acetabular fractures and acetabular fractures with associated injuries. J Orthop Trauma. 2017;31(1):31-36. [ Links ]
7. Glass NE, Burlew CC, Hahnhaussen J, et al. Early definitive fracture fixation Is safely performed in the presence of an open abdomen in multiply injured patients. J Orthop Trauma. 2017;31(12):624-30 [ Links ]
8. Kruppa CG, Sietsema DL, Khoriaty JD, et al. Acetabular fractures in children and adolescents: comparison of isolated acetabular fractures and acetabular fractures associated with pelvic ring injuries. J Orthop Trauma. 2018;32(2):e39-45. [ Links ]
9. Langford JR, Burgess AR, Liporace FA, Haidukewych GJ. Pelvic fractures: part 2. Contemporary indications and techniques for definitive surgical management. J Am Acad Orthop Surg. 2013;21(8):458-68. [ Links ]
10. Tile M, Helfet DL, Kellam JF, Vrahas M. Fractures of the pelvis and acetabulum. Baltimore: Williams & Wilkins; 1995 Jan. [ Links ]
11. Russell Jr GV, Nork SE, Routt Jr MC. Perioperative complications associated with operative treatment of acetabular fractures. J Trauma Acute Care Surg. 2001;51(6):1098-103. [ Links ]
12. Küper MA, Konrads C, Trulson A, et al. Complications of surgical approaches for osteosynthesis treatment of acetabular fractures: Analysis of pitfalls and how to avoid them. Injury. 2020;51(4):984-90. [ Links ]
13. Tile M. Acute pelvic fractures: II. Principles of management. J Am Acad Orthop Surg. 1996;4(3):152-61. [ Links ]
14. Tile M. Pelvic ring fractures: should they be fixed? J Bone Joint Surg Br. 1988;70(1):1-12. [ Links ]
15. Matta JM, Anderson LM, Epstein HC, Hendricks PI. Fractures of the acetabulum. A retrospective analysis. Clin Orthop Relat Res. 1986;1(205):230-40. [ Links ]
16. Judet R. Fractures of the acetabulum. Classification and surgical approaches for open reduction. J. Bone Joint Surg Am. 1961;43:30-59. [ Links ]
17. Boissonneault AR, Schenker M, Staley C, et al. Impact of closed suction drainage after surgical fixation of acetabular fractures. Arch Orthop Trauma Surg. 2019;139(7):907-12. [ Links ]
18. Lunsjo K, Tadros A, Hauggaard A, et al. Associated injuries and not fracture instability predict mortality in pelvic fractures: a prospective study of 100 patients. J Trauma Acute Care Surg. 2007;62(3):687-91. [ Links ]
19. Almahmoud K, Pfeifer R, Al-Kofahi K, et al. Impact of pelvic fractures on the early clinical outcomes of severely injured trauma patients. Eur J Trauma Emerg Surg. 2018;44(2):155-62. [ Links ]
20. Sharma S, Mathur H, Sinsuwadia K, Jaysingani T. Short-term follow-up of anterior and posterior both column fractures of acetabulum managed through both column plating. Eur J Orthop Surg Traumatol. 2019;29(3):605-10. [ Links ]
21. Maimin DG, Laubscher M, Maqungo S, Marais LC. Hypoalbuminaemia in orthopaedic trauma patients in a rural hospital in South Africa. Int Orthop. 2022 Jan;46(1):37-42. [ Links ]
22. Selvey DM, Siboto GM. Classification of posterior fracture dislocation of the hip joint: a modification of the Thompsen Epstein classification. Injury. 2001;32(3):217-19. [ Links ]
23. Maqungo S, Koller I, Roche S. Overlapping pubic symphysis dislocation: a case report and proposal of a classification system. SA Orthop J. 2010;9(4):74-77. [ Links ]
24. Tile M. Acute pelvic fractures: I. Causation and classification. J Am Acad Orthop Surg. 1996;4(3):143-51. [ Links ]
25. Meinberg EG, Agel J, Roberts CS, et al. Fracture and dislocation classification compendium. J Orthop Trauma. 2018;32:S1-0. [ Links ]
26. Langford JR, Burgess AR, Liporace FA, Haidukewych GJ. Pelvic fractures: part 1. Evaluation, classification, and resuscitation. J Am Acad Orthop Surg. 2013;21(8):448-57. [ Links ]
27. Depypere M, Kuehl R, Metsemakers WJ, et al. Recommendations for systemic antimicrobial therapy in fracture-related infection: a consensus from an international expert group. J Orthop Trauma. 2020;34(1):30. [ Links ]
28. Metsemakers WJ, Morgenstern M, Senneville E, et al. General treatment principles for fracture-related infection: recommendations from an international expert group. Arch Orthop Trauma Surg. 2019; 29:1-5. [ Links ]
29. Horan TC, Gaynes RP, Martone WJ, et al. CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infection Control & Hospital Epidemiology. 1992;13(10):606-608. [ Links ]
30. Bossche LV, Vanderstraeten G. Heterotopic ossification: a review. J Rehabil Med. 2005;37(3):129-36. [ Links ]
31. Corrales LA, Morshed S, Bhandari M, Miclau III T. Variability in the assessment of fracture-healing in orthopaedic trauma studies. J Bone Joint Surg Am. 2008;90(9):1862-8. [ Links ]
32. Baker SP, O'Neill B, Haddon W Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma Acute Care Surg. 1974;14(3):187-96. [ Links ]
33. Lundin N, Enocson A. Complications after surgical treatment of pelvic fractures: a five-year follow-up of 194 patients. Eur J Orthop Surg Traumatol. 2022;10(2):1-6. [ Links ]
34. Giannoudis PV, Grots MR, Papakostidis C, Dinopoulos H. Operative treatment of displaced fractures of the acetabulum: a meta-analysis. J Bone Joint Surg Br. 2005;87(1):2-9. [ Links ]
35. Susuki T, Smith WR, Hak DJ, et al. Combined injuries of the pelvis and acetabulum: nature of a devastating dyad. J Orthop Trauma. 2010;24(5):303-308. [ Links ]
36. Henry SM, Pollak AN, Jones AL, e al. Pelvic fracture in geriatric patients: a distinct clinical entity. J Trauma Acute Care Surg. 2002;53(1):15-20. [ Links ]
37. Alton TB, Firoosabadi R. Management of pelvic ring fractures in the geriatric patient. Current Geriatrics Reports. 2014;3(2):101-108. [ Links ]
38. Halawi MJ. Pelvic ring injuries: Surgical management and long-term outcomes. J Clin Orthop Trauma. 2016;7(1):1-6. [ Links ]
39. Firoosabadi R, Alton T, Sagi HC. Heterotopic ossification in acetabular fracture surgery. J Am Acad Orthop Surg. 2017;25(2):117-24. [ Links ]
40. Firoosabadi R, O'Mara TJ, Swenson A, et al. Risk factors for the development of heterotopic ossification after acetabular fracture fixation. Clin Orthop Relat Res. 2014;472(11):3383-88. [ Links ]
41. Chen MJ, Tigchelaar SS, Wadhwa H, et al. Gluteus minimus debridement during acetabular fracture surgery does not prevent heterotopic ossification-a comparative study. J Orthop Trauma. 2021;35(10):523-28. [ Links ]
42. Davis JA, Roper B, Muns JW, et al. Does postoperative radiation decrease heterotopic ossification after the Kocher-Langenbeck approach for acetabular fracture. Clin Orthop Relat Res. 2016;474(6):1430-305. [ Links ]
43. Griffin SM, Sims SH, Karunakar MA, et al. Heterotopic ossification rates after acetabular fracture surgery are unchanged without indomethacin prophylaxis. Clin Orthop Relat Res. 2013;471(9):2776-82. [ Links ]
44. Cichos KH, Spitler CA, Quade JH, et al. Do indomethacin or radiation for heterotopic ossification prophylaxis increase the rates of infection or wound complications after acetabular fracture surgery? J Orthop Trauma. 2020;34(9):455-61. [ Links ]
45. Swingmann J, Südkamp NP, Kõnig B, et al. Intra-and postoperative complications of navigated and conventional techniques in percutaneous iliosacral screw fixation after pelvic fractures: results from the German Pelvic Trauma Registry. Injury. 2013;44(12):1765-72. [ Links ]
46. Ochenjele G, Reid KR, Castillo RC, et al. Predictors of unplanned reoperation after operative treatment of pelvic ring injuries. J Orthop Trauma. 2018;32(7):e245-e250. [ Links ]
47. Lindsay A, Tornetta III P, Diwan A, Templeman D. Is closed reduction and percutaneous fixation of unstable posterior ring injuries as accurate as open reduction and internal fixation? J Orthop Trauma. 2016;30(1):29-33. [ Links ]
48. Elsohairy MM, Salama AM. Open reduction internal fixation versus percutaneous iliosacral screw fixation for unstable posterior pelvic ring disruptions. Orthop Traumatol Surg Res. 2017;103(2):223-27. [ Links ]
Received: July 2022
Accepted: October 2022
Published: May 2023
* Corresponding author: sandytools2@gmail.com
Editor: Prof. Maritz Laubscher, University of Cape Town, Cape Town, South Africa
Funding: No funding was received for this study.
Conflict of interest: The authors declare they have no conflicts of interest that are directly or indirectly related to the research.














