Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.22 n.1 Centurion 2023
http://dx.doi.org/10.17159/2309-8309/2023/v22n1a2
HAND
Functional outcome of free fibula grafting in benign non-reconstructable bone tumours involving the hand
Manish R ShahI, *; Manisha M ShahII; Isha M ShahIII
IDepartment of Orthopaedics, Dhiraj Hospital, Smt BK Shah Medical Institute and Research Centre, Sumandeep Vidyapeeth Deemed to be University, Waghodia, Gujarat, India
IIDepartment of Pathology, Medical College and SSG Hospital, Vadodara, Gujarat, India
IIIGMERS Medical College, Gotri, Vadodara, Gujarat, India
ABSTRACT
BACKGROUND: Bone tumours involving hands are usually benign but can be locally aggressive. Several treatments have been described. Usual modalities of treatment include curettage and bone grafting. In more advanced stages when short bones of the hand are involved with more than 70% cortical destruction, or when such treatment option is not possible (as with non-contained tumours with cortical breaches, pathological fracture), only the resection or amputation of the affected segment can offer an effective cure. We studied the role of the free fibula graft (non-vascularised) in such types of benign non-reconstructable (by conventional methods) hand tumours. The aims and objectives were to study the functional outcome of free fibula grafting in benign non-reconstructable bone tumours involving the hand and to analyse the complications, if any, and assess the causes and solutions for them
METHODS: We prospectively studied 15 patients with different types of benign, non-reconstructable bone tumours involving the hand operated by free fibula grafting. The study period ranged from January 2014 to December 2021. Follow-up ranged from 2 to 8 years (average of 4.26 years
RESULTS: Results were analysed by the QuidkDASH-9 score system. There was no recurrence. One case of superficial infection was treated with antibiotics and dressing. All patients were happy with the treatment and resumed their normal duties and functional movements
CONCLUSION: Use of the free fibula graft can be a good option for benign non-reconstructable bone tumours involving the hand to avoid amputation. The free fibula graft gives better results due to total excision of the lesion and strut graft support for good functional outcomes
Level of evidence: Level 3
Keywords: benign bone tumour, free fibula graft, QuickDASH-9 score, bone tumour, orthopaedic oncology
Introduction
Bone tumours involving hands are usually benign but can be locally aggressive. Of all the bone tumours, only 6% occur in the hand.1 Several treatments have been described. Usual modalities of treatment include curettage and bone grafting. Cytotoxic adjuvant agents such as liquid nitrogen, phenol and hydrogen peroxide can be used in conjunction with curettage to enhance the area of tumour kill, although their efficacy is still controversial.2-4 In some cases, local sclerosant injections are advocated. All such methods require contained lesions.
Optimal treatment of bone tumours requires a careful balance of local tumour control and preservation of hand function. Treatment plans are influenced by factors such as tumour size, bone destruction, risk of recurrence, proximity to joint surfaces and overall predicted function.
When insufficient bone stock is available for salvage, en bloc excision with reconstruction is needed. Reconstructive options include osteoarticular allograft, vascularised or non-vascularised bone graft from either local (for example, distal radius) or distant sites (for example, fibula or iliac crest), and arthrodesis. In more advanced stages when short bones of hands are involved with more than 70% destruction or when such treatment option is not possible (as in non-contained tumours with cortical breaches, pathological fracture), only the resection or amputation of the affected segment can offer an effective cure. Such lesions are non-reconstructable by conventional methods. This can lead to disability, more or less pronounced, depending on which bone is involved, and the characteristics of the patient. Over the years, various forms of reconstruction have been described, but it is difficult to provide a return to the previous functional level.5,6 Vascularised fibula grafts are usually reserved for bigger defects, and for the site where bigger diameter vessels are available for anastomosis. In hand tumours, the length of strut graft is less and digital vessels are of narrow diameter. We studied the role of the free fibula (non-vascularised) grafts in such types of benign non-reconstructable hand tumours. Our use of the term 'non-reconstructable' refers to lesions which cannot be filled with cancellous graft after curettage (conventional method) because of the non-contained nature of the tumour. In comparison to iliac crest graft, the fibula has the medullary canal for fixation of the graft by intramedullary wire, and the shape of the fibula can be matched to small hand bones; we therefore preferred the fibula in our study.
The aims were to study the functional outcome of free fibula grafting in benign non-reconstructable bone tumours (by conventional method) involving the hand. Objectives included the assessment of the functional outcome of free fibula grafting in benign non-reconstructable bone tumours involving the hand; to analyse the complications, if any, and assess the causes and solutions for them; to study the time of union of free fibula graft; to compare results with other centres; and to study different types of benign bone tumours involving the hand.
Methods
After obtaining clearance from the ethical committee of the institute, and informed consent from the patients, work was carried out on suitable patients in this interventional study. The sampling method was purposive sampling, and the study was conducted on 15 patients with benign bone tumours involving the hand, which were non-reconstructable.
Inclusion criteria were all cases of benign bone tumours irrespective of patient age. The benign nature was decided as per the clinical history and examination, radiological parameters (X-ray, CT scan, and MRI as required), or biopsy. Biopsy was done on all cases except those cases that were clearly benign by clinical and radiological parameters. Benign bone tumours are non-reconstructable-like lesions with pathological fracture, lytic expansile lesion involving more than 70% of the bone (phalanx or metacarpal), destruction or lesions with non-contained defect.
Exclusion criteria comprised patients who refused to participate in the programme; patients who did not have a minimum of six months follow-up; and patients with malignant bone tumours involving the hand (proved by preoperative biopsy).
Preoperative evaluation
Patients of either sex with benign non-reconstructable hand tumours were included in the study as per inclusion and exclusion criteria. Biopsy was done in all except three cases. Those three cases were clinically and radiologically confirmed as benign and patients were ready for final treatment. However, all three were informed about the risks and prognosis. All cases were subjected to routine pre-anaesthetic check-up and additional investigations where indicated.
The procedure was explained to the patients, and that follow-up at four, six, 12 and 24 weeks was necessary. The chances of recurrence and other complications were made clear.
Operative procedure
After preoperative investigations, patients were operated on with all standard sterile precautions. The fibular graft was harvested from the ipsilateral side in all cases. (As per our setup, one surgical team would operate per case, therefore an ipsilateral leg was chosen for the graft. However, if two teams are available, the contralateral leg can be used to make the procedure faster. Another reason for selecting the ipsilateral leg was, from the patient's point of view, to keep one side of the body pain-free.)
For tumours involving the thumb, a lateral approach was taken; for tumours involving phalanges, a midline dorsal approach (with splitting extensor tendon) was taken.
The tumour was excised as per preoperative measurements and intraoperative image intensifier television (IITV) guidance. The length of the fibula graft was decided before the excision of the tumour. Thorough curettage was done as per tumour protocol using a high-speed burr, and hydrogen peroxide and povidone-iodine wash was given. Intraoperative frozen section confirmed the benign nature on the table.
In all except two cases, we preserved proximal and distal articular margins. In two cases of tumours involving proximal phalanges of thumb, it was not possible to preserve the proximal articular surface due to the involvement by the tumour itself. In those two cases, we attempted the cartilage grafting technique (putting pieces of articular cartilage/fascia obtained while procuring fibula between the fibula graft and proximal articular surface). The graft was fixed by K-wire in all cases.
Postoperative protocol
Intravenous antibiotics were given for three days. Intravenous analgesics were given for one day followed by oral analgesics for 7-10 days. The first postoperative dressing was done on the second day and the second postoperative dressing on the fifth day. Suture removal was done at roughly two weeks. X-ray of the affected hand, biopsy and immunohistochemistry (IHC) (as per the case) were done postoperatively.
The patient was discharged from the hospital once the wound condition and the patient's general condition was satisfactory. The patient was called for follow-up at four weeks, six weeks, three months, six months and after a year. X-ray of the affected hand was done at each follow-up. Implant extraction (usually K-wire) was done after the radiological union of the graft.
Results
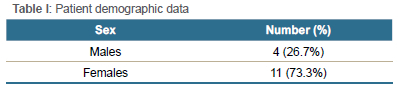
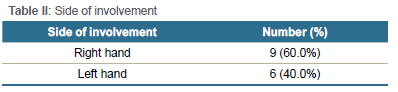
We prospectively studied 15 patients with benign bone tumours. All patients were operated on by a single surgeon. The study period ranged from January 2014 to December 2021. Of the 15 patients, four (26.7%) were male and 11 (73.3%) female. The right hand was involved in nine (60%) and the left hand in six (40%) patients (Tables I and II). Age ranged from 13 to 49 years (average 24.86).
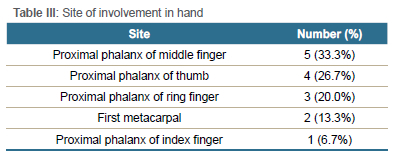
The first metacarpal was involved in two (13.3%) (Figures 1 and 2); a proximal phalanx of the middle finger in five (33.3%) (Figures 3 and 4); a proximal phalanx of the thumb in four (26.7%) (Figure 5); a proximal phalanx of the ring finger in three (20%); and a proximal phalanx of the index finger was involved in one (6.7%) of the patients (Table III).
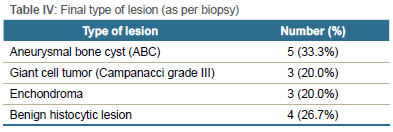
Preoperative and postoperative types of lesions (confirmed by biopsy) were bone cyst, aneurysmal bone cyst (ABC), giant cell tumour (GCT) and enchondroma. Postoperative (final biopsy) lesions included ABC (5/15 = 33.3%), GCT (3/15=20%), enchondroma (3/15 = 20%) and benign histocytic lesion (4/15 = 26.7%) (Table IV).
In all cases, the fibula graft was fixed with one K-wire. The average length of the fibula graft was 3 cm (range: 2.8-3.2). The wire was kept till union was found in three out of four cortices in AP and oblique views radiologically. The average time of graft union was 96.86 days (range: 90-100) in our study.
Cases were followed up for infection and wire-related complications in the early stage and recurrence and functional range of movements (ROM) in later stages. Follow-up ranged from 2 to 8 years (average of 4.26 years). Superficial infection was found in one case of first metacarpal tumour which healed by dressings and antibiotics over three weeks in total (Figure 5). No implant-related complications were found in our study. No recurrence was found in any case.
Functional ROM was satisfactory in all cases. All cases were assessed by the QuickDASH-9 score pre- and postoperatively. The average preoperative score was 73.7 and the average postoperative score was 24. All patients were happy with the treatment and resumed their normal duties and functional movements.
Discussion
We studied the results of free fibula graft in benign, non-reconstructable bone tumours. There are studies that describe the diagnostic approaches to hand tumours.1,4 Several treatments have been described. Usual modalities of treatment include curettage and bone grafting. Cytotoxic adjuvant agents such as liquid nitrogen, phenol and hydrogen peroxide can be used in conjunction with curettage to enhance the area of tumour kill, although their efficacy is still controversial.2-4 Studies compared results of curettage with or without allograft bone with the use of cement and other adjuvants. It was found that adequacy of tumour removal rather than the type of adjuvant determines the risk of recurrence.5,6
Most of the studies described giant cell tumours and options for treatment with follow-up mainly finding recurrence as the main complication. Averill et al. showed that curettage is not an effective method. Thirteen out of 15 tumours recurred in their series treated by curettage. They recommended amputation or local resection.6 Jones et al. described reconstruction of the entire metacarpal bone and metacarpophalangeal joint using osteocutaneous fibula free flap and silicone arthroplasty for GCT of the third metacarpal bone. They showed that a free vascularised fibula graft is ideal for the reconstruction of defects of metacarpal bone.7 Naam et al. showed recurrence after one year in their study for GCT fourth and fifth metacarpal bone which was treated by pulmonary lobe resection.8 Lim and Babineaux showed arthrodesis as a treatment for tumours involving the entire first metacarpal bone. They used a tricortical iliac crest bone graft. Nine months follow-up in their study showed no recurrence.9
Other authors showed the use of vascularised grafts in their studies.10-12 When insufficient bone stock is available for salvage, en bloc excision with reconstruction is needed. Reconstructive options include osteoarticular allograft, vascularised or non-vascularised bone graft from either local (i.e., distal radius) or distant sites (i.e., fibula or iliac crest), and arthrodesis.11,12 Saini et al., in their series, showed the use of autogenous fibula for the reconstruction of aggressive GCT of distal radius Campanacci grade II/III.13 Biopsy was not done only in cases that were sure to be benign in nature by clinical and radiological parameters.14 Authors have recently described case reports of GCT being treated by free fibula graft with promising results.15,16 A study done by Mukherjee et al. showed that up to 20 cm free fibula graft can be used in adults (with 36 cm total fibula length) and up to 10 cm free fibula graft can be taken in children (with total fibula length of 25 cm).17 Furthermore, vascular fibula graft requires surgical expertise or assistance from a plastic/microvascular surgeon. Harvesting vascular fibula graft takes more surgical time and requires compliance of the patient. All these factors increase the cost of surgery.18
We have studied all common types of benign bone tumours for a reasonably long period (seven years). No recurrence was found in any type of tumour. All our tumours were non-reconstructable by routine curettage and cancellous bone grafting techniques. Our results matched those of published case reports. We used K-wire, which is a very common implant. The use of other implants such as plates or fixators can cause problems such as impingement of the implant and infection. No implant-related complication was found in our series. Only one case of superficial infection found in the first metacarpal tumour was treated by dressing and antibiotics for three weeks. Our time to graft union and graft incorporation matches other studies.16 All of our patients gained functional movements and returned to their normal professions.
The variety of tumours and long-term follow-up are a strength of our study. More patients and study results from different centres would be useful to study the treatment method.
Conclusion
The use of free fibula graft is a good option for benign non-reconstructable bone tumours involving the hand to avoid amputation. It gives better results due to total excision of the lesion and strut graft support for good functional outcomes. This treatment option provides fewer chances of recurrent tumour and prevents future re-surgeries. Cosmetically it is more acceptable than amputation. Though other modalities of treatment are available for contained defects in benign tumours, for tumours having more than 70% destruction of the small bone in the hand, free fibula grafting is a viable option available to the general orthopaedic surgeon. Our study showed no recurrence at long-term follow-up and full patient satisfaction.
Acknowledgements
We acknowledge the immense help received from the scholars whose articles are cited and included in the references of this manuscript. The authors are also grateful to authors/editors/publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
We acknowledge the patients, their family members, hospital staff, and all others who directly or indirectly participated in the study.
Ethics statement
The authors declare that this submission is in accordance with the principles laid down by the Responsible Research Publication Position Statements as developed at the 2nd World Conference on Research Integrity in Singapore, 2010.
Prior to the commencement of the study, ethical approval was obtained from the Sumandeep Vidyapeeth Institutional Ethics Committee: SVIEC/MED/RP/20029.
All procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Written informed consent was obtained from all patients included in the study. Consent was obtained from patients for the use of clinical photographs, and these images were adequately anonymised.
Declaration
The authors declare authorship of this article and that they have followed sound scientific research practice. This research is original and does not transgress plagiarism policies.
Author contributions
MRS: study conceptualisation, data capture, data analysis, first draft preparation, manuscript revision
MMS: data analysis, manuscript preparation, manuscript revision IMS: design of testing set-up, manuscript preparation
ORCID
Shah MR https://orcld.org/0000-0002-9381-9095
Shah MM https://orcid.org/0000-0002-2252-9752
Shah IM https://orcld.org/0000-0002-7468-0278
References
1. Hsu CS, Hentz VR, Yao J. Tumours of the hand. Lancet Oncol. 2007;8:157-66. https://doi.org/10.1016/S1470-2045(07)70035-9 [ Links ]
2. Turcotte RE. Giant cell tumor of bone: Giant cell tumor of bone. Orthop Clin North Am. 2006 Jan;37(1):35-51. https://doi.org/10.1016Zj.ocl.2005.08.005 [ Links ]
3. Errani C, Ruggieri P, Asenzio MA, et al. Giant cell tumor of the extremity: A review of 349 cases from a single institution. Cancer Treat Rev. 2010 Feb;36(1):1-7. https://doi.org/10.1016/j.ctrv.2009.09.002 [ Links ]
4. Payne WT, Merrell G. Benign bony and soft tissue tumors of the hand. J Hand Surg Am. 2010 Nov;35(11):1901-10. https://doi.org/10.1016/jjhsa.2010.08.015 [ Links ]
5. Blackley HR, Wunder JS, Davis AM, et al. Treatment of giant-cell tumors of long bones with curettage and bone-grafting. J Bone Joint Surg Am. 1999 Jun;81(6):811-20. https://doi.org/10.2106/00004623-199906000-00008 [ Links ]
6. Averill RM, Smith RJ, Campbell CJ. Giant-cell tumors of the bones of the hand. J Hand Surg Am. 1980 Jan;5(1):39-50. https://doi.org/10.1016/s0363-5023(80)80042-6 [ Links ]
7. Jones NF, Dickinson BP, Hansen SL. Reconstruction of an entire metacarpal and metacarpophalangeal joint using a fibular osteocutaneous free flap and silicone arthroplasty. J Hand Surg Am. 2012, 37:310-15. https://doi.org/10.1016/jjhsa.2011.10.031 [ Links ]
8. Naam NH, Jones SL, Floyd J, Memisoglu EI. Multicentric giant cell tumor of the fourth and fifth metacarpals with lung metastases. Hand (NY). 2014;9:389-92. https://doi.org/10.1007/s11552-013-9574-x [ Links ]
9. Lim S, Babineaux KL. reconstruction of an entire thumb metacarpal: a case report. Plast Reconstr Surg Glob Open. 2016;4:610. https://doi.org/10.1097/GOX.0000000000000593 [ Links ]
10. Kotwal PP, Nagaraj C, Gupta V. Vascularised joint transfer in the management of recurrent giant cell tumour of the second metacarpal. J Hand Surg Eur Vol. 2008; 33:314-16. https://doi.org/10.1177/1753193408089048 [ Links ]
11. Maini L, Cheema GS, Yuvarajan P, Gautam VK. Free osteoarticular metatarsal transfer for giant cell tumor of metacarpal - a surgical technique. J Hand Microsurg. 2011;3:89-92. https://doi.org/10.1007/s12593-011-0048-5 [ Links ]
12. Malizos KN, Dailiana ZH, Innocenti M, et al. Vascularized bone grafts for upper limb reconstruction: defects at the distal radius, wrist, and hand. J Hand Surg Am. 2010;35:1710-18. https://doi.org/10.1016/jjhsa.2010.08.006 [ Links ]
13. Saini R, Bali K, Bachhal V, et al. En bloc excision and autogenous fibular reconstruction for aggressive giant cell tumor of distal radius: a report of 12 cases and review of literature. J Orthop Surg Res. 2011;6(14). https://doi.org/10.1186/1749-799X-6-14 [ Links ]
14. Bickels J, Malawer MM. Biopsy of musculoskeletal tumors. In: Operative Techniques in Orthopaedic Surgical Oncology. 2014. p. 25-33. [ Links ]
15. Fernandes H, Almeida M, Lopes R, et al. Reconstruction of the second metacarpal bone after bone tumor resection with free fibular graft. J Cas Rep. 2018;8:290-93. https://doi.org/10.17659/01.2018.0078 [ Links ]
16. Agrawal AC, Verma S, Kar B, et al. Mammoth giant cell tumor of the first metacarpal: a case report and management trends. Cureus. 2021;13(7):e16150. [ Links ]
17. Mukherjee AN, Pal AK, Singharoy D, et al. Harvesting the free fibular graft: A modified approach. Indian J Orthop. 2011 Jan;45(1):53-56. https://doi.org/10.4103/0019-5413.73657 [ Links ]
18. Devireddy SK, Senthil MM, Kishore KRV, et al. Evaluation of non-vascular fibula graft for mandibular reconstruction. J Maxillofac Oral Surg. 2015 Jun;14(2):299-307. https://doi.org/10.1007/s12663-014-0657-1 [ Links ]
Received: April 2022
Accepted: September 2022
Published: March 2023
* Corresponding author: manishshah2001in@yahoo.co.in
Editor: Dr Duncan McGuire, University of Cape Town, Cape Town
Funding: No funding was received for the purposes of performing this study.
Conflict of interest: The authors declare they have no conflicts of interest that are directly or indirectly related to the research.














