Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SA Orthopaedic Journal
versión On-line ISSN 2309-8309
versión impresa ISSN 1681-150X
SA orthop. j. vol.21 no.4 Centurion 2022
http://dx.doi.org/10.17159/2309-8309/2022/v21n4a6
BASIC SCIENCES
The mechanical testing of a novel interlocking forearm nail
Henry S Pretorius*; Marilize C Burger; Nando Ferreira
Division of Orthopaedic Surgery, Department of Surgical Sciences, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
ABSTRACT
BACKGROUND: Mechanical testing of newly designed implants provides valuable insight into their mechanical properties. This provides surgeons with information about implant choice for the treatment of fractures and the effect of the implant's mechanical properties on fracture healing
METHODS: A novel interlocking forearm nail was subjected to standardised mechanical testing according to the Standard Specification and Test Methods for Intramedullary Fixation Devices (ATSM 126416), using static and dynamic four-point bending and static torsion (ASTM STP 588). Three nails were used for the static bending and torsion and nine for the dynamic bending tests. All nails were catalogued, numbered and photographed before testing
RESULTS: The mechanical testing results showed a mean force yield (Fy) of 566 ± 20 N, a moment of yield (My) 10.75 ± 0.37 Nm, a stiffness of 67.10 ± 2 N/mm and structural stiffness of 1.53 ± 0.50 m2. The torsional stiffness of the nail was 0.088 ± 0.002 Nm/°. The four-point dynamic bending test showed a fatigue strength of 5.23 Nm. This value was determined using the semi-log moment/ number of cycles (M-N) diagram and showed a 50% failure at a million cycles. If the moment were reduced to 4.4 Nm, mathematically, the survival rate would improve to 90%
CONCLUSION: The results from this mechanical testing show that this novel intramedullary forearm nail can resist mechanical forces experienced during fracture healing and could potentially be used in future clinical studies
Level of evidence: Level 4
Keywords: mechanical testing, ASTM, load, yield, stiffness, fatigue strength
Introduction
The mechanical properties of implants are one of many factors that contribute to the mechanobiological environment for fracture healing. Mechanical testing of newly designed implants provides valuable insight into their mechanical properties. This provides surgeons with information about implant choice and the effect of the implant's mechanical properties on fracture healing.1
Although not weight-bearing, radius and ulna fracture fixation are still exposed to significant in vivo forces, including pronation/ supination rotational and bending moments created when carrying objects. The ability of an implant to withstand these forces is considered when these devices undergo mechanical testing prior to clinical use.
Compression plate fixation of the forearm provides absolute stability with no fragment movement while bridge plating and nail fixation will provide relative stability with some movement between fragments. Restoration of length and alignment and the ability to control rotation make intramedullary nail fixation ideal for managing long bone fractures. Comminuted and segmental fractures, which are frequently seen in high-energy gunshot wounds, are particularly well suited to intramedullary fixation as the intramedullary nail provides load-sharing mechanics, restores anatomy and fragment stability and has a minimal invasive insertional approach which can be important when soft tissue injuries are involved. With nail fixation of simple forearm fractures, the bone provides some mechanical support, but with comminuted or segmental fractures, the nail provides most of the support, so any implant must have the mechanical properties to maintain stability until fracture union.
A novel interlocking forearm nail was designed to address both length and rotational stability in forearm fractures. The implant design was based on findings from a computed tomography scan anatomical study.2 In the design process, the biomechanical properties of bone, the modulus of elasticity of metals and the mechanical testing process of similar products in the literature were used to inform the process.1,3,4
The modulus of elasticity of bone ranges from 10-28 GPa (gigapascals or kN/mm20 and for the radius specifice.ly 10-17 GPa.5 Titanium specifically has a modulus closest to bone and better fatigue than stain less steel ; afte r taking thi s i nto account, titanium (Ti6AI4V ISO 5832-3) was utilised.6-8
The nail is machined to the correct specifications instead of being cast or 3D printed. The base material, a solid tube, is made by additive manufacturing (AM), an advanced manufacturing technology using 3D CAD by adding materials in a layer-by-layer fashion that allows products with geometric complexities as simple as solid tube structures or complex shapes like replacement mandible bones to be made.9
This study reports the results of standardised mechanical testing of a novel forearm nail to ascertain whether the implant would withstand physiologicalload during fracture healing.
Methods
Standardised mechanical testing to ascertain the clinical applicability of the new nail design was conducted. Implants are generally exposed to between 150 000 and 200 000 cycles of repeated strain over three months until fracture union.4 To simulate the upper limit of expected cycles until union, fatigue testing is performed at a standard amount of one million cycles.4 The four-point bending with static and dynamic tests and static torsion tests are the implants' prescribed tests. Saka et al. showed a mean bending test force of 539.75 N and a mean torsional force of 0.028 Nm/°.10 Gardner et al. used 250 N force represented by partial weight-bearing to evaluate femur fracture intramedullary nails as an idea of mechanical strength needed for specific orthopabdic products.1 With the evaluation of plate constructs by Roberts et al., the locked hybrid model showed anterior bending stiffness of 194 N/mm, a lateral stiffness of 430 N/mm and torsional stiffness of 0.42 Nm/0.11
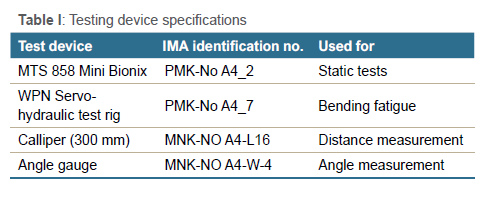
Mechanical testing according to the Standard Specification and Test Methods for Intramedullary Fixation Devices (IMFD) (ATSM 1264-16) was undertaken by IMA Materialforschung und Anwendungstechnik GMBH (Dresden, Germany 01109).4 This refers to static and dynamic four-point bending and static torsion testing. All testing and statistical analysis was performed according to industry standards (ASTM STP 588). All nails were catalogued, numbered and photographed before testing. Three nails were used for the static bending and torsion, and nine nails were used for the dynamic bending tests. The dest device specifications are shown in Table I.
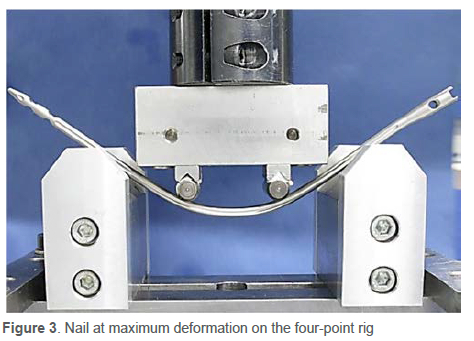
The nails for four-point bending were placed on the hydraulic rig (MTS 858 Mini Bionix) with a 38 mm centre span, and the distance to the loading points was also 38 mm (Figures 1 and 2). A constant force at a rate of 0.1 mm/s was applied until failure. In this test, failure was defined as permanent deformation, breakage or buckling. The test was stopped, and the maximum force was measured in Newtons (N) (Figure 3). The results are reported as yield force, momentoh pield, stiffness and structural stiffness. Dynamic testing was performed in a WPN Servo-hydraulic test rig and followed a sinusoidal cyclic load waveform at a frequency of 5 Hz and programmed for 1 million cycles or until failure. The results were plotted on a moment/number of cycles (M-N diagram) graph to determine the fatigue strength that 50% of the specimens will survive at one million cycles.

The test setup for the dynamic torsional test has the nail clamped between a base plate and hydraulic rotation device (Figure 4). The system rotates at a fixed rate of 5° per minute until failure. The results are reported as torsional stiffness.

Results
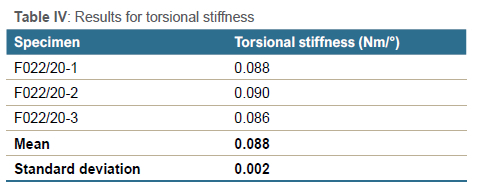
Following the ATSM 1264-16 guidelines, a report was supplied showing photos of the setup, the results and photographs of breakages. A summary of the testing parameters is shown in Table II. The mechanical testing results showed a mean force yield (Fy) of 566 ± 20 N, a moment of yield (My) 10.75 ± 0.37 Nm, a stiffness of 67.10 ± 2 N/mm and structural stiffness of 1.53 ± 0.50 m2 (Table III). The torsional stiffness of the nail was similar in the three specimens, with a mean result of 0.088 ± 0.002 Nm/° (Table IV). The four-point dynamic bending test showed a fatigue strength of 5.23 Nm. This value was determined using the semi-log M-N diagram and showed a 50% failure at one million cycles.
Due to the large numbers used for the cycles and the small numbers used for the moment, the graphs are presented as cycles in a logarithmic scale on the X-axis and the moment in a linear scale on the Y-axis. If the moment was reduced to 4.4 Nm, mathematically, the survival rate improved to 90% (Figure 5). The force applied can be calculated mathematically with the forearm as the lever arm: moment [Nm] = force [N] χ lever arm [m]. If the forearm from elbow to palm measures 0.2 m, the force would be 22 N or 2.2 KgF (Kilogram-force).
All the samples used for dynamic testing were tested until failure, and the place of failure was then noted. To this end, photos of the broken nails were supplied to show where each nail failed (Figure 6). In this example, the nails broke in the shaft and not through the locking holes.

Discussion
Mechanical testing of newly designed implants provides valuable insight into their mechanical properties and ability to withstand expected physiological forces during fracture healing. This provides surgeons with information about implant choice for fractures and the effect of the implant's mechanical properties on bone and fracture healing.
Bone is anisotropic, indicating different tolerances to forces applied from different directions. Normal bone can withstand axial forces of approximately 15 000 N and tangential forces of 6 000 N.5 The human upper limb seldom generates forces exceeding 200 N.12,13 Halilaj et al. and Putnam et al., in various tests of the wrist function for jar twist and grip, showed that the maximum force generated was 47-65 N.14,15 Horii used 140 N when testing wrist strength and transfer of mechanical loads to the carpus.16 Peine et al. tested dorsal plates for distal radius fractures and applied a maximum force of 400 N for testing plate strength.17 Implants are expected to withstand up to 200 N forces to allow fracture healing.
The human forearm is rarely exposed to forces exceeding 200 N, but any implant is expected to survive this threshold tolerance. In an article by Saka et al., the yield strength of the radial nail had a mean of 539 N and torsional strength of 0.028 Nm/°.3 The yield strength in the current study was 566 N and a higher torsional strength of 0.080 Nm/°. As this is a locked nail, the amount of comminution of the fracture affects how much of the torsional forces are transferred to the prosthesis. With load-sharing nails, the length of cortical contact is reduced in severely comminuted fractures and a higher torque resistance is therefore beneficial.18 This shows the proposed implant to have results equivalent to contemporary forearm nails in clinical use.
Dynamic testing showed a moment strength of 5.2 Nm is 50% survival with one million cycles. With extrapolation from the graph to 4.4 Nm, the survival of the implant improves to 90%. This is equivalent to exposing the nail to a 2.2 kg weight held in the hand. As the lever arm or forearm, in this case, gets longer, the force will reduce. This will allow the clinician to allow mobilisation of the forearm while allowing functional activities with a weight limit until union of the fracture.
The standardised testing of implants by independent companies provides integrity for the results. These standard tests limit the number of implants needed for testing that may result in slightly different results and could help make the semi-logarithmic graphs more accurate.
Conclusion
The results from the study's mechanical testing show that this novel intramedullary forearm nail can resist mechanical forces experienced during fracture healing and could potentially be used in future clinical studies.
Ethics statement
The author/s declare that this submission is in accordance with the principles laid down by the Responsible Research Publication Position Statements as developed at the 2nd World Conference on Research Integrity in Singapore, 2010. Prior to commencement of the study, ethical approval was obtained from the following ethical review board: Stellenbosch University Health Research Ethics committee, S20/04/100 (PhD).
Declaration
The authors declare authorship of this article and that they have followed sound scientific research practice. This research is original and does not transgress plagiarism policies.
Author contributions
HSP: study conceptualisation, first draft preparation, data analysis and manuscript revision
MCB: data analysis and manuscript revision NF: data analysis and manuscript revision
ORCID
Pretorius HS https://orcld.org/0000-0002-7419-0885
Burger MC https://orcld.org/0000-0003-2831-4960
Ferreira N https://orcld.org/0000-0002-0567-3373
References
1. Gardner MJ, Silva MJ, Krieg JC. Blomechanical testing of fracture fixation constructs: Variability, validity, and clinical applicability. J Am Acad Orthop Surg. 2012;20:86-93. [ Links ]
2. Pretorius HS, Ferreira N, Burger MC. A computer tomography-based anthropomorphic study of forearm osteology: implications for prosthetic design. SA Orthop J. 2021;20(3):162-66. [ Links ]
3. Saka G, Saglam N, Kurtulmus T, et al. New Interlocking Intramedullary radius and ulna nails for treating forearm diaphyseal fractures in adults: A retrospective study. Injury. 2014;45(Suppl 1):S16-23. [ Links ]
4. ASTM. Standard Specification and Test Methods for Intramedullary Fixation Devices 1. Annual book on ASTM standards. 2003. p1-22. [ Links ]
5. Bosisio MR, Talmant M, Skalli W, et al. Apparent Young's modulus of human radius using inverse finite-element method. J Biomech. 2007;40(9):2022-28. [ Links ]
6. Niinomi M, Nakai M. Titanium-based biomaterials for preventing stress shielding between implant devices and bone. Int J Biomech. 2011;2011:1-10. [ Links ]
7. Koh J, Berger A, Benhaim P. An overview of internal fixation implant metallurgy and galvanic corrosion effects. J Hand Surg Am. 2015;40(8):1703-10.http://dx.doi.org/10.1016/j.jhsa.2015.03.030 [ Links ]
8. Hayes JS, Richards RG. The use of titanium and stainless steel in fracture fixation. Expert Rev Med Devices. 2010;7(6):843-53. [ Links ]
9. Liu S, Shin YC. Additive manufacturing of Ti6Al4V alloy: A review. Mater Des. 2019 Feb;164:107552. https://doi.org/10.1016/j.matdes.2018.107552 [ Links ]
10. Saka G, Saglam N, Kurtulmus T, et al. Treatment of isolated diaphyseal fractures of the radius with an intramedullary nail in adults. Eur J Orthop Surg Traumatol. 2014;24(7):1085-93. [ Links ]
11. Roberts JW, Grindel SI, Rebholz B, Wang M. Biomechanical evaluation of locking plate radial shaft fixation: unicortical locking fixation versus mixed bicortical and unicortical fixation in a sawbone model. J Hand Surg Am. 2007;32(7):971-75. [ Links ]
12. Rikli DA, Honigmann P, Babst R, et al. Intra-articular pressure measurement in the radioulnocarpal joint using a novel sensor: in vitro and in vivo results. J Hand Surg Am. 2007 Jan;32(1):67-75.https://doi.org/10.1016/j.jhsa.2006.10.007 [ Links ]
13. Kuhn S, Burkhart KJ, Schneider J, et al. The anatomy of the proximal radius: implications on fracture implant design. J Shoulder Elb Surg. 2012;21(9):1247-54. http://dx.doi.org/10.1016/j.jse.2011.11.008 [ Links ]
14. Halilaj E, Moore DC, Patel TK, et al. Early osteoarthritis of the trapeziometacarpal joint is not associated with joint instability during typical isometric loading. J Orthop Res. 2015;33(11):1639-45. [ Links ]
15. Putnam MD, Meyer NJ, Nelson EW, et al. Distal radial metaphyseal forces in an extrinsic grip model: Implications for postfracture rehabilitation. J Hand Surg Am. 2000;25(3):469-75. [ Links ]
16. Horii E, Garcia-Elias M, An KN, et al. Effect on force transmission across the carpus in procedures used to treat Kienböcks disease. J Hand Surg Am. 1990;15(3):393-400. [ Links ]
17. Peine R, Rikli DA, Hoffmann R, et al. Comparison of three different plating techniques for the dorsum of the distal radius: A biomechanical study. J Hand Surg Am. 2000;25(1):29-33. [ Links ]
18. Marcus RE. Practical biomechanics, techniques in orthopaedics. 1998 Jan;13(1):1-8. [ Links ]
Received: April 2022
Accepted: June 2022
Published: November 2022
Editor: Prof. Leonard C Marais, University of KwaZulu-Natal, Durban, South Africa
Funding: No funding was received for this study.
Conflict of interest: All research related to the design and manufacture of the intramedullary nail system was done in conjunction with ImplantCast GmbH (Buxtehude, Germany). Prototypes were produced and provided for research purposes at no cost. All research-related costs were borne by Stellenbosch University. A royalty agreement between Stellenbosch University and ImplantCast GmbH (Buxtehude, Germany) was negotiated in the event of the design eventually being used commercially.
* Corresponding author: hsp359@sun.ac.za














