Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SA Orthopaedic Journal
versión On-line ISSN 2309-8309
versión impresa ISSN 1681-150X
SA orthop. j. vol.21 no.4 Centurion 2022
http://dx.doi.org/10.17159/2309-8309/2022/v21n4a5
TRAUMA AND GENERAL ORTHOPAEDICS
The burden of road traffic accident-related trauma to orthopaedic healthcare and resource utilisation at a South African tertiary hospital: a cost analysis study
Ndivhoniswani D Thikhathali*; Mthunzi V Ngcelwane
Department of Orthopaedics, University of Pretoria, Steve Biko Academic Hospital, Pretoria, South Africa
ABSTRACT
BACKGROUND: Road traffic accidents (RTAs), the second commonest cause of trauma in South Africa (SA), are on the rise. It is therefore important to study and understand the burden of RTA-related injuries on our orthopaedic healthcare and healthcare in general, in order to devise new prevention strategies to minimise the number of RTAs
METHODS: A retrospective analysis of data from orthopaedic trauma intake records was done for patients admitted with RTA-related injuries to the orthopaedic department at a South African tertiary hospital between February 2019 and January 2020. Hospital records and the PAC (picture archiving and communication) system were analysed for radiological studies done. The Uniform Patient Fee Schedule (UPFS) was analysed for individual costing of all variables being studied
RESULTS: There were 642 patients seen and managed with RTA-related injuries included in this study. Seventy-one per cent of them were males, with an average age of 35 years. The majority (76.2%) were motor vehicle occupants, whereas 17% were pedestrians. Seventeen per cent of them had polytrauma. Four hundred and sixty-two (76%) patients required some form of surgical intervention and spent an average of 171 minutes in theatre per procedure. Ten per cent of these patients required ICU/HCU admission for an average of 13 days. The total length of hospital stay was an average of 21.8 days. The majority of patients (67%) had some form of orthopaedic implant inserted, with an average of 1.3 implants per patient. The average cost per patient was R92 737.39. The major cost drivers were hospital stay, ICU/HCU stay, implant cost, radiological studies and theatre utilisation, respectively
CONCLUSION: Management of RTA-related trauma puts a significant burden on orthopaedic healthcare management and resource utilisation. While we may not be able to directly influence other contributing factors to high costs, reducing the use of temporary external fixators may help reduce the cost of managing RTA victims
These findings provide scientific data which will help support the implementation of preventative measures aimed at minimising the numbers of RTAs we see on our roads, thereby minimising the burden this puts on our healthcare system.
Level of evidence: Level 3
Keywords: road traffic accident, burden, implant cost, theatre time, length of hospital stay, polytrauma
Introduction
Road traffic accidents (RTAs) are one of the commonest causes of trauma globally, and are ranked the ninth leading cause of mortality worldwide.1-4 RTAs have become a neglected global epidemic and they continue to rise, mostly in low- and middle-income countries (LMICs) like South Africa (SA).1,2,5 RTAs are the second most common cause of trauma in SA, the most common being interpersonal violence (IPV).2
Many patients with trauma-related injuries sustain musculo-skeletal injuries.6-8 These injuries increase the workload for orthopaedic surgeons who treat the majority of these patients.7 The majority of patients affected are pedestrians, cyclists and passengers in commercial vehicles.2,6,9
RTAs mostly cause high-energy injuries and the majority of the patients have polytrauma, sustaining long bone fractures and life-threatening head, blunt chest and abdominal injuries.9,10 They are prioritised for emergency theatre management and intensive care unit (ICU) or high care unit (HCU) admission because they have life- or limb-threatening conditions which require emergency procedures.7,9,11-13
They utilise more theatre time on initial theatre visits with orthopaedic and non-orthopaedic lifesaving, damage control surgical/orthopaedic procedures being performed. Up to 26% of them will have second theatre visits for definitive management with some form of orthopaedic implants. These implants play a major role in driving the financial burden of managing musculoskeletal trauma.8,9
The severity of the injury plays a big role in influencing the length of ICU stays as well as the overall length of hospital stay.6'7,11,12 Many musculoskeletal injuries have increased risks of developing complications which will require multiple theatre visits, multiple radiological studies and a subsequent prolonged length of hospital stay.14
There is a big discrepancy in reporting the number of RTA-related injuries in our country. Only the RTA-related fatalities are reported on national statistics, while non-fatal injuries, said to be three to eight patients per reported accident, are unreported.15,16 These patients are seen and managed at our healthcare facilities, which increases the disease burden both financially and in terms of resource utilisation in orthopaedic healthcare.15,16
It is difficult to quantify the impact of managing these patients on our healthcare systems due to lack of quantifiable data.11 Despite there being literature reports showing increased rates of musculoskeletal injuries among these patients, there is still a paucity of literature locally and abroad that addresses the impact of managing these patients on orthopaedic healthcare.6,7,15 The question about the burden of managing patients with RTA-related injuries with musculoskeletal injuries to an orthopaedic department remains unanswered.
The aim of our study was to determine the overall burden of managing patients with RTA-related injuries, both financially and in terms of resource utilisation, on the orthopaedic surgery department at Steve Biko Academic Hospital. This information will help direct policy on funding prevention strategies or methods of minimising RTAs. Our study objectives were to determine the proportion of RTA patients compared to the total trauma load seen at Orthopaedics in the study period.
Methods
A retrospective, single centre study was conducted to determine the burden of RTA-related injuries treated at Steve Biko Academic Hospital, a South African tertiary hospital, over a 12-month period from February 2019 to January 2020. The departmental daily admission records were analysed for all patients assessed with trauma-related injuries during the study period. The patient population in the study included all patients who sustained trauma from RTAs. These were patients of all ages and both sexes. The proportion of this study population was compared to the total number of trauma patients seen at the orthopaedic department during the same study period.
These were further subdivided according to the modes of RTAs into motor vehicle accidents (MVAs), motorbike accidents (MBAs) and pedestrian-vehicle accidents (PVAs). We recorded the patients' demographic data, injuries sustained, injury severity, mechanism of injury, and length of hospital stay, including length of ICU/HCU stay, from the hospital records. The Injury Severity Score (ISS) was used to differentiate between polytrauma and multiply injured patients. The ISS is a score used to assess the severity of the trauma sustained by the patient and it is helpful in determining if the patient's injuries are severe. It is directly related to the length of hospital stay as well as the morbidity and mortality after the injury. Polytrauma was defined as injury to two or more major systems with an associated ISS > 15, whereas a multiply injured patient was defined as a patient with multiple injuries to different systems with minimal severity and an ISS < 15.
Radiological investigations were analysed and recorded from the patient archiving and communication system (PACS). Theatre register records were analysed for procedures performed, orthopaedic implants, number of procedures, frequency of theatre visits and duration of procedures. Duration of a procedure was calculated from the patient's sign-in time to their sign-out time. The procedures were classified into major procedures (for which orthopaedic implants were utilised) and minor procedures, including soft tissue procedures such as tendon repairs, debridement and wound closure.
The micro-costing (bottom-up) method of direct data costing was utilised for the study variables per patient. This kind of study includes calculating detailed individual costs for each patient to obtain an individual's total cost. Although it is time consuming, it gives the most accurate results compared to the top-bottom method which only takes institution average costs, dividing it by the number of patients in the study to get an average cost per patient.
The costs of radiological studies, theatre utilisation per procedure, ICU/HCU and general orthopaedic ward stays were obtained from the finance department, Uniform Patient Fee Schedule (UPFS) and Road Accident Fund (RAF) offices in the hospital. All recorded costs included facility utilisation and specialist fee for each procedure or service rendered. The costs of implants were taken from individual patients' invoices, from the implant suppliers and the government tender pricing system. All other consumables and medication were part of the facility fee as described by the UPFS, except for a few things such as vacuum-assisted closure (VAC) wound dressings and machines, braces and other forms of orthosis.
The total cost of treating RTA-injured patients from time of admission to time of discharge was derived from the total costs of emergency department (ED) consultation, the radiological studies performed, the cost of ICU and HCU utilisation, theatre utilisation costs, costs of implants and general ward admission costs per day. All the data was analysed and recorded in a Microsoft Excel spreadsheet. All the patient identifiers were removed from the data collection sheet to ensure anonymity.
Results
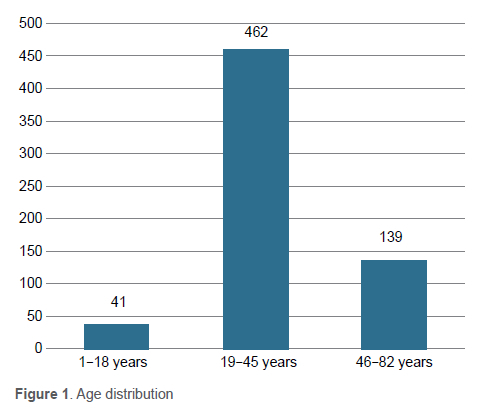
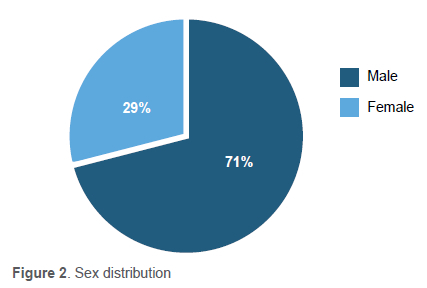
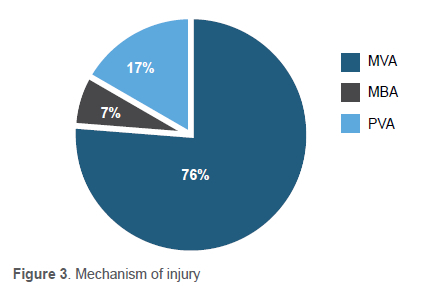
A total of 3 237 patients with trauma-related injuries were assessed at the orthopaedic department during the study period. The study cohort consisted of 642 (20%) patients who sustained RTA-related injuries. The average age of the study population patients was 35.7 years (range 1-82), with 462 (72%) patients between 19 and 45 years of age (Figure 1). Figure 2 shows there were 458 (71.3%) males and 184 (28.7%) females. MVAs were the most common modes of RTA, responsible for 76.2% of injuries, compared to PVAs (17%) and MBAs (6.8%), as shown in Figure 3.
A total of 560 (87.2%) patients were admitted for further management, while 82 (12.8%) were assessed and discharged on the day of presentation. Of the admitted patients, 124 (22%) were treated nonoperatively while ten (1.8%) patients died in hospital after admission. One hundred and twelve patients had polytrauma, 57 were multiply injured and the remainder had isolated injuries. Our 642 patients sustained a total of 870 (mean: 1.4) orthopaedic injuries.
The injuries included lower limb (LL) injuries (54.5%), upper limb (UL) injuries (36.6%) and spine injuries (9.0%) (Figures 4 and 5). One hundred and thirty patients had open injuries, 63.9% of which were open long bone fractures. Ninety-one patients had associated non-orthopaedic injuries. Four hundred and thirty-two (67.3%) patients were treated operatively, and 22.9% of them went to theatre more than once. A total of 565 (mean: 1.3) orthopaedic procedures were performed.
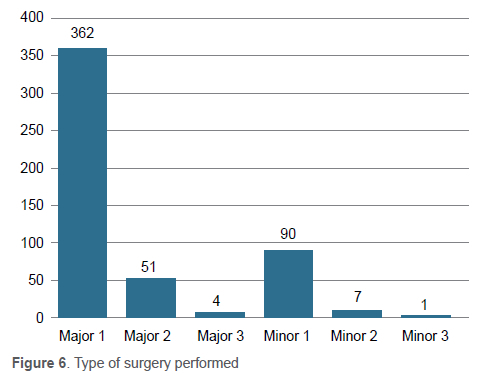
Of the 565 procedures, 362 patients had major procedures utilising 431 (mean: 1.2) orthopaedic implants. Eighty-one patients had two major operations, while 13 had three major procedures (Figure 6). The remaining 90 patients had minor procedures performed in theatre. Eight patients required more than one theatre visit. Of the 431 implants, 80 (18.6%) were external fixators used for either temporary or permanent fracture stabilisation.
The total cost spent on orthopaedic implants was R8 065 494.87, an average of R19 820.15 per patient. This amounts to 28.8% of the total hospital budget for all surgical implants, including for other orthopaedic sub-specialities. The most expensive implants were external fixators, accounting for 42% of the total implant costs utilised in the current study period.
The surgical procedures required a total surgical time of 96 854 minutes (mean: 171). This translates to 265.35 minutes, an equivalent of 4.4 hours per day. Six patients blocked theatre for an average 622.50 minutes (range: 240-1 885 minutes), while awaiting ICU/HCU bed availability. The cumulative cost of theatre utilisation was R3 363 070.00, an average of R5 952.34 per procedure and R4 578.72 per patient.
A total of 45 patients required an average ICU admission of 13 days (range: 2-50), while 71 patients required an average HCU admission of seven days (range: 2-32). Of the ICU and HCU patients, 52 patients had polytrauma with associated life-threatening non-orthopaedic injuries. The total cost of ICU stay was R12 455 820.00, an average R276 796.00 per patient, whereas total HCU costs were R4 983 808.00, an average of R70 336.00 per patient.
The initial assessment cost at the ED for the study patients was R418 584.00. All patients required at least one form of radiological study on initial assessment, whereas more studies were done during their admission period. A total of 4 920 plain radiographs, 219 skeletal survey radiographs, 75 ultrasounds, 603 CT scans, 23 MRIs and 2 677 fluoroscopic imaging were done. The total cost of radiological investigations was R4 330 613.00, an average of R6 745.50 per patient.
The admitted patients had an average length of in-hospital stay of 21.8 days. The total cost of hospital stay was R25 916 165.00, translating to R46 278.86 per patient. Total cost of treating RTA-injured patients requiring orthopaedic intervention was R59 533 555.87, which equates to R92 731.39 per patient.
The biggest cost driver for this study was hospital stay contributing 43.5%, followed by ICU/HCU costing 29.3% of the total costs (Figure 7).
Discussion
This is the first study to assess the burden of RTA injuries with specific reference to orthopaedic healthcare in South Africa. The burden was determined by assessing financial burden as well as time and resource utilisation. This tertiary hospital is one of the three public tertiary hospitals which receive trauma patients in Pretoria.
We found a high male-to-female ratio of 7.1:2.9, with an average age of 35 years. This is comparable to previous studies which reported that patients in this age group and sex engaged more in high-risk behaviour on the road.17-19 More significantly, however, we found that 72% of patients were between the ages of 19 and 45 years. These are the economically active people with musculoskeletal injuries, which take a minimum of six weeks to heal. The patients are off-duty for a significant amount of time and are unable to contribute to the economy.1
Previous studies in Africa and abroad have highlighted the disproportionate involvement of vulnerable road users such as pedestrians in RTAs. Prakash et al. found that 53% of the RTA victims were pedestrians, whereas in a South African study, Parkinson et al. reported 41% of pedestrian victims.18,20 Unlike the other studies reporting high rates of PVAs, our study found only 17% pedestrians who sustained road traffic injuries.
While previous literature reported high rates of in-patient mortality ranging between 5.6% in South Africa to 38.8% in Ethiopia following RTAs, our study found a remarkably low inpatient mortality rate of 1.78% following RTA injuries.21,22
Almost all RTA-injured patients sustain high-energy injuries, with patients having high ISS, severe musculoskeletal injuries and other life-threatening non-orthopaedic injuries. Our study found a high admission rate of 87%, 77% of whom required surgical intervention, with 21% of them having open fractures. These patients had an average of 1.3 procedures per patient, and 81 of them required more than one theatre visit. They spent an average of 171 minutes per procedure in theatre.
The average theatre utilisation for RTA trauma management was 265.35 minutes (4.4 hours), an equivalent of 18.3% theatre time per day. Although our institution runs a 24-hour emergency theatre, this is still a significant amount of time given that our emergency theatre caters for other trauma and non-trauma emergencies alike. The amount of time and frequency of theatre visits is influenced by many modifiable and non-modifiable factors.
These factors include a high ISS, multiple fractures, open fractures, life-threatening non-orthopaedic injuries and development of complications, which has a big influence on theatre utilisation, as well as on length of hospital stay. Most haemodynamically unstable patients and those with open fractures require initial debridement and temporary stabilisation before definitive management; they will therefore require more than one theatre visit.
Other factors influencing theatre times are the surgeons, anaesthetists and nursing team's experience. Most of these emergency operations are performed at night when mostly junior registrars are on call. The quality of initial debridement and fracture stabilisation will determine the subsequent frequency of theatre visits. Our tertiary hospital as a training institution has many surgeons and anaesthetists at different levels of training. This has an impact on the anaesthesia time as well as quality of debridement and surgical time.
The above factors also have an influence on ICU, HCU and length of hospital stays. Our patients had long ICU/HCU and hospital stays. This was in keeping with the injury severity, open fractures and associated life-threatening non-orthopaedic injuries reported in the current study. These findings were similar to those reported by Parkinson et al.9 Many patients also spend long periods of time in the wards for bed rest or rehabilitation before they can be safely discharged home or to rehabilitation facilities.
The long periods of hospital stay and multiple theatre visits with prolonged surgical time have an impact on orthopaedic healthcare. These patients are occupying hospital beds for protracted periods, and as a result, block the admission of other non-trauma or elective patients who require orthopaedic interventions. Prolonged theatre durations limit available theatre time for other non-trauma and non-RTA trauma patients who utilise the same theatre.
Resource utilisation, such as theatre, ICU or HCU availability and utilisation, by these patients also has a significant impact on other orthopaedic patient care. Patients with severe life- or limb-threatening injuries will always be prioritised for theatre occupancy. These patients are haemodynamically unstable and require ICU management postoperatively. An ICU/HCU bed is, on its own, a precious resource which is never readily available. These unstable patients cannot be transferred to general wards for further management.
They will essentially block the theatre while awaiting ICU bed availability. One patient blocking theatre has an enormous negative impact on other non-trauma or non-RTA orthopaedic emergency patient care. Fifty-four patients in our study blocked theatre. It took an average of 622.50 minutes, ranging between 240 minutes and 1 885 minutes. This is a significant amount of time for no operations to be done in an emergency theatre.
Radiological investigations play an integral role in the diagnosis and management of musculoskeletal injuries. These investigations contributed significantly to the resource utilisation in the patient care during their hospital stay. The majority of these patients received an average of 13.3 radiological investigations, the majority of which were ordered from the ICU/HCU complex throughout the admission period. These amounted to an average cost of R6 745.50 per patient.
With a majority of our patients sustaining high-energy injuries and multiple fractures, we recorded that 87.8% of the operated patients required an average of 1.2 orthopaedic implants. Approximately 19% of these implants were external fixators used either for temporary or permanent fracture stabilisation. The other implants included plates, screws and intramedullary devices. Implants such as K-wires were recorded as minor as they are considered part of the orthopaedic sets in hospital and are therefore classified with other theatre consumables.
Of the orthopaedic implants utilised, external fixators accounted for only 18.6% of all the implants and they were utilised in treating only 21% of the patients; however, they were responsible for 42% of the total implant costs. These findings highlight external fixators as one of the major cost drivers in orthopaedic trauma management.
Although most previous literature directs us to utilise temporary external fixation for most initial open fracture management, recent evidence supports early definitive fracture fixation which allows primary nailing for open fractures up to Gustilo-Anderson grade IIIA.23-25 As surgeons we need to start adopting new protocols which allow for early fracture fixation where possible, in order to minimise implant costs. The tibia intramedullary nail costs R8 500.00 on tender, while a temporary external fixator costs R40 000.00.
The total cost of cases in this study was R59 533 555.87, which translates to an average cost of R92 731.39 per patient and 4.4 hours in theatre per day. This cost is still high despite implementation of government tender prices for orthopaedic implants used in government institutions.
Limitations of the study include that it is a retrospective, single centre study. Polytrauma patients have other associated life-threatening injuries which influence the length of hospital stays, theatre time and management costs. We were unable to include costs of other consumable items like blood transfusions and VAC wound dressings that were utilised in the study period.
The radiographs done in ICU influence the costs spent in treating these patients. The amount of theatre time in the study reflected different levels of experience, mostly including junior doctors with minimal experience. This has a bearing on the amount of time spent in theatre, and in some cases the number of times a patient goes to theatre.
Conclusion
Road traffic accidents place a significant burden on orthopaedic patient care. There is a major financial, time and resource utilisation burden placed on orthopaedic patient care, and this has a negative impact on other non-trauma orthopaedic patients.
Minimising the use of temporary external fixation may help reduce the cost of management.
Acknowledgements
The author would like to thank the Department of Orthopaedic Surgery, Steve Biko Academic Hospital and University of Pretoria for research support. Special thanks to Prof. MV Ngcelwane for all the guidance provided throughout the study, and Steve Biko Academic Hospital for allowing me to access patients' records in order to make this study a success.
Ethics statement
The authors declare that this submission is in accordance with the principles laid down by the Responsible Research Publication Position Statements as developed at the 2nd World Conference on Research Integrity in Singapore, 2010.
The study was approved by the Research Ethics Committee, Faculty of Health Sciences, University of Pretoria with Ethics reference number: 474/2020.
All procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki
Declaration of 1975, as revised in 2008. Informed written consent was not obtained from patients for being included in this retrospective study.
Declaration
The authors declare authorship of this article and that they have followed sound scientific research practice. This research is original and does not transgress plagiarism policies.
Author contributions
NDT: conception and design, data collection, data analysis and interpretation, drafting the article, critical revision, final approval of article
MVN: conception and design, drafting the article, critical revision, final approval of article
ORCID
Thikhathali ND https://orcid.org/0000-0002-8208-5153
Ngcelwane MV https://orcid.org/0000-0001-7564-3308
References
1. Sakran JV, Greer SE, Werlin E, McCunn M. Care of the injured worldwide: trauma still the neglected disease of modern society. Scand J Trauma Resusc Emerg Med. 2012;20:64. [ Links ]
2. Saggie J. Trauma: South Africa's other epidemic. SAMJ. 2013;103:589-90. [ Links ]
3. Adeloye D, Thompson JY, Akanbi MA, et al. The burden of road traffic crashes, injuries and deaths in Africa: a systematic review and meta-analysis. Bull World Health Organ. 2016;94(7):510-21A. [ Links ]
4. Paniker J, Graham SM, Harrison JW. Global trauma: the great divide. Sicot J. 2015;1:19. [ Links ]
5. Norton R, Kobusingye O. Injuries. N Engl J Med. 2013;368(18):1723-30. [ Links ]
6. Parkinson F, Kent S, Aldous C, et al. Road traffic crashes in South Africa: the burden of injury to a regional trauma centre. S Afr Med J. 2013;103(11):850-52. [ Links ]
7. Stinner DJ, Edwards D. Surgical management of musculoskeletal trauma. Surg Clin North Am. 2017;97(5):1119-31. [ Links ]
8. Martin C, Thiart G, McCollum G, et al. The burden of gunshot injuries on orthopaedic healthcare resources in South Africa. S Afr Med J. 2017;107(7):626-30. [ Links ]
9. Parkinson F, Kent SJ, Aldous C, et al. The hospital cost of road traffic accidents at a South African regional trauma centre: a micro-costing study. Injury. 2014;45(1):342-45. [ Links ]
10. Hoogervorst P, Shearer DW, Miclau T. The burden of high-energy musculoskeletal trauma in high-income countries. World J Surg. 2020;44(4):1033-38. [ Links ]
11. Hardcastle TC, Oosthuizen G, Clarke D, Lutge E. Trauma, a preventable burden of disease in South Africa : review of the evidence, with a focus on KwaZulu-Natal. South African Health Review. 2016;2016(1):179-89. [ Links ]
12. Gnass I, Ritschel M, Andrich S, et al. Assessment of patient-reported outcomes after polytrauma: protocol for a systematic review. BMJ Open. 2018;8(3):e017571. [ Links ]
13. Laing GL, Skinner DL, Bruce JL, et al. Understanding the burden and outcome of trauma care drives a new trauma systems model. World J Surg. 2014;38(7):1699-706. [ Links ]
14. Aizpuru M, Staley C, Reisman W, et al. Determinants of length of stay after operative treatment for femur fractures. J Orthop Trauma. 2018;32(4):161-66. [ Links ]
15. Beveridge M, Howard A. The burden of orthopaedic disease in developing countries. J Bone Joint Surg Am. 2004;86(8):1819-22. [ Links ]
16. Norman R, Matzopoulos R, Groenewald P, Bradshaw D. The high burden of injuries in South Africa. Bull World Health Organ. 2007;85(9):695-702. [ Links ]
17. Lutge EE, Muirhead D. The epidemiology and cost of trauma to the orthopaedic department at a secondary-level hospital. S Afr J Surg. 2005;43(3):74-77. [ Links ]
18. Prakash I, Neves O, Cumbe E, et al. The financial burden of road traffic injuries in Mozambique: a hospital-related cost-of-illness study of Maputo Central Hospital. World J Surg. 2019;43(12):2959-66. [ Links ]
19. Turner C, McClure R. Age and gender differences in risk-taking behaviour as an explanation for high incidence of motor vehicle crashes as a driver in young males. Inj Control Saf[ Promot. 2003;10(3):123-30. [ Links ]
20. Parkinson F, Kent S, Aldous C, et al. Patterns of injury seen in road crash victims in a South African trauma centre. S Afr J Surg. 2013;51(4):131-34. [ Links ]
21. Woyessa AH, Heyi WD, Ture NH, Moti BK. Patterns of road traffic accident, nature of related injuries, and post-crash outcome determinants in western Ethiopia - a hospital based study. Afr J Emerg Med. 2021;11(1):123-31. [ Links ]
22. Saidi HS, Macharía WM, Ating'a JEO. Outcome for hospitalized road trauma patients at a tertiary hospital in Kenya. Eur J Trauma. 2005;31(4):401-406. [ Links ]
23. Poletti F, Macmull S, Mushtaq N, Mobasheri R. Current concepts and principles in open tibial fractures - Part II Management and controversies. MOJ Orthop Rheumatol. 2017;8. [ Links ]
24. Diwan A, Eberlin KR, Smith RM. The principles and practice of open fracture care, 2018. Chin J Traumatol. 2018;21(4):187-92. [ Links ]
25. Manjra M, Basson T, Du Preez G, et al. Current concepts in the management of open tibia fractures. SA Orthop J. 2019;18(4):52-62. [ Links ]
Received: July 2021
Accepted: July 2022
Published: November 2022
Editor: Prof. Sithombo Maqungo, University of Cape Town, Cape Town, South Africa
Funding: No funding was received for this study.
Conflict of interest: The authors declare they have no conflicts of interest that are directly or indirectly related to the research.
* Corresponding author: ndivho@gmail.com














