Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.21 n.3 Centurion 2022
http://dx.doi.org/10.17159/2309-8309/2022/v21n3a6
CURRENT CONCEPTS REVIEW
Wide awake local anaesthesia no tourniquet: a review of current concepts
Antoine GL RocherI, *; Megan O'ConnorI; Odette KochII
IDiscipline of Orthopaedic Surgery, University of KwaZulu-Natal, Inkosi Albert Luthuli Central Hospital, Durban, South Africa
II1 Military Hospital, Department of Orthopaedic Surgery, University of Pretoria; Netcare Pretoria East Hospital Suite M33, Pretoria, South Africa
ABSTRACT
BACKGROUND: Wide awake local anaesthesia no tourniquet (WALANT) is a local anaesthetic technique that employs lignocaine combined with adrenaline to maintain a pain-free and bloodless field during surgery on an awake patient, without the use of a tourniquet
METHODS: This article is a narrative review of the literature on the use of this mode of anaesthesia in orthopaedic and hand surgery
RESULTS: The review summarises the existing research pertaining to WALANT. It discusses the anaesthetic solution constituents, administration technique and applications of WALANT, highlighting the safety profile and benefits to patients and healthcare systems alike
CONCLUSION: The WALANT technique is safe, economical, and acceptable to patients. It should form part of the orthopaedic surgeon's armamentarium. Future research should investigate the benefits of intraoperative functional assessment of the awake patient
Level of evidence: Level 5
Keywords: WALANT, wide-awake, narrative review, current concept review, awake surgery, orthopaedic
Background
The false belief that adding adrenaline to the anaesthetic solution, when providing local blocks to the fingers or hand, will cause digital necrosis has meant that many surgeons have missed the opportunity to use a safe and cost-effective means of anaesthetic. It has been established that patients accept this mode of anaesthetic, and it has demonstrated both outcome and postoperative pain-relief benefits. The trepidation when using adrenaline with local anaesthetic originated before the 1950s when extremely acidic procaine was mixed with adrenaline, and when injected into digits, caused necrosis in some patients. Procaine becomes more acidic over time, and medicine expiry dates were not regulated at that time.
As early as the 1990s, surgeons sporadically started using lignocaine with adrenaline in hands and fingers. In the early 2000s, Dr Lalonde began popularising this method under the acronym WALANT (Wide Awake Local Anaesthetic No Tourniquet).1 The premise of WALANT as he describes, is the injection of a tumescent local anaesthetic (large volume of low concentration solution injected subcutaneously until the tissues are firm and tense), mixed with adrenaline and sodium bicarbonate, at the site of surgery. These patients do not receive sedation, nor is a tourniquet required, as the temporary vasoconstriction of the adrenaline provides a bloodless field.
Local anaesthetic mixture
Because of its relatively low toxicity, lignocaine combined with adrenaline can safely be injected in volumes of up to 7 mg per kg. Burk et al. published their experience during liposuction, where they used lignocaine volumes of up to 28 mg per kg and total adrenaline doses of up to 10 mg, with no side effects noted by either the patient or the administrator.2 Lignocaine is rapidly unbound from sodium channels when the axonal membrane is hyperpolarised during rest, and is removed from the tissue by blood flow. The vasoconstrictive action of adrenaline, however, causes delayed clearance from the site of surgery, significantly prolonging the local analgesic action of lignocaine. Lignocaine in the solution is typically diluted to 1% or less, contingent on the size of the surgical area. Concentrations as low as 0.25% lignocaine with adrenaline can provide adequate analgesia for 6-10 hours.2 In contrast to lignocaine, bupivacaine dissociates very slowly or incompletely from sodium channels, which prolongs its action, and potentially also prolongs its adverse effects.3 Bupivacaine interferes with multiple cellular functions, which can result in cardiotoxicity, which is complex to treat and often fatal.3 Patients can also experience protracted numbness after their pain sensation has returned when bupivacaine is used.4
In addition to prolonging the local effect of lignocaine, adrenaline serves to ensure a bloodless field, the safety of which has historically been questioned. Lalonde described a 1:100 000 adrenaline solution, in which a 1 ml vial of 1:1 000 adrenaline is diluted with 99 ml of saline to produce 100 ml of the mixture (any volume mixture can be reproduced provided the ratios are maintained).1 Confirmation of the safe use of adrenaline in hands and digits has been replicated in multiple studies and populations worldwide.5,6 In a prospective study, Lalonde et al. reported on 3 110 consecutive cases in which they used adrenaline in the hand and digits; 1 340 of these cases had the solution injected in their fingers.5 They measured the number of times phentolamine was required as a rescue treatment for irreversible finger necrosis, but found that this was not necessary in a single case.5 Tang et al. reported on the Nantong and Tianjin experience in China, where 12 000 cases were studied in which surgeons used adrenaline and local anaesthetic for hand surgery (involving extensive surgery in several cases such as advancement and vascularised pedicle flaps).7 They concluded that the mixture was safe, patient-friendly, economical, and found that there was no added risk of infection.7 Moog et al. performed minor digital surgeries on 17 patients using a modified WALANT solution. Articaine was used, which contains 1:200 000 adrenaline and articaine hydrochloride, and the solution was administered into the palmar base of the digits. They continuously measured tissue perfusion from just before injection up to 32 minutes after the injection. Four of the patients had short episodes of critical tissue perfusion in the period 10 to 20 minutes after injection, but all patients had normal tissue perfusion measurements after 32 minutes.8
With the safety of adrenaline established, the benefit of adrenaline providing a bloodless surgical field, and eliminating the need for a tourniquet, can be appreciated.9 The difference in blood loss, comparing the use of WALANT and other forms of anaesthesia with a tourniquet, has been extensively investigated. Farzam et al. performed a prospective trial assessing 86 patients who had hand surgery of 30 minutes or less. Forty-three patients had a below elbow Bier's block, and 43 received WALANT. None of the WALANT group needed additional analgesia or sedation, but 20% of the Bier's block group required intravenous (IV) analgesia and sedation during the procedure due to tourniquet discomfort. Furthermore, pain in the WALANT group was significantly less at one hour postoperatively.10 Davison et al. compared 200 consecutive carpal tunnel releases (CTR), in which 100 received WALANT in one centre and had an open CTR, and 100 had endoscopic CTR performed at another centre, under sedation and local lignocaine with a tourniquet. While it seems both anaesthesia modalities were equally tolerated and safe, in both groups 93% of patients stated that they would choose the same method of anaesthesia for subsequent surgery and there were no anaesthetic complications in either group, the WALANT group had a mean of 2.6 hours shorter hospital stay and required fewer postoperative opioids on average.11
The final additive to the WALANT solution is sodium bicarbonate (NaHCO3). A 1% lignocaine, with 1:100 000 adrenaline, solution has a mean pH of 4.24 (standard deviation [SD] 0.42). By adding between 1.1 and 1.8 ml of 8.5% sodium bicarbonate to a 10 ml mixture (or 10% of any volume solution), the pH is increased to a value of between 7.38 and 7.62. This is termed buffering, when an additive to a solution stabilises the solution's pH close to neutral. Buffering the WALANT solution results in a higher pH, which lessens the pain of the injection, and accelerates the onset of action of the lignocaine.12-15 A premixed lignocaine solution with adrenaline becomes more acidic over time once opened, so it is recommended that the 8.5% sodium bicarbonate be added to the lignocaine on the day of use.
Anaesthetic administration in practice and special considerations
For a typical WALANT slate in the authors' practice, comprising three or four patients with a range of pathologies including tendon lacerations, Dupuytren's contracture, trigger finger or carpal tunnel syndrome, 200 ml of the solution is prepared. The authors choose to mix a large volume at the beginning of a slate to prevent mixing the solution in haste, where ratio and dosing discrepancies are most likely to occur, one of the few risks in conducting WALANT surgery. In a stepwise fashion, 122 ml of the contents of a 200 ml bag of saline is removed, 100 ml of 2% lignocaine (intravenous-use lignocaine) is then added to the contents, along with 2 ml (two ampoules) of 1:1 000 adrenaline and 20 ml of 8.5% sodium bicarbonate. Sodium bicarbonate is added last to prevent precipitation of crystals, which occurs if sodium bicarbonate is mixed directly with the acidic lignocaine. This achieves the desired concentration ratio of 1% lignocaine, 1:100 000 adrenaline and 0.85% sodium bicarbonate solution, and can similarly be reproduced for any volume required.
At this concentration, the average 70 kg male (using 7 mg per kg as the upper dose limit for lignocaine) can receive 49 ml of the mixture, and the total 200 ml of solution would be adequate for four patients requiring the maximum volume. Figure 1 is a graphic depicting the volumes of constituents required to produce 10 ml of WALANT mixture using the same ratio, and Figure 2 is a photo of the medications and consumables the authors use locally to reconstitute 20 ml of the mixture. The solution concentration can be altered; primarily this is performed when the surgical area is extensive, such that a larger volume of solution is required. In this instance, only the lignocaine volume is altered, and the adrenaline and bicarbonate volume ratios remain unchanged. Table I lists common procedures for which the authors use the solution, and the corresponding approximate volumes and concentrations for each. The authors refer the reader to an instructional course lecture prepared by Lalonde et al. for a more detailed description, beyond the scope of this article.16

Significant bleeding during surgery has not been reported; however, it should be noted, according to a study by McKee et al., that after injecting adrenaline the surgical site takes on average 26 minutes (± 5 minutes) to reach the targeted maximum bloodless surgical field.17 While this is a considerable time to wait before conducting the surgery, the authors have learned to utilise this time to inject the following patient (so there is no delay in beginning the surgery for this patient), prepare patient paperwork and other necessary equipment, perform a surgical hand wash as well as clean and drape the patient for surgery. An additional concern when considering blood loss are those patients using chronic anticoagulation therapy. Croutzet and Guinand reported on 63 procedures performed under WALANT for patients on anticoagulation therapy (with international normalised ratios on occasion in the range 3-4) or antiaggregant therapy (clopidogrel).18 These patients underwent common hand procedures such as Dupuytren's excision, carpal tunnel release, trigger finger release and digital tumour excision. The authors reported that all the procedures were uncomplicated by bleeding, despite allowing all patients to continue their anticoagulation therapy.18
Other considerations when conducting WALANT are patient factors that could result in negative outcomes. Current literature supports the safety of WALANT for use in the hand and fingers, with fewer complications than Bier's block, sedation and local anaesthesia or general anaesthesia.19 There have, however, been isolated case reports of finger necrosis.20 One case occurred in a patient with Raynaud's disease, and other patient comorbidities included atherosclerosis, diabetes or a smoking history. In these rare instances, there was also no phentolamine rescue (alpha-blocking agent) available for reversal.20 Phentolamine or alternatives are not currently available in South Africa, so we caution surgeons to carefully evaluate patients for pre-existing peripheral vascular disease, circulatory conditions such as Buerger's or Raynaud's disease, and lignocaine allergy, prior to performing WALANT. In addition, part of the consent process should involve informing patients of the risk of digital necrosis.
Technique of injection
There are two main goals when injecting local anaesthesia. The first is to infiltrate the subcutaneous tissue of the surgical site with a large volume of diluted local anaesthesia. The second is to do this as pain-free as possible, and several techniques have been advocated to achieve this. In a meta-analysis conducted in 2011, Hogan et al. concluded that warming local anaesthesia before injection reduces the discomfort of the injection.21 The additional use of sodium bicarbonate as a buffer, discussed previously, has an even greater effect in reducing the discomfort of the injection.14 In a cleverly designed prospective study, Yang et al. compared patients who underwent bilateral axillary surgery for axilla osmidrosis across three groups.22 Group A received warm (40 °C) buffered lignocaine with adrenaline to one axilla, and cold (22 °C) buffered lignocaine with adrenaline to the opposite axilla. Group B received a warm buffered solution to one axilla, and a warm unbuffered solution on the opposite side. Group C received a warm buffered solution to one axilla and a cold unbuffered solution to the opposite axilla. The investigators assessed patients' perception of pain in each group and found significant differences. Patients had significantly less pain when injected with a warm, buffered lignocaine and adrenaline solution, as compared to the other combinations.22
In addition to solution preparation, the technique of injection has also been shown to reduce the pain experience.14 The initial injection should be at the most proximal part of the planned surgical incision, to ensure the distal nerve fibres located where subsequent injections will be administered are already anaesthetised. The clinician pinches the skin, drawing the skin onto the needle. The needle is kept perpendicular to the skin, and a subcutaneous tumescent bullous of local anaesthetic is slowly injected (Figure 3). Cognitive and sensory distraction can be performed by discussing unrelated topics with the patient and applying an ice pack proximal to the injection site. These distractions minimise the discomfort of the initial injection. The needle is then directed distally within the already numb region, and further local anaesthetic injected, advancing the anaesthetic bullous ahead of the needle tip. When blocks need to cover large areas, the injection can be performed through a single skin puncture, by replacing the short 27 G needle with a spinal or liposuction needle through the initial skin puncture. Strazar et al. discuss these and other injection techniques to make WALANT administration as comfortable as possible for patients.13,14 Utilising these methods, patients typically report pain scores of 4 or less on the visual analogue scale (VAS) for WALANT anaesthesia administration.13

WALANT soft-tissue applications and benefits
WALANT is most commonly used for minor soft tissue procedures on the hand. Lee et al. found a significant difference in pain between two similar populations, who received either WALANT or conventional local anaesthetic with a tourniquet, for either a carpal tunnel, trigger finger or De Quervain's release.23 The WALANT group, injected according to the recommended methods outlined by Strazar, had VAS scores of 4 or less on average, during the administration of anaesthesia, as compared to a VAS score of more than 6 on average for the conventional group.14,23 The WALANT group had much longer postoperative pain relief, with the most significant difference in VAS scores occurring six hours postoperatively.23 Furthermore, the WALANT group had lower VAS scores and took less analgesia postoperatively for up to two days post-surgery.23
The applications and benefits of WALANT use in common soft tissue conditions of the hand have been studied extensively, in many geographical locations and by multiple authors. The consensus is that WALANT is safe, effective and well-tolerated by patients.24 Most commonly WALANT has been investigated for carpal and cubital tunnel release;25-28 De Quervain's tenosynovectomy;23 tenolysis;29,30 and trigger finger release.31-33 The advantage of WALANT in trigger finger release and tenolysis is the immediate assessment of the release - the awake patient is asked to actively move the affected finger or joint to determine if a pulley constriction or tethering still exists. Similarly, immediate assessment of tendon repairs is especially beneficial. Assessing the tensile strength of the repair and uninterrupted gliding of the tendon is possible during WALANT anaesthesia, where active finger range of motion can be performed by the awake patient. Unresolved tendon repair gapping and pulley entrapment would otherwise result in poor outcomes, if not identified during surgery. There is also an opportunity for the surgeon to discuss the rehabilitation process with the patient, who can appreciate the functional result before postoperative pain and stiffness are experienced and while fully awake.34-36
The advantage of using WALANT during tendon transfer surgery has also been cited.34 Retraining donor motor units after tendon transfers, before the advent of WALANT, was considered a lengthy rehabilitation process.37 Bezuhly et al. and other investigators have found that the cognitive activation of the donor unit is immediate when appropriate synergistic muscles are used.34,37,38 In addition, under wide-awake conditions, the muscle tension, repair strength and excursion can immediately be assessed and altered if necessary, and the patients can witness the effect of the tendon transfer immediately.34,37,38
WALANT has also been utilised for extended soft tissue surgery applications such as local and distant flaps to cover hand and finger skin defects.7,39 Xing and Tang reported on 27 local soft tissue flap cases, for skin defect coverage, that were closely monitored by a trained nurse for five hours after surgery. One of the 27 patients was injected with phentolamine near the flap to reverse the effect of adrenaline.39 Xu et al. reported 12 cases where abdominal or thoracic flaps were effectively performed for finger skin defects utilising only lignocaine and adrenaline at both the donor and recipient sites. A notable recommendation from this paper was to take precautions when injecting, being careful to avoid anaesthetic solution entering the vascular pedicle of the flap.40 Wong et al. reported 12 cases of successful reimplantation of 12 digits using WALANT.41 Four of the patients developed superficial skin necrosis but healed without further surgery, and the remainder healed without complication.41
The use of WALANT has recently been expanded to include small joint arthroscopy. The popularity of wrist, metacarpophalangeal and interphalangeal arthroscopy is increasing, and the use of WALANT for these procedures has been reported.42 In a 2019 article, Liu et al. reported on their experience with WALANT for wrist arthroscopy. They did, however, caution that WALANT anaesthetic for arthroscopy should only be attempted by surgeons who are already proficient at wrist arthroscopy; that it is essential to select appropriate patients; and contingency plans should be in place for patients that do not tolerate the procedure. The benefits of having a fully awake patient, as proposed by the authors of this study, were that real-time kinematic assessments could be performed and that the findings could be demonstrated and discussed with the patient during the procedure.42
WALANT bony procedure applications and benefits
Common bony hand procedures, such as thumb carpometacarpal joint surgery, phalangeal fracture plating, and metalware removal from the fingers and wrist, have also been cited as appropriate indications for WALANT anaesthesia.33,43 Bony procedures require additional deep administration of solution near the periosteum for effective anaesthesia. More recently, the use of WALANT has been investigated for use in the management of certain acute fractures by open reduction and internal fixation (ORIF).44 These include in the upper limb, olecranon, distal radius and clavicle fractures.45-47 WALANT use for distal radius fracture ORIF has been investigated extensively.48-51 Abd Hamid et al. compared distal radius ORIFs performed with the use of general anaesthesia (in 32 patients) and WALANT (33 patients) respectively, in a randomised controlled trial.52 They found no statistical difference in blood loss or functional outcome. The pain during surgery for the WALANT group was minimal. Aggressive or gentle manipulation raised the average VAS score to 1; during all other surgical periods the VAS reported was zero.52 Tahir et al.'s randomised controlled trial (RCT) of 169 patents comprised three groups that compared WALANT, Bier's block or GA for distal radius ORIF. They concluded that distal radius fracture ORIF performed under WALANT was more cost effective, led to faster recovery (quicker return to light-duty work) and had fewer complications than either the GA or Bier's block groups (in which cases of tourniquet palsy, wound inflammation and local anaesthetic toxicity occurred).19
Foot and ankle surgery
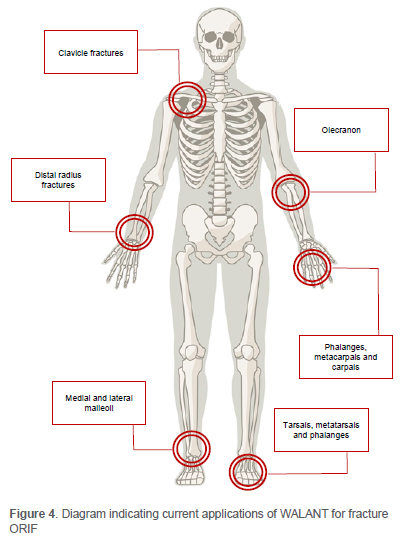
The anaesthetic requirements for peripheral lower extremity surgery seem essentially the same as those of the wrist and hand. However, using WALANT for foot and ankle surgery has not yet been researched as extensively. Bilgetekin et al. reported their experience with lateral and medial malleolus ankle fractures, toe phalangeal fractures, Lisfranc injuries, Achilles tendon ruptures, and various other bony and ligamentous injuries of the foot and ankle. They successfully treated these injuries under WALANT, without patients requiring additional anaesthesia.53 In an RCT, Borg et al. investigated 129 patients who underwent surgery for ankle fractures. Of these patients, 62 received WALANT anaesthesia and 67 received spinal anaesthesia.54 They reported that the WALANT group patients were more comfortable during surgery and more satisfied (as measured by the Short-Form Health Questionnaire SF-12) one year post-surgery, despite similar surgical outcomes in both groups, although potential reasons for this were not elaborated on. Surgery performed under WALANT was more cost-effective.54 Figure 4 depicts the current applications of WALANT for fracture fixation of the upper and lower limb.
Efficiency and cost-saving
Economic and workflow considerations are institution-specific and not easily generalisable. To make universal claims in this regard is difficult, but cost-effectiveness and efficiency are recurring themes in many WALANT articles.31,55-57 The medications and equipment required to perform WALANT are inexpensive. Furthermore, 7 mg per kg lignocaine dosing with adrenaline is safely administered without the need for routine preoperative blood testing, preoperative fasting, intraoperative IV access and intraoperative monitoring, which allows for more rapid patient turnover and cost-saving.2 Postoperative recovery room monitoring is also not needed when using WALANT anaesthesia.1
Due to the established safety of WALANT, minor surgical procedures have been performed in office side rooms and minor operating theatres, raising the concern for increased infection rates when surgery is performed in these less stringently controlled environments. In a prospective multicentre study of 1 500 cases, Leblanc et al. reported that only six patients who had carpal tunnel release surgery performed in a minor procedure room developed superficial infections, of which four required antibiotics to resolve the infection.58 None of the 1 500 patients received prophylactic antibiotics, and none developed deep postoperative infections. Furthermore, these cases were performed under field sterility, defined in the article as the surgeon applying a surgical mask, performing a surgical hand wash, and donning sterile gloves only (no gown, hair covering or shoe covering).58 The patient's arm is prepped with chlorhexidine or povidone-iodine, and only the arm is draped. Minimal draping, no gown usage, no IV-line requirements, no general anaesthetic medication, and the absence of need for monitoring disposables all result in a significant reduction in waste production, easier waste management and cost reductions.58
Low and middle-income countries (LMICs)
As surgeons in the public sector in South Africa, the authors regularly experience the frustration of scarce resources and unpredictable infrastructure, such as limited theatre access, limited availability of nursing and anaesthetic staff, and sporadic water and power shortages. Resource constraints and disruption of infrastructure interrupt not only clinical service delivery but also training. Having the hand surgery scarce skill, being reliant on an unstable infrastructure is unmerited. Holoyda et al. described the establishment of an outpatient procedure room for WALANT hand surgery in their Ghanaian hospital. They highlighted that despite the significant increase in surgical capacity afforded by the procedure room, the cost to the hospital and individual patients decreased.26 This is one of several articles from LMICs that propose WALANT anaesthetic as a means to improve access to surgery in resource-constrained settings.24,33,45,46,59
COVID-19 and the positive patient experience
Not only did the simplicity of WALANT anaesthesia lessen the burden on overwhelmed health systems, but viral spread through airway manipulation was reduced (WALANT does not require intubation), hospital stays were shortened, and many elective hand surgery procedure cancellations avoided while patient surgical experience was maintained.60-62
With the healthcare system crippled by COVID-19 and elective surgery ravaged by the lack of theatre time, the overwhelmingly positive patient experience with WALANT was the silver lining in those challenging times. WALANT was a game-changer worldwide during the peak of the pandemic. Kurtzman et al.'s review article summarises the advantages of wide-awake surgery in optimising patient satisfaction, pertinent in the context of a pandemic where accessibility to theatre is reduced and resources constrained.44 Patient-reported outcome measures such as the patients' experience and satisfaction are increasingly necessary. In a multicentre study, Davison et al. compared carpal tunnel surgeries performed with either WALANT or with a Bier's block and sedation. The wideawake group used fewer narcotics, spent less time in the facility and had less anxiety. All three of these findings emphasise the applicability of WALANT amidst a pandemic.11 Minimal pain with the WALANT procedure and high patient satisfaction rates have also been demonstrated in a local study conducted by Naude et al. Patients' mean VAS score during the procedure in this study was 0.2 (SD ± 0.7), and 100% of the study population reported a preference for the WALANT procedure in comparison to hospital admission and surgery in the main operating theatres.63 Similar positive patient experiences were reported in a study from a military medical centre in the US which reported that 73% of patients studied graded their pain scores as less painful than a dental procedure.64 So, while the COVID-19 pandemic has been the catalyst for increased use of WALANT, these positive patient experiences should incite routine use of the technique in practice.
Research opportunities
There has been ample research investigating the safety, benefits and applications of WALANT anaesthesia. In their article, Festen-Schrier and Amadio highlighted new investigative directions to pursue, particularly those where awake patients are required to perform active movement during surgery, a unique feature of WALANT.65 As an example, real-time kinematic imaging of the wrist and carpal bones is possible. In addition, they underscored that surgical outcomes can now be clearly separated from rehabilitation outcomes, proffering an interesting area for future study.65
Conclusion
There is consensus in the current literature in support of the use of WALANT for a wide range of surgical procedures. Most notably its use is advantageous on account of its established safety profile, positive patient experience and postoperative benefits, and should form part of the orthopaedic surgeon's armamentarium. Additionally, pertinent to the local context, is the accord across investigations that utilisation of the technique profits resource-constrained healthcare systems by improving cost-saving, efficiency and expansion of surgical capacity. Future investigation should be directed toward determining the benefits of intraoperative functional assessment.
Ethics statement
The authors declare that this submission is in accordance with the principles laid down by the Responsible Research Publication Position Statements as developed at the 2nd World Conference on Research Integrity in Singapore, 2010.
As this is a review article, no studies on humans or animals were conducted for this study. No ethics or institutional review board approval were required.
Declaration
The authors declare authorship of this article and that they have followed sound scientific research practice. This research is original and does not transgress plagiarism policies.
Author contributions
AGLR: literature review, first draft preparation, manuscript preparation MO: literature review, manuscript revision OK: invited local context commentary
ORCID
Rocher AGL https://orcid.org/0000-0002-9710-5591
O'Connor M https://orcid.org/0000-0001-8864-4916
Koch O https://orcid.org/0000-0003-1871-9569
References
1. Lalonde DH. Conceptual origins, current practice, and views of wide awake hand surgery. J Hand Surg Eur. 2017;42(9):886-95. https://doi.org/10.1177/1753193417728427 [ Links ]
2. Burk RW, 3rd, Guzman-Stein G, Vasconez LO. Lidocaine and epinephrine levels in tumescent technique liposuction. Plast Reconstr Surg. 1996;97(7):1379-84. https://doi.org/10.1097/00006534-199606000-00009 [ Links ]
3. Clarkson CW, Hondeghem LM. Mechanism for bupivacaine depression of cardiac conduction: fast block of sodium channels during the action potential with slow recovery from block during diastole. Anesthesiology. 1985;62(4):396-405. [ Links ]
4. Calder K, Chung B, O'Brien C, et al. Bupivacaine digital blocks: how long is the pain relief and temperature elevation? Plast Reconstr Surg. 2013;131(5):1098-104. https://doi.org/10.1097/PRS.0b013e3182865dbb [ Links ]
5. Lalonde D, Bell M, Benoit P, et al. A multicenter prospective study of 3,110 consecutive cases of elective epinephrine use in the fingers and hand: the Dalhousie Project clinical phase. J Hand Surg Am. 2005;30(5):1061-1067. https://doi.org/10.10164.jhsa.2005.05.006 [ Links ]
6. Thomson CJ, Lalonde DH, Denkler KA, et al. A critical look at the evidence for and against elective epinephrine use in the finger. Plast Reconstr Surg. 2007;119(1):260-66. https://doi.org/10.1097/01.prs.0000237039.71227.11 [ Links ]
7. Tang JB, Gong KT, Xing SG, et al. Wide-awake hand surgery in two centers in China: Experience in Nantong and Tianjin with 12,000 patients. Hand Clin. 2019;35(1):7-12. https://doi.org/10.1016pcl.2018.08.011 [ Links ]
8. Moog P, Dozan M, Betzl J, et al. WALANT-epinephrine injection may lead to short term, reversible episodes of critical oxygen saturation in the fingertips. Arch Orthop Trauma Surg. 2021;141(3):527-33. https://doi.org/10.1007/s00402-020-03744-5 [ Links ]
9. Saleh E, Saleh J, Govshievich A, et al. Comparing minor hand procedures performed with or without the use of a tourniquet: a randomized controlled trial. Plast Reconstr Surg Global Open. 2021;9(4):e3513. https://doi.org/10.1097/gox.0000000000003513 [ Links ]
10. Farzam R, Deilami M, Jalili S, et al. Comparison of anesthesia results between wide awake local anesthesia no tourniquet (WALANT) and forearm tourniquet bier block in hand surgeries: a randomized clinical trial. Arch Bone Jt Surg. 2021;9(1):120-25. https://doi.org/10.22038/abjs.2020.49526.2487 [ Links ]
11. Davison PG, Cobb T, Lalonde DH. The patient's perspective on carpal tunnel surgery related to the type of anesthesia: a prospective cohort study. Hand. 2012;8(1):47-53. https://doi.org/10.1007/s11552-012-9474-5 [ Links ]
12. Schwarz W, Palade PT, Hille B. Local anesthetics. Effect of pH on use-dependent block of sodium channels in frog muscle. Biophys J. 1977;20(3):343-68. https://doi.org/10.1016/S0006-3495(77)85554-9 [ Links ]
13. Steiner MM, Calruccio JH. Use of wide-awake local anesthesia no tourniquet in hand and wrist surgery. Orthop Clin North Am. 2018;49(1):63-68. https://doi.org/10.1016/j.ocl.2017.08.008 [ Links ]
14. Strazar AR, Leynes PG, Lalonde DH. Minimizing the pain of local anesthesia injection. Plast Reconstr Surg. 2013;132(3):675-84. https://doi.org/10.1097/PRS.0b013e31829ad1e2 [ Links ]
15. Frank SG, Lalonde DH. How acidic is the lidocaine we are injecting, and how much bicarbonate should we add? Can J Plast Surg. 2012;20(2):71-73. https://doi.org/10.1177/229255031202000207 [ Links ]
16. Lalonde DH, Eaton C, Amadio P, et al. Wide-awake hand and wrist surgery: a new horizon in outpatient surgery. Instr Course Lect. 2015;64:249-59. [ Links ]
17. McKee DE, Lalonde DH, Thoma A, et al. Optimal time delay between epinephrine injection and incision to minimize bleeding. Plast Reconstr Surg. 2013;131(4):811-14. https://doi.org/10.1097/PRS.0b013e3182818ced [ Links ]
18. Croutzet P, Guinand R. Maintaining anticoagulant treatmentin hand surgery - a review of 63 procedures. Hand Surg Rehabil. 2017;36(6):428. https://doi.org/10.1016/j.hansur.2017.10.008 [ Links ]
19. Tahir M, Chaudhry EA, Zaffar Z, et al. Fixation of distal radius fractures using wide-awake local anaesthesia with no tourniquet (WALANT) technique A randomized control trial of a cost-effective and resource-friendly procedure. Bone Joint Res. 2020;9(7):429-39. https://doi.org/10.1302/2046-3758.97.bjr-2019-0315.r1 [ Links ]
20. Zhang JX, Gray J, Lalonde DH, et al. Digital necrosis after lidocaine and epinephrine injection in the flexor tendon sheath without phentolamine rescue. J Hand Surg Am. 2017;42(2):e119-23. https://doi.org/10.10164.jhsa.2016.10.015 [ Links ]
21. Hogan ME, VanderVaart S, Perampaladas K, et al. Systematic review and meta-analysis of the effect of warming local anesthetics on injection pain. Ann Emerg Med 2011;58(1):86-98 e81. https://doi.org/10.1016/j.annemergmed.2010.12.001 [ Links ]
22. Yang CH, Hsu HC, Shen SC, et al. Warm and neutral tumescent anesthetic solutions are essential factors for a less painful injection. Dermatol Surg. 2006;32(9):1119-22. https://doi.org/10.1111/j.1524-4725.2006.32254.x [ Links ]
23. Lee SK, Gul Kim S, Sik Choy W. A randomized controlled trial of minor hand surgeries comparing wide awake local anesthesia no tourniquet and local anesthesia with tourniquet. Orthop Traumatol Surg Res. 2020;106(8):1645-51. https://doi.org/10.10164.otsr.2020.03.013 [ Links ]
24. Gunasagaran J, Sean ES, Shivdas S, et al. Perceived comfort during minor hand surgeries with wide awake local anaesthesia no tourniquet (WALANT) versus local anaesthesia (LA)/tourniquet. J Orthop Surg (Hong Kong). 2017;25(3): 2309499017739499. https://doi.org/10.1177/2309499017739499 [ Links ]
25. Farkash U, Bain O, Sagiv P, et al. A radical innovative change in the practice of hand surgery using wide awake local anesthesia. Acta Orthop Belg. 2020;86:37-41. [ Links ]
26. Holoyda KA, Farhat B, Lalonde DH, et al. Creating an outpatient, local anesthetic hand operating room in a resource-constrained Ghanaian hospital builds surgical capacity and financial stability. Ann Plast Surg. 2020;84(4):385-89. https://doi.org/10.1097/sap.0000000000002196 [ Links ]
27. Kang SW, Park HM, Park JK, et al. Open cubital and carpal tunnel release using wide-awake technique: reduction of postoperative pain. J Pain Res. 2019;12:2725-31. https://doi.org/10.2147/jpr.s210366 [ Links ]
28. Nikkhah D, Ruston J, Pearl R, et al.'WALANT carpal tunnel release: Technical considerations and pain outcomes'. J Plast Reconstr Aesthet Surg. 2019;72(9):1576-606. https://doi.org/10.1016/j.bjps.2019.05.014 [ Links ]
29. Woo SH, Yoo MJ, Ahn HC. Lessons learned in the authors' first years of wide-awake hand surgery at the W Hospital in Korea. Hand Clin. 2019;35(1):59-66. https://doi.org/10.10164.hcl.2018.08.006 [ Links ]
30. Pires Neto PJ, Ribak S, Sardenberg T. Wide awake hand surgery under local anesthesia no tourniquet in South America. Hand Clin. 2019;35(1):51-58. https://doi.org/10.1016/j.hcl.2018.08.005 [ Links ]
31. Codding JL, Bhat SB, Ilyas AM. An economic analysis of MAC versus WALANT: a trigger finger release surgery case study. Hand (NY). 2107;12(4):348-51. https://doi.org/10.1177/1558944716669693 [ Links ]
32. Gil JA, Hresko AM, Weiss AC. Current concepts in the management of trigger finger in adults. J Am Acad Orthop Surg. 2020;28(15):e642-50. https://doi.org/10.5435/jaaos-d-19-00614 [ Links ]
33. Mohd Rashid MZ, Sapuan J, Abdullah S. A randomized controlled trial of trigger finger release under digital anesthesia with (WALANT) and without adrenaline. J Orthop Surg (Hong Kong). 2019;27:2309499019833002. https://doi.org/10.1177/2309499019833002 [ Links ]
34. Lalonde D, Martin A. Tumescent local anesthesia for hand surgery: improved results, cost effectiveness, and wide-awake patient satisfaction. Arch Plast Surg. 2014;41(4):312-16. https://doi.org/10.5999/aps.2014.4L4.312 [ Links ]
35. Lalonde DH. Latest advances in wide awake hand surgery. Hand Clin. 2019;35(1):1-6. https://doi.org/10.1016/j.hcl.2018.08.002 [ Links ]
36. Tang JB. Flexor tendoninjuries. Clin Plast Surg. 2019;46(3):295-306. https://doi.org/10.1016/j.cps.2019.02.003 [ Links ]
37. Bezuhly M, Sparkes GL, Higgins A, et al. Immediate thumb extension following extensor indicis proprius-to-extensor pollicis longus tendon transfer using the wide-awake approach. Plast Reconstr Surg. 2007;119(5):1507-12. https://doi.org/10.1097/01.prs.0000256071.00235.d0 [ Links ]
38. Mohammed AK, Lalonde DH. Wide Awake tendon transfers in leprosy patients in India. Hand Clin. 2019;35(1):67-84. https://doi.org/10.1016pcl.2018.09.001 [ Links ]
39. Xing SG, Tang JB. Extending applications of local anesthesia without tourniquet to flap harvest and transfer in the hand. Hand Clin. 2019;35(1):97-102. https://doi.org/10.1016/j.hcl.2018.08.009 [ Links ]
40. Xu JH, Yin L, Cao SM, et al. Application of WALANT technique for repairing finger skin defect with a random skin flap. J Orthop Surg Res. 2021;16(1):164. https://doi.org/10.1186/s13018-021-02319-3 [ Links ]
41. Wong J, Lin CH, Chang NJ, et al. Digital revascularization and replantation using the wide-awake hand surgery technique. J Hand Surg Eur. 2017;42(6):621-25. https://doi.org/10.1177/1753193417703516 [ Links ]
42. Liu B, Ng CY, Arshad MS, et al. Wide-awake wrist and small joints arthroscopy of the hand. Hand Clin. 2019;35(1):85-92. https://doi.org/10.1016/jhcl.2018.08.010 [ Links ]
43. Kritiotis C, Phillips A, Muir L, et al. Practice in wide-awake hand surgery: differences between United Kingdom and Cyprus. Hand Clin. 2019;35(1):43-50. https://doi.org/10.1016/j.hcl.2018.08.007 [ Links ]
44. Kurtzman JS, Etcheson JI, Koehler SM. Wide-awake local anesthesia with no tourniquet: an updated review. Plast Reconstr Surg Glob Open. 2021;9(3):e3507. https://doi.org/10.1097/gox.0000000000003507 [ Links ]
45. Ahmad AA, Sabari SS, Ruslan SR, et al. Wide-awake anesthesia for olecranon fracture fixation. Hand (N Y). 2021;16(3):402-406. https://doi.org/10.1177/1558944719861706 [ Links ]
46. Ahmad AA, Kamal MAUM, Ruslan SR, et al. Plating of clavicle fracture using the wide-awake technique. J Shoulder Elbow Surg. 2020;29(11):2319-25. https://doi.org/10.1016/j.jse.2020.03.003 [ Links ]
47. Niempoog S, Tanariyakul Y, Jaroenporn W. Wide-awake local anesthesia for clavicle fracture fixation: A case report. Int J Surg Case Rep. 2021;79:112-15. https://doi.org/10.1016/j.ijscr.2021.01.005 [ Links ]
48. Abitbol A, Merlini L, Masmejean EH, et al. Applying the WALANT technique to surgical treatment of distal radius fractures. Hand Surg Rehabil. 2021;40(3):277-82. https://doi.org/10.1016/j.hansur.2021.02.001 [ Links ]
49. Ahmad AA, Yi LM, Ahmad AR. Plating of distal radius fracture using the wide-awake anesthesia technique. J Hand Surg Am. 2018;43(11):1045. https://doi.org/10.1016/j.jhsa.2018.03.033 [ Links ]
50. Huang YC, Hsu CJ, Renn JH, et al. WALANT for distal radius fracture: open reduction with plating fixation via wide-awake local anesthesia with no tourniquet. J Orthop Surg Res. 2018;13(1):195. https://doi.org/10.1186/s13018-018-0903-1 [ Links ]
51. Orbach H, Rozen N, Rubin G. Open reduction and internal fixation of intra-articular distal radius fractures under wide-awake local anesthesia with no tourniquet. J Int Med Res. 2018;46(10):4269-76. https://doi.org/10.1177/0300060518793036 [ Links ]
52. Abd Hamid MH, Abdullah S, Ahmad AA, et al. A randomized controlled trial comparing wide-awake local anesthesia with no tourniquet (WALANT) to general anesthesia in plating of distal radius fractures with pain and anxiety level perception. Cureus. 2021;13(1):e12876. https://doi.org/10.7759/cureus.12876 [ Links ]
53. Bilgetekin YG, Kuzucu Y, Oztiirk A, et al. The use of the wide-awake local anesthesia no tourniquet technique in foot and ankle injuries. Foot Ankle Surg. 2021;27(5):535-38. https://doi.org/10.1016/j.fas.2020.07.002 [ Links ]
54. Borg TM, Tahir M, Heidari N. The use of a wide-awake local anaesthesia no tourniquet (WALANT) technique in foot and ankle procedures - a randomised control trial. Br J Surg. 2021;108(Supple 2):znab134.456. https://doi.org/10.1093%2Fbjs%2Fznab134.456 [ Links ]
55. Leblanc MR, Lalonde J, Lalonde DH. A detailed cost and efficiency analysis of performing carpal tunnel surgery in the main operating room versus the ambulatory setting in Canada. Hand (N Y). 2007;2(4):173-78. https://doi.org/10.1007/s11552-007-9043-5 [ Links ]
56. Alter TH, Warrender WJ, Liss FE, et al. A cost analysis of carpal tunnel release surgery performed wide awake versus under sedation. Plast Reconstr Surg. 2018;142(6):1532-38. https://doi.org/10.1097/prs.0000000000004983 [ Links ]
57. Kamal RN, Behal R. Clinical care redesign to improve value in carpal tunnel syndrome: a before-and-after implementation study. J Hand Surg Am. 2019;44(1):1-8. https://doi.org/10.1016/j.jhsa.2018.09.013 [ Links ]
58. Leblanc MR, Lalonde DH, Thoma A, et al. Is main operating room sterility really necessary in carpal tunnel surgery? A multicenter prospective study of minor procedure room field sterility surgery. Hand (N Y). 2011;6(1):60-63. https://doi.org/10.1007/s11552-010-9301-9 [ Links ]
59. Ahmad TS, Ahmad AA, Abdullah S. Hand surgery in Malaysia. J Hand Microsurg. 2021;13(1):21-26. https://doi.org/10.1055/s-0040-1721942 [ Links ]
60. Hobday D, Welman T, O'Neill N, et al. A protocol for wide awake local anaesthetic no tourniquet (WALANT) hand surgery in the context of the coronavirus disease 2019 (COVID-19) pandemic. Surgeon. 2020;18(6):e67-e71. https://doi.org/10.1016/j.surge.2020.06.015 [ Links ]
61. Turcotte JJ, Gelf JM, Jones CM, et al. Development of a low-resource operating room and a wide-awake orthopedic surgery program during the COVID-19 pandemic. Surg Innov. 2021;28(2):183-88. https://doi.org/10.1177/15533506211003530 [ Links ]
62. Turcotte JJ, Petre BM, Jones CM, et al. Maintaining access to orthopaedic surgery during periods of operating room resource constraint: expanded use of wide-awake surgery during the COVID-19 pandemic. J Am Acad Orthop Surg Glob Res Rev. 2020;4(12):e20.00100. https://doi.org/10.5435/jaaosglobal-d-20-00100 [ Links ]
63. Naude JJ, Koch O, Schmidt LW, et al. Positive patient experience of wide awake local anaesthesia no tourniquet (WALANT) hand surgery in the government setting: a prospective descriptive study. SA Orthop J. 2021;20(3):141-46. http://dx.doi.org/10.17159/2309-8309/2021/v20n3a1 [ Links ]
64. Rhee PC, Fischer MM, Rhee LS, et al. Cost savings and patient experiences of a clinic-based, wide-awake hand surgery program at a military medical center: a critical analysis of the first 100 procedures. J Hand Surg Am. 2017;42(3):e139-47. https://doi.org/10.10164.jhsa.2016.11.019 [ Links ]
65. Festen-Schrier VJMM, Amadio PC. Wide awake surgery as an opportunity to enhance clinical research. Hand Clin. 2019;35(1):93-96. https://doi.org/10.1016/j.hcl.2018.08.003 [ Links ]
Received: December 2021
Accepted: May 2022
Published: August 2022
* Corresponding author: rocher@ukzn.ac.za
Editor: Dr Ajmal Ikram, Stellenbosch University, Cape Town, South Africa
Funding: No funding was received for this study.
Conflict of interest: The authors declare they have no conflicts of interest that are directly or indirectly related to the research.














