Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.21 n.3 Centurion 2022
http://dx.doi.org/10.17159/2309-8309/2022/v21n3a4
HIP
Short-term outcomes of one-stage bilateral total hip arthroplasty in a South African setting
Sayed M MiaI, *; Jitesh RajpaulI; Ismail E GogaII
IDepartment of Orthopaedic Surgery, Inkosi Albert Luthuli Central Hospital, University of KwaZulu-Natal, Durban, South Africa
IIOrthopaedic surgeon, Nu Shifa Hospital, Durban, South Africa
ABSTRACT
BACKGROUND: Total hip arthroplasty (THA) is one of the most successful orthopaedic surgical procedures that dramatically improves function, pain relief and quality of life for the patient. In South Africa, we have a high prevalence of osteonecrosis of the femoral head (ONFH) and inflammatory arthropathy affecting a young population. This subgroup of patients is usually between the ages of 30 and 50 years (young) and they require bilateral total hip replacements (BTHA) to allow them to return to their previous level of function and employment. The study aimed to assess the short-term outcomes and complications in patients with bilateral hip pathology managed surgically with a one-stage BTHA
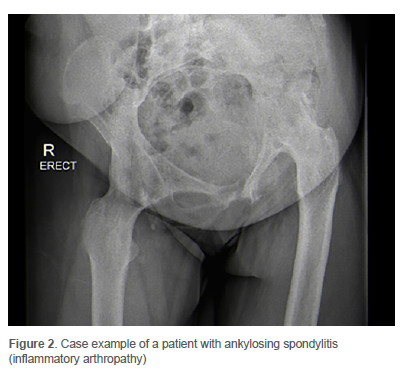
METHODS: We retrospectively reviewed a series of 33 patients who underwent a one-stage BTHA at a high-volume arthroplasty unit in a central hospital in South Africa between January 2016 and December 2018. The mean age was 38 years (standard deviation [SD] 9 years), and the most common diagnosis was ONFH (76%). In this cohort, 12 patients (36%) tested HIV positive. We assessed patient folders for diagnosis, perioperative details, postoperative follow-up and complications. Radiographic analysis was also performed
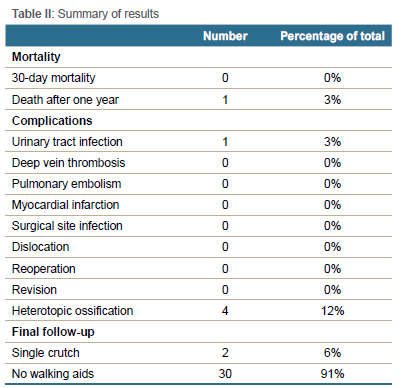
RESULTS: There were no revisions or planned surgical interventions for any of the patients at a median follow-up of 22 months (interquartile range [IQR] 11-45 months). Thirty patients reported no hip pain and walked unaided at their most recent follow-up visit. Two patients reported groin pain and continued to walk with a single crutch. One patient demised from unrelated causes approximately one year post-surgery. The only perioperative complication was a urinary tract infection (UTI) in one patient. The median postoperative length of stay was six days (IQR 4-7 days), and no other medical or surgical complications were reported. Radiographic analysis revealed four patients (12%) with Brooker grade 1 heterotopic ossification in six hips
CONCLUSION: Our results suggest that surgical treatment with a one-stage BTHA is a good alternative to a two-stage BTHA when performed in a high-volume arthroplasty centre and carefully selected patients. The 30-day mortality rate was 0%, and the complication rate was low
Level of evidence: Level 4
Keywords: one-stage bilateral total hip arthroplasty, two-stage bilateral total hip arthroplasty, simultaneous bilateral total hip arthroplasty, bilateral osteonecrosis of the femoral head
Introduction
Total hip arthroplasty (THA) is one of the most successful orthopaedic surgical procedures that dramatically improves function, pain relief and quality of life for the patient. A wide range of pathology affects the hip joint in our population, including osteoarthritis, osteonecrosis of the femoral head (ONFH), inflammatory arthropathy and infection.
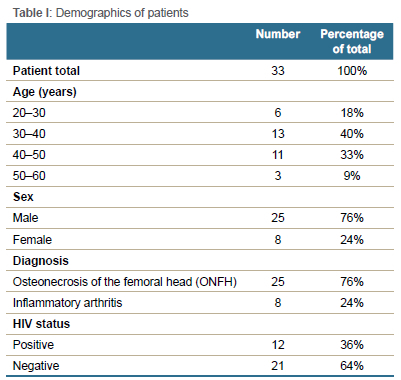
In South Africa, we have a high prevalence of ONFH affecting a young population, and the aetiology is varied. One of the postulated causes is the chronic use of antiretroviral drugs; however, it is unclear whether antiretroviral medication or the human immunodeficiency virus (HIV) itself is responsible for the pathogenesis of ONFH.1 Despite the significant progress in the rollout of antiretroviral drugs, South Africa has one of the highest incidences of HIV globally.2 We treat many patients with advanced bilateral ONFH (Steinberg stage IV-VI disease3). This subgroup of patients is usually between 30 and 50 years (young) and they require bilateral total hip replacements (BTHA) to allow them early return to their previous level of function and employment.4
A two-stage BTHA encompasses a lengthy period of morbidity and rehabilitation for the patient, which can sometimes span up to five years in our public healthcare system due to the high burden of disease and limited theatre time. Staged BTHA involves an initial admission where a unilateral hip replacement is performed on the most severely affected hip. Due to the pain, disability and contracture of the opposite unoperated hip, rehabilitation is usually slow. The contralateral THA is often performed after six months to one year, and the patient must undergo further rehabilitation to regain their function. Due to this prolonged treatment method, patients often do not return to work and depend on the state for a disability grant to support their families.
A one-stage BTHA is performed during a single admission, whereby THA is performed on both hips at the same theatre setting. The advantage of this method of treatment is a faster recovery and an earlier return to previous function.4,5 With this in mind, we retrospectively reviewed a cohort of patients who underwent a one-stage BTHA with the aims to evaluate the perioperative details; the early in-hospital complications; the early clinical outcomes; the radiographic outcomes; and the need for revision surgery.
Materials and methods
Following ethical approval, we identified all patients presenting for THA at an arthroplasty unit in a hospital in South Africa, over two years (January 2016 to December 2018). All patients who underwent a unilateral THA or a two-stage BTHA were excluded. We included a total of 33 patients who underwent a one-stage BTHA and assessed patient folders for demographics, diagnosis, perioperative details, postoperative follow-up and complications.
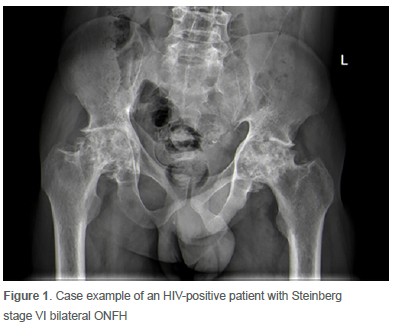
The cohort (Table I) included eight females and 25 males, with a mean age of 38 years (SD ± 9 years). The aetiology was ONFH (Figure 1) in 25 patients (76%) and inflammatory arthritis (Figure 2) in eight patients (24%). The anaesthesiologist graded all 33 patients as American Society of Anesthesiologists (ASA) class I or II.
Surgical workflow
All surgical procedures were performed using the posterior hip approach in the lateral decubitus position. Two senior fellowship-trained arthroplasty surgeons were the primary and assistant surgeons in all cases. General anaesthesia (GA), regional anaesthesia (epidural), regional nerve blocks or a combination of the above were used depending on the case's complexity. All patients received a collarless, fully hydroxyapatite-coated, pressfit stem (Corail®, De Puy International Ltd.) and a hemispherical porous-coated press-fit acetabular cup (De Puy International Ltd.).
Intravenous antibiotic prophylaxis (1 g cefazolin) was administered preoperatively and three doses on the first day postoperatively. The thromboprophylaxis protocol included postoperative subcutaneous low molecular weight heparin (enoxaparin 0.5 mg/kg) until discharge from the hospital and aspirin 150 mg to take home for a total duration of four weeks. Full weight-bearing was allowed from the day after surgery, and the patient initially mobilised with a walker with progression to crutches as tolerated. Clinical follow-up was expected at six weeks, six months and yearly after that. An anteroposterior pelvis X-ray was taken on day one post-surgery and at the six-week follow-up visit. These radiographs served as a reference for follow-up films.
Radiographs
The authors independently evaluated the early postoperative and most recently available anteroposterior X-rays. Linear and angular measurements were taken using Siemens Syngo.plaza Picture Archiving and Communication System (PACS), and the following radiographic features were recorded:
1. Acetabular component position: measured as the angle between the inter-teardrop line and the inclination of the cup in degrees. Outliers were identified according to the safe zone defined by Lewinnek et al.6
2. Limb length discrepancy (LLD): The difference in perpendicular distance between the inter-teardrop line to the corresponding tip of the lesser trochanter of both hips were measured in millimetres.
3. Heterotopic ossification graded according to Brooker et al.7
Patient data
We reviewed all patient's electronic medical records on the hospital software Meditech Health Care Information System to extract the following data: diagnosis, age, sex, length of stay (LOS), HIV status, CD4 cell count, preoperative haemoglobin, postoperative haemoglobin, operative time, anaesthetic details, and complications (such as urinary tract infection [UTI], deep vein thrombosis [DVT], pulmonary embolism [PE], myocardial infarction [MI], surgical site infection [SSI], dislocation, heterotopic ossification [HO] and revision).
Statistical methods
Statistical analysis was performed using jamovi version 2.0 (The jamovi project [2021]. Retrieved from https://www.jamovi.org). Continuous variables were reported as mean (± standard deviation [SD]) if normally distributed, or median (interquartile range [IQR]) if skewed, and categorical variables as numbers and percentages, unless otherwise stated. P-values of less than 0.05 were considered significant.
Results
Patients
A one-stage BTHA was performed on 33 patients (a total of 66 total hip arthroplasties) over two years (January 2016 to December 2018). The median follow-up period was 22 months (IQR 11-45 months). Twenty-four patients had completed a minimum of 12 months of clinical follow-up, and of these, 22 remained pain-free and walked unaided on their last follow-up visit. In this subgroup, one patient diagnosed with ankylosing spondylitis (Figure 2) complained of persistent groin pain with no radiographic or haematological changes to suggest loosening or infection (Figure 3). Another patient reported acute onset right hip pain after lifting a heavy object at work. His radiographs at his five-year follow-up visit revealed no change in position of the implants and the formation of Brooker grade 1 heterotopic ossification. His symptoms resolved after a short course of non-steroidal anti-inflammatory medication.

The remaining nine patients did not complete a minimum of one-year follow-up period, and of this group, seven reported no complications, were pain-free and walked without assistance. One patient (eight months post-surgery) complained of left hip pain and was using a single crutch to mobilise; however, he defaulted his subsequent follow-up appointment, suggesting that he did not have any further complications.
One patient demised from unrelated causes approximately one year post-surgery.
Thirty-six per cent of patients were HIV positive (n = 12 of 33) with a median CD4 cell count of 497 cells/mm3 (IQR 422-650 cells/mm3). All the HIV-positive patients were operated on for a diagnosis of ONFH with no other identifiable risk factors, and there were no complications reported.
Despite good pain relief and restoration of function in most cases, six patients (18%) requested a state disability grant application at their most recent follow-up visit.
Perioperative period
Eighteen patients (55%) received a combined GA and epidural while the remainder received either a GA (21%), epidural (12%) or a combined GA and a regional nerve block (12%). There were no anaesthetic complications reported. The mean theatre time (anaesthesia and surgical procedure time) was 182 minutes (SD ± 30 minutes), and the mean surgical procedure time (skin incision on the first hip to skin closure on the second hip) was 143 minutes (SD ± 26 minutes). The mean preoperative haemoglobin level was 13.60 g/dL (SD ± 1.57 g/dL). Seven patients (21%) received an average of two units of blood transfusion postoperatively, and the mean post-surgery haemoglobin level was 9.86 g/dL (SD ± 1.67 g/dL).
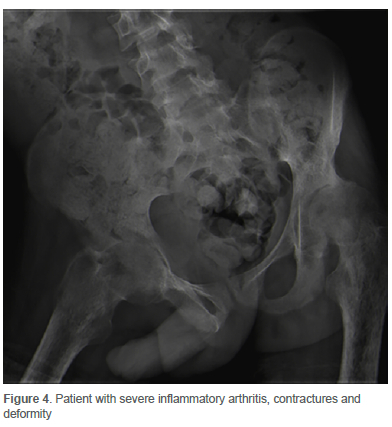
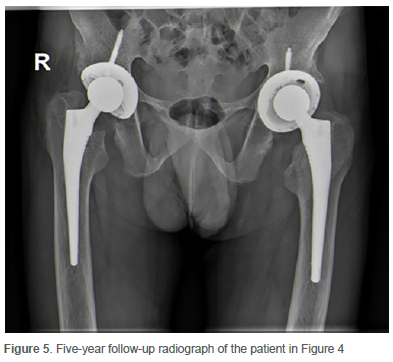
The median postoperative length of stay (LOS) was six days (IQR 4-7 days). The longest postoperative LOS of 16 days was in a patient with severe ankylosing spondylitis (Figure 2) due to multiple joint involvement and prolonged rehabilitation. Another patient with severe inflammatory arthritis (Figure 4) had a prolonged hospital stay of 14 days post-surgery due to a UTI, which resolved with intravenous antibiotic therapy. This patient was bedridden for several months prior to surgery with severe contracture and deformity. He was admitted on skin traction at a peripheral hospital before he could receive his one-stage BTHA. At the patient's most recent clinical assessment (five-year follow-up), he remains pain-free, walks unaided, and his implant position remains unchanged (Figure 5). In all other patients, no other medical or surgical complications were reported (Table II). There were no perioperative (30-day mortality) deaths.
Radiographs
Of the 25 patients with ONFH, 20 were graded as Steinberg stage VI, and five patients as Steinberg stage V. The median acetabular inclination angle of the right hip on the anteroposterior radiograph was 40° (IQR 38-45°) and of the left hip 41° (IQR 39-46°). On follow-up radiographs, none of the cups had migrated, and there was no periacetabular osteolysis evident. A total of seven hips in seven patients had an increased acetabular inclination angle outside the safe zone (> 50°) as described by Lewinnek et al.; however, none of these patients had an episode of hip instability.6 The mean LLD was 0.49 mm (SD ± 0.32 mm), and there was no evidence of femoral osteolysis around the femoral component in all patients. Four radiographs (12%) demonstrated heterotopic ossification in six hips, all classified as Brooker grade 1.
Revision
At the last clinical review, none of the patients had undergone revision surgery or required further surgical intervention.
Discussion
A unilateral THA has been shown to provide good pain relief, improve function, and be reliably performed with minimal complications. When performing a two-stage BTHA, patients have a prolonged rehabilitation period after their first surgical procedure as they await their second procedure with a painful and stiff hip. The advantages of a one-stage BTHA include a theoretical reduction in anaesthetic risk (single anaesthetic versus two), a shorter rehabilitation period, decreased costs to the healthcare system and an earlier return to work.8-10
Despite this, there are several concerns regarding the safety of a one-stage BTHA due to the reported increase in complication rates and the lack of evidence in the literature.10-12 In the United States, over 2 million THAs were performed between 2002 and 2010, and only less than 1% was a one-stage BTHA.13 The annual incidence of primary THA is increasing exponentially. It is forecast that about 500 000 procedures will be performed in the United States in 2030.8 It is essential to risk-stratify patients for a one-stage BTHA to improve the efficiency and outcomes of the arthroplasty service worldwide. This is especially pertinent in a developing country due to the limited resources and the long waiting periods for elective arthroplasty surgery.
The decision as to which patients to perform a one-stage BTHA on is controversial due to the historical reporting of increased medical complications such as thromboembolic events, myocardial infarction (MI) and chest infections. Data obtained between 2005 and 2014 from England's National Health Service (NHS) revealed an overall more significant risk of pulmonary embolism, MI, renal failure, chest infection and mortality. When they performed a subgroup analysis, patients younger than 60 years with no comorbidities had a comparable complication rate in both groups. When the one-stage BTHA was performed at a high-volume arthroplasty centre, the complication rate was also reduced. The authors recommended a rigorous patient selection process and preferably high-volume surgeons to perform the procedure to minimise the risks for the patient.10 Flick et al. reported low complication rates in a group of 730 patients, and they considered the use of a simultaneous BTHA a safe and effective procedure in patients with appropriate comorbidities.14 A retrospective cohort study by Guo et al. showed an increased complication rate in their staged group compared to their simultaneous BTHA group, particularly for superficial infection and dislocation.15
Only one patient suffered an acute complication (UTI) post-surgery in our study, which resolved with antibiotic therapy. Low-risk, young patients (ASA I and ASA II) were selected for a one-stage BTHA, which is in keeping with the above recommendations. Thirty-six per cent of patients in this study were HIV positive; however, in this subgroup, we did not find any perioperative complications or an increase in the incidence of surgical site infection. Similar results between HIV-positive and -negative patients are in keeping with a recent study by Ngwazi et al.16
Several authors have highlighted a similar mortality rate between one-stage BTHA and two-stage BTHA. Kim et al. reported a perioperative mortality rate of 0.31% (three patients out of 978) in their simultaneous group compared to 0.18% (three patients out of 1 666) in their two-stage group.17 Experience from the Australian Orthopaedic Association National Joint Replacement Registry revealed a higher mortality rate in the one-stage group (0.18%) versus the two-stage group (0.06%); however, they recommend simultaneous BTHA as the absolute incidence of 30-day mortality is low.11
The 30-day mortality rate in our study was 0%, and only one patient demised from unknown causes one year post-surgery. This highlights the safety of this procedure in young, medically fit patients with severe bilateral hip pathology, especially when performed in a high-volume arthroplasty centre.
Many studies have demonstrated a reduced cost to the healthcare system when performing a one-stage BTHA.5,10,12,18,19 Rolfson et al. calculated both direct medical and indirect non-medical costs for a one-stage BTHA and a two-stage BTHA. Their study, which was carried out in Sweden, compared 32 patients in both groups and the authors used the EQ-5D questionnaire as a health-related quality of life (HRQOL) instrument. The average cost per patient in the one-stage group was 14 470 euros compared to 9 060 euros per hip for the two-stage group. The one-stage BTHA was approximately 3 650 euros cheaper (25%), and the authors noted a significant increase in the HRQOL. Sick-leave cost reduction was also calculated to be roughly 30%.12,18 Micicoi et al. also estimated a total hospital cost reduction of 25-30%.18
A contrasting study by Phillips et al. showed no difference in the total episode-of-care cost between a one-stage and a two-stage bilateral total joint replacement (BTJA) at 90 days. The more significant inpatient costs associated with two hospital admissions were offset by the greater post-acute care costs in the one-stage BTJA group. They cautioned against simultaneous BTJA in older patients with a history of stroke, cardiac disease or liver disease.20
In our cohort, the median postoperative length of stay of six days (IQR 4-7 days), the low complication rate, and the reduction in the number of patient hospital visits (post-acute care costs), suggests that the overall cost was reduced; however, we did not have a comparison group, and a cost data analysis was not performed. Due to a lack of resources in the South African public healthcare system, several of the patients in this study were required to travel from outlying rural areas to access the arthroplasty service. In our opinion, the one-stage BTHA reduced the direct costs to the patient, the waiting period for surgery and the inconvenience associated with travel. Further cost data analysis needs to be performed.
Despite being pain-free and independent ambulators, 18% of patients requested a disability grant application postoperatively at their first follow-up visit. It is therefore assumed that the rest of the patients (82%) attempted to return to work or their previous level of employment as most patients were the primary breadwinners in their families. The current employment status data was not available in the patient records. Patients subjectively reported improved quality of life (pain-free and independent ambulators post-surgery); however, no instrument was used to measure HRQOL in the electronic records.
There are several limitations to this study. It is retrospective, hence reliant on information gained from the electronic patient records. The low sample size is due to the recent introduction (January 2016) of the one-stage BTHA protocol into the arthroplasty unit and there were strict selection criteria for patients (ASA stage I or II). We could not include a scoring system to assess clinical outcomes due to the inadequacy of data in the patient notes and there was a varied follow-up period due to the lack of resources to attend the hospital regularly, which may have altered the analysis.
Conclusion
We have performed an analysis on retrospective records of 33 patients who underwent a one-stage bilateral total hip replacement (BTHA), and present the short-term outcomes at a median follow-up of 22 months (IQR 11-45 months). Our results suggest that surgical treatment with a one-stage BTHA is a good alternative to a two-stage BTHA when performed in a high-volume arthroplasty centre and carefully selected patients. The 30-day mortality rate was 0%, and the complication rate was low.
The level of evidence of this retrospective study is low with a low sample size and no comparison group; therefore, randomised controlled studies on this subject are recommended.
Ethics statement
The authors declare that this submission is in accordance with the principles laid down by the Responsible Research Publication Position Statements as developed at the 2nd World Conference on Research Integrity in Singapore, 2010. Prior to the commencement of the study ethical approval was obtained from the following ethical review board: UKZN BREC, reference number BREC/00003168/2021. All procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Declaration
The authors declare authorship of this article and that they have followed sound scientific research practice. This research is original and does not transgress plagiarism policies.
Author contributions
SMM: study conceptualisation, data capture, data analysis, first draft preparation, manuscript revision
JR: data analysis, final draft preparation
IEG: language and grammar correction, data analysis
ORCID
Mia SM https://orcid.org/0000-0002-3834-2730
Rajpaul J https://orcid.org/0000-0001-8950-4878
References
1. Youngman TR, Riepen DW, Rinehart DB, et al. Complications of primary total hip arthroplasty in humanimmunodeficiency virus-positive patients with femoral head osteonecrosis. Hip Int. 2021:11207000211005750. https://doi.org/10.1177/11207000211005750 [ Links ]
2. Vandormael A, Cuadros D, Kim HY, et al. The state of the HIV epidemic in rural KwaZulu-Natal, South Africa: a novel application of disease metrics to assess trajectories and highlight areas for intervention. Int J Epidemiol. 2020;49(2):666-75. https://doi.org/10.1093/ije/dyz269 [ Links ]
3. Steinberg ME, Hayken GD, Steinberg DR. A quantitative system for staging avascular necrosis. J Bone Joint Surg Br. 1995;77(1):34-41. [ Links ]
4. Kim SC, Lim YW, Jo WL, et al. Surgical accuracy, function, and quality of life of simultaneous versus staged bilateral total hip arthroplasty in patients with osteonecrosis of the femoral head. BMC Musculoskelet Disord. 2017;18(1):266. https://doi.org/10.1186/s12891-017-1605-2 [ Links ]
5. Saini R, Powell J, Sharma R, et al. One-stage versus 2-stage bilateral total joint arthroplasty: a matched cohort study. Can J Surg. 2020;63(2):E167-73. https://doi.org/10.1503/cjs.001019 [ Links ]
6. Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60(2):217-20. [ Links ]
7. Brooker AF, Bowerman JW, Robinson RA, Riley LH, Jr. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am. 1973;55(8):1629-32. [ Links ]
8. Taheriazam A, Saeidinia A. Short-term outcomes of one-stage bilateral total hip arthroplasty in young patients (< 30 years old). Orthop Rev (Pavia). 2018;10(2):7542. https://doi.org/10.4081/or.2018.7542 [ Links ]
9. Tan Z, Cao G, Wang G, et al. Total hospital cost, length of stay, and complications between simultaneous and staged bilateral total hip arthroplasty: A nationwide retrospective cohort study in China. Medicine (Baltimore). 2019;98(11):e14687. https://doi.org/10.1097/MD.0000000000014687 [ Links ]
10. Partridge TCJ, Charity JAF, Sandiford NA, et al. Simultaneous or staged bilateral total hip arthroplasty? An analysis of complications in 14,460 patients using national data. J Arthroplasty. 2020;35(1):166-71. https://doi.org/10.1016/j.arth.2019.08.022 [ Links ]
11. Calabro L, Yong M, Whitehouse SL, et al. Mortality and implant survival with simultaneous and staged bilateral total hip arthroplasty: experience from the Australian Orthopedic Association National Joint Replacement Registry. J Arthroplasty. 2020;35(9):2518-24. https://doi.org/10.1016/j.arth.2020.04.027 [ Links ]
12. Rolfson O, Digas G, Herbert P, et al. One-stage bilateral total hip replacement is cost-saving. Orthop Muscul Syst. 2014;3:4. https://doi.org/10.4172/2161-0533.1000175 [ Links ]
13. Houdek MT, Wyles CC, Watts CD, et al. Single-anesthetic versus staged bilateral total hip arthroplasty: a matched cohort study. J Bone Joint Surg Am. 2017;99(1):48-54. https://doi.org/10.2106/JBJS.15.01223 [ Links ]
14. Flick TR, Ofa SA, Patel AH, et al. Complication rates of bilateral total hip versus unilateral total hip arthroplasty are similar. J Orthop. 2020;22:571-78. https://doi.org/10.1016/j.jor.2020.11.010 [ Links ]
15. Guo SJ, Shao HY, Huang Y, et al. Retrospective cohort study comparing complications, readmission, transfusion, and length of stay of patients undergoing simultaneous and staged bilateral total hip arthroplasty. Orthop Surg. 2020;12(1):233-40. https://doi.org/10.1111/os.12617 [ Links ]
16. Ngwazi M, Ryan P, Goga I, Marais LC. The association between HIV infection and periprosthetic joint infection following total hip replacement in young adults. SA Orthop J. 2021;20(2):76-80. https://doi.org/10.17159/2309-8309/2021/v20n2a2 [ Links ]
17. Kim YH, Kwon OR, Kim JS. Is one-stage bilateral sequential total hip replacement as safe as unilateral total hip replacement? J Bone Joint Surg Br. 2009;91(3):316-20. https://doi.org/10.1302/0301-620x.91b3.21817 [ Links ]
18. Micicoi G, De Dompsure RB, Micicoi L, et al. One-stage bilateral total hip arthroplasty versus unilateral total hip arthroplasty: A retrospective case-matched study. Orthop Traumatol Surg Res. 2020;106(3):577-81. https://doi.org/10.1016/jotsr.2020.02.003 [ Links ]
19. Hou JF, Hu C, Zhang Y, et al. Cost analysis of staged versus simultaneous bilateral total knee and hip arthroplasty using a propensity score matching. BMJ Open. 2021;11(3):e041147. https://doi.org/10.1136/bmjopen-2020-041147 [ Links ]
20. Phillips JLH, Rondon AJ, Gorica Z, et al. No difference in total episode-of-care cost between staged and simultaneous bilateral total joint arthroplasty. J Arthroplasty. 2018;33(12):3607-11. https://doi.org/10.1016/j.arth.2018.08.035 [ Links ]
Received: October 2021
Accepted: March 2022
Published: August 2022
* Corresponding author: sayedmmia@gmail.com
Editor: Dr Chris Snyckers, Eugene Marais Hospital, Pretoria, South Africa
Funding: No funding was received for the purposes of performing this study.
Conflict of interest: The authors declare they have no conflicts of interest that are directly or indirectly related to the research.














