Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.21 n.3 Centurion 2022
http://dx.doi.org/10.17159/2309-8309/2022/v21n3a3
SPINE
Halo-external fixator frame-assisted correction to treat severe kyphotic deformity in children younger than 4 years old
Mehmet CetinkayaI; Vuyo GezenganaI; Theresa N MannI, II; Jacques du ToitI; Johan H DavisI, II, *
IDivision of Orthopaedic Surgery, Department of Surgical Sciences, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
IIInstitute of Orthopaedics and Rheumatology, Mediclinic Winelands Orthopaedic Hospital, Stellenbosch, South Africa
ABSTRACT
BACKGROUND: Severe kyphotic deformity in young children may have devastating outcomes when neglected. Halo-pelvic traction has been shown to be very effective as part of the treatment for severe kyphosis, but little is known about application of this technique in very young individuals. The aim of this case series was to provide novel insights into the surgical technique associated with halo-external fixator frame (HEFF) treatment for severe spinal deformity in patients younger than 4 years old, along with the associated radiologic outcomes and complications
METHODS: Clinical and demographic characteristics including the duration in the HEFF, HEFF-associated change in kyphosis angle (KA) and final KA following definitive surgery were extracted from medical records
RESULTS: Five female patients with a mean age of 36 months (range 30-44) were included. Three patients had thoracic spinal tuberculosis (mean KA 82°), one had lumbar spinal tuberculosis (KA 42°) and one had iatrogenic post-laminectomy cervical kyphosis (type 1 neurofibromatosis)(KA 112°). The HEFF was applied for a mean of six weeks and resulted in a mean thoracic deformity correction of 29° (38%), a lumbar correction of 23° (55%) and cervical correction of 47° (42%). Definitive surgery resulted in a further mean overall deformity correction of 28, and patients had a satisfactory KA angle (23° lordosis to 31° kyphosis) at the last follow-up. HEFF-associated complications included pin-site infection, pneumonia and frame dislodgement
CONCLUSION: HEFF appears to be an effective method for correcting severe kyphotic spinal deformity in very young patients where other options are limited. It allows for independent mobilisation and can provide for spinal stabilisation while awaiting bony healing after definitive surgery. However, healthcare providers should be aware of the potential dangers of HEFF hardware, such as difficulty in establishing an airway due to the fixed position of the neck
Level of evidence: Level 4
Keywords: external fixators, kyphosis, spine, child, tuberculosis
Introduction
Severe kyphotic deformities in very young patients may have devastating outcomes when neglected, including decreased thoracic volume and vital capacity, thoracic insufficiency syndrome and costo-pelvic impingement.1,2 The anteriorly folded trunk is usually accompanied by a posterior gibbus deformity, and longitudinal growth in the upper body is restricted. With extreme and progressive deformity, myelopathic changes of the spinal cord, and even paralysis, may occur.2,3
The treatment of choice for severe kyphotic deformity is surgical correction. However, these surgeries can be complex and high risk, especially in children. In the very young, the vertebrae are still largely cartilaginous, and even though instrumentation with spinal implants is possible, anchor strength is limited.4,5 Furthermore, techniques that require long segment instrumentation and fusion are not suitable for young children as this age group still has high longitudinal growing potential. Single-staged procedures for severe deformity may also have limited correction capacity in some cases and are associated with significantly increased perioperative complication rates due to the extensive surgical approach and risk to the spinal cord.3,6
Given the problems associated with corrective surgery alone to treat severe kyphotic deformity, various traction techniques have been developed to promote an improvement in deformity prior to definitive surgical correction.7-11 A traction-induced decrease in deformity has been shown to reduce preoperative patient risk scores along with the complexity and duration of the subsequent surgery.8,12 Furthermore, the gradual correction allows the spinal cord and its blood supply to adjust to the increased length and shape of the spine, reducing the risk of neurological insult as in acute correction.13 Severe deformity may be complicated by respiratory dysfunction, and traction has also shown substantial benefit for improving preoperative respiratory function in these cases.14,15 Traction techniques described in the literature include halo-pelvic, halo-gravity, and halo traction, accompanied by anterior release procedures as indicated.7-12,14-17
Halo-pelvic traction was first developed by O'Brien et al. in 1958 and has been shown to be very effective as part of the treatment for severe kyphosis.7,8,14,16-18 For example, previous studies have reported significantly reduced blood loss and surgery time when comparing patients who received preoperative halo-pelvic traction to those who received surgical correction only.8,17 In one study, preoperative halo-pelvic traction also significantly improved deformity correction and patient height compared to surgery alone, whereas another study found reduced complications with preoperative halo-pelvic traction but a similar postoperative deformity correction.8,17 In recent decades, halo-gravity traction has gained prominence for the treatment of kyphotic deformity, with halo-pelvic traction less commonly reported.9,10,12,19 However, the latter technique remains an effective and affordable option and may even have advantages when it comes to very young children.8,16
While halo-gravity traction has the advantage of leaving the legs and pelvis unrestrained, it does nevertheless limit independent mobility by requiring a wheelchair or suspensive walking frame, effectively tethering the patient to their gravity suspension device. Conversely, halo-pelvic traction allows for independent, bipedal mobility - an important consideration during the rapid growth and development of early life. This technique may also be more suited to the small body size and weight of very young children and, in addition, allows caretakers to carry and lift the patients for hygiene and other purposes without any alteration to the traction force or moment.
To our knowledge, use of a halo-external fixator frame (HEFF), with adjustability in three dimensions, for the treatment of severe kyphotic deformities has not previously been described in young children in whom the spinal column is not fully developed. Furthermore, to our knowledge, the use of six expandable struts with universal couplings joining the halo-ring to the pelvic ring construct, allowing for unique and controlled gradual correction of complex spinal deformities, has also not previously been reported. Thus, the aim of this case series was to provide a novel description of the surgical technique, radiological outcomes and complications associated with HEFF use in children younger than 4 years old.
Materials and methods
This case series followed the design of a retrospective cohort study and involved patients with severe spinal kyphotic deformity who underwent HEFF-assisted correction before definitive corrective surgery. The inclusion criteria were early-onset (< 4 years old) deformity and single kyphotic deformity with acute angulation that was corrected with HEFF as a last resort option. All procedures were performed by the same fellowship-trained senior orthopaedic spinal surgeon and took place at the same tertiary hospital between 2011 and 2017. The follow-up period presented spanned from the initial clinical examination to post-definitive surgical correction.
Data extracted from each patient's medical records included demographic details, medical history and body weight as well as the length of time in the HEFF, and any associated complications. Neurological status, kyphosis angle (KA) on radiographs before and after HEFF application and surgical procedure were also recorded.
Halo-external fixator-frame application
The HEFF application was performed under general anaesthesia. After preoperative evaluation for any potential anaesthesia-induction contraindication, pin entry sites, AP and lateral scoliosis radiographs, and limited fine slice computerised tomography (CT) scans of the deformities were evaluated for preoperative planning. The patient was first positioned in the supine position on the operating table. The HEFF was mocked up prior to surgery to aid with selection of appropriate ring sizes. Standard halo-application technique for children was used, with eight skull pins inserted. The anterior pin location was 1.5 cm above the lateral thirds of the eyebrows (Figure 1a). Posterior pin entry points were located right across to anterior pins and just 1 or 2 cm distal to the prominent equator of the head, with additional pins interspersed to evenly spread holding forces (Figure 1b). The pins were tightened in a cross-over fashion to 2 lbs/square inch (and subsequently re-tightened daily for three days). The pelvic ring was affixed with hydroxyapatite-coated Schanz pins placed bilaterally under fluoroscopy imaging guidance. Two pins were placed in the supra-acetabular region directly over the palpable greater trochanter of the femur in a coronal plane. Two pins were placed from anterior into the superior anterior iliac spines following the inter-table plane posteromedial, and a further two pins placed in the posterior iliac wings with an insertion point of posterior inferior iliac spine from posterior to anterior (Figure 1b and Figure 2). The pin tracts were drilled at low speed with a new sharp drill bit in order to avoid thermal necrosis and poor pin purchase. HA-coated pins were manually advanced until the threaded part was embedded in the bone with the smooth shank protruding from the soft tissue. The Schanz pins were fixed to an Ilizarov-type ring around the pelvis with at least 2 cm of distance between frame and skin (Figure 1b). The external fixator frame ring and the halo rings were then connected with two anterior and two posterior expandable external fixation rods, or by six adjustable struts with universal couplings to the rings to allow angular correction, thus allowing gradual distraction or deformity correction by alternating lengthening of the struts in a pre-planned fashion (Figure 3). Frame positioning for thoracic, lumbar and cervical spine deformities is shown in Figure 4. The pin sites were cleaned on a daily basis with sterile swabs and 2% chlorhexidine gluconate solution. No rod lengthening was done during the first postoperative week to allow for bone and hydroxyapatite-coated implant interface integration.

After supposed HA-bone integration, sequential adjustments were made to the struts on a daily basis according to a pre-determined plan to gradually correct the deformity specific to the individual case through distraction and/or segmental extension. Weekly control radiographs were taken to monitor correction in deformity and careful daily clinical examinations (specifically neurological function) followed the daily adjustments.
Results
Patient characteristics and presentation
There were five female patients who met the study criteria, with patient characteristics and diagnosis shown in Table I. The mean age was 36 months (range 30-44), and the mean body weight was 13 kg (range 9-14).
Patients 1-3 presented with deformity of the thoracic region. Each had a severe dorsal gibbus, and the mean initial KA was 82°. The spinous processes were typically splayed from distal adjacent ones. All patients appeared malnourished upon clinical examination. Furthermore, each had a positive TB contact history and palpable cervical lymphadenopathy. A single patient (patient 2) was neurologically intact whereas patient 1 and patient 3 had neurological deficit with a Frankel grade of B and D and Ashworth spasticity score of 2 and 3, respectively. The latter two patients were described as having insidious onset of progressive lower limb weakness accompanied by faecal incontinence developed over the past six weeks. Patient 2 had a previous T8-11 posterior onlay fusion (POF) when she was a 20-month-old.
Patient 4 presented with a lumbar kyphotic deformity. She had a cachectic appearance and was suffering from severe abdominal distension. She was initially investigated extensively for abdominal TB. However, MRI demonstrated large psoas abscesses causing abdominal distension. She had palpable cervical lymphadenopathy and a lumbar region gibbus deformity corresponding to L2-4 levels and causing a loss in lumbar lordosis and increased pelvic retroversion. X-rays revealed a 42° lumbar kyphotic deformity. There was no clinically evident neurologic deficit (Frankel E).
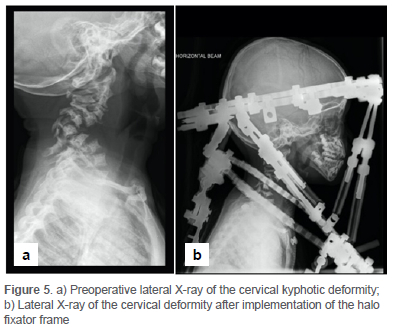
Patient 5 had involvement of the cervical spine and presented with a KA of 112° at C6-7 level and left arm weakness. She was able to walk with assistance but had a myelopathic gait disturbance and Frankel grade of D. Background medical history revealed cervical laminectomy for resection of epidural neurofibroma causing spinal cord compression and myelopathy when she was a 12-month-old. This resulted in a severe iatrogenic post-laminectomy, cervical kyphotic deformity. Unlike the other patients, this patient had a halo attached to a ring mounted on the shoulders of a body jacket, through six adjustable struts with universal couplings to allow angular correction of the cervical kyphosis (Figure 5).
HEFF-assisted deformity correction
Time spent in the HEFF along with change in deformity and neurological status is shown in Table II. In patients 1-3, with thoracic involvement, the mean KA decreased from 82° to 53° (38%) after HEFF application, with a mean traction duration of 6.3 weeks. Furthermore, patients 1 and 3, who had neurological deficit at baseline, showed one Frankel grade of neurological improvement during HEFF correction. The definitive surgeries performed were T4-10 strut graft followed by T3-11 posterior instrumented fusion (PIF), T6-11 anterior instrumentation and fusion, and T6-11 PIF, respectively. The KA was further improved to a mean of 29° after the definitive surgery, with no neurological fallout.
Patient 4 spent five weeks in the HEFF, during which time her kyphotic deformity was decreased from 42° to 19° (55%). She then underwent L2-4 anterior debridement and strut graft implementation followed by POF and remained in the HEFF for a further six weeks. Her curve decreased to 23° lordosis after the surgery and, at the last follow-up, there was no neurological deficit.
Patient 5 spent four weeks in the HEFF, after which the cervical deformity was reduced from 112° to 57° (42%). She subsequently underwent an anterior three-level corpectomy and bone graft strut and was immobilised further in the HEFF while admitted to the paediatric ICU. The patient regrettably demised shortly after this definitive corrective surgery as described under 'Complications' below.
Complications
During the time in HEFF traction, patient 1 had pin-site infection, and pin loosening three days before the intended removal of the frame. A hospital-acquired pneumonia developed and was effectively treated with antibiotics. Patient 4 developed surgical site infection, which resolved with vacuum-assisted closure dressings and oral antibiotics, as well as a nosocomial sepsis with unknown source that resolved on intravenous antibiotics. Patients 2 and 3 presented with dislodgement of the HEFF after a weekend pass-out in the care of their parents. In contrast, patient 5 did not experience complications during the HEFF traction. However, this patient developed respiratory arrest approximately 12 hours after a definitive surgical procedure, while still immobilised in the HEFF. After excluding obstructive airway compromise and all other surgery-related complications through post-mortem investigation, the death was attributed to a likely hypoventilation with progressive and gradual hypoxia secondary to opiate analgesia. The physician attending in ICU was unable to intubate the patient for ventilation assistance due to the rigid halo frame fixating the head and not allowing for cervical extension. This incident highlighted the risk and difficulty of managing the airway in such a patient. The authors subsequently keep a bolt cutter and laryngeal mask airway in close proximity to these patients in the early postoperative period.
Discussion
The current series constitutes one of the first descriptions of HEFF-assisted deformity correction in children younger than 4 years of age. The series showed that 4-8 weeks in the frame resulted in a mean kyphotic deformity correction of 29° (38%) for the three patients with thoracic involvement and corrections of 23° (55%) and 47° (42%) for patients with lumbar and cervical involvement, respectively. Definitive surgery resulted in a further mean overall deformity correction of 28° and patients had a satisfactory KA angle (23° lordosis to 31° kyphosis) at the last follow-up.
The HEFF-associated deformity correction observed in the current series is broadly in keeping with previous reports of halo-gravity-associated correction in older children. For example, Pourtaheri et al. reported a 33° (35%) mean reduction in thoracic kyphosis following a mean of 4.6 weeks halo-gravity traction among eight children 5-12 years of age.19 Similarly, Verhofste et al. reported a mean deformity correction of 38% in cervical kyphosis following 5.3 weeks of halo-gravity traction among 12 children with mean age of 11 years.20 Iyer et al. summarised previous halo-gravity studies as showing 30-35% deformity correction.12 Furthermore, in their own large study of 96 cases, the authors reported a mean deformity correction of 31% following halo-gravity traction among patients with a mean age of 17 years.12 In this instance, the mean period of traction period was 14 weeks, somewhat longer than that of Pourtaheri et al., Verhofste et al. and the current series.
Although patients in the current series developed complications such as infection or frame dislodgement, these could be resolved relatively easily and were generally similar to complications reported for other traction techniques. For example, complication rates of 53% and 34% have been reported for halo traction and halo-gravity traction, respectively, with the majority of complications consisting of pin-site infection.12,21 Forms of halo traction can also carry a risk of neurological injury, including injury to the cranial nerves, although no such complications were observed in the current series.21 Previously reported complications, such as limited range of motion in the cervical spine following prolonged immobilisation and avascular necrosis of the odontoid peg, were also not encountered in this series.22 This is possibly due to the shorter duration of traction and more flexible, yielding nature of the very young spine. In contrast to some of the aforementioned complications, the problem of airway access while fitted with a HEFF is clearly unique to this form of traction. While this constitutes a significant risk, such risk can be mitigated through having a bolt cutter and laryngeal mask readily available as a precaution.
Severe kyphosis is a relatively rare presentation and prospective studies to directly compare the effectiveness, required duration and complication rates of different traction techniques would be very challenging to execute. However, there is one notable retrospective study available.15 Chen et al. compared outcomes following preoperative halo-gravity traction or halo-pelvic traction among 81 patients with severe, rigid kyphoscoliosis (Cobb angle > 100°) and found largely in favour of the halo-pelvic technique.15 When compared to halo-gravity traction, halo-pelvic traction was associated with significantly shorter traction time, significantly better deformity correction, significantly better improvement in pulmonary function and fewer osteotomies.15 The authors noted that although halo-gravity traction is well tolerated, it has relatively poor strength and efficiency and may be subject to a 'plateau effect' within a relatively short period. Thus, it was felt to be unsuitable for rigid deformities. In contrast, halo-pelvic traction provided powerful distraction forces but was associated with prolonged hospitalisation, cervical stiffness, early cervical degeneration and pin-site infections.15
With few other comparative studies available, clinical judgement may play a significant role in the choice of traction technique for a particular presentation. The major advantage of halo-gravity traction is that it leaves the lower body unrestricted, significantly reducing patient discomfort. Nevertheless, this technique may provide relatively lower distraction strength and is thought to be unsuitable for rigid deformities.15 Patients managed with halo-gravity traction may also require more assistive care, including weight adjustment when changing to a supine position. The main advantage of the HEFF is that it allows for independent, bipedal mobilisation rather than reliance on a wheelchair or walking frame. Furthermore, independent mobilisation may somewhat reduce the level of assistive care required when compared to halo-gravity traction. From a technical perspective, the HEFF allows for gradual, controlled adjustment of traction in tiny increments every day and the nature of the apparatus allows for angular correction as well as length distraction. Furthermore, it can provide for spinal stabilisation while awaiting bony healing after definitive surgery. A major disadvantage of the HEFF is that it is clearly very burdensome for patients to wear, although the modified, half-ring halo-pelvic apparatus described by Wang and colleagues may partially relieve patient discomfort.14,16 This technique also typically involves prolonged hospitalisation and constant vigilance for pinsite infection.
The main limitation of the current study was the small sample size. A larger sample size may have provided a better representation of average HEFF-assisted deformity correction and common complications in this population, increasing the generalisability of the findings. Nevertheless, a large sample would have been difficult to achieve given that severe kyphosis in patients younger than 4 years is a rare presentation. For example, the current small sample was accumulated over seven years in a tertiary referral hospital.
Conclusion
Preliminary evidence suggests that HEFF is a powerful and effective technique for correcting severe kyphotic spinal deformity in very young patients. A major advantage of this method is that it promotes independent mobilisation of patients. However, healthcare providers should be aware of the potential dangers of HEFF hardware, such as difficulty with intubation due to the fixed position of the neck. For this reason, it is advisable to have bolt cutters within easy access during HEFF implementation as a safety precaution in addition to a laryngeal mask airway at the bedside.
Ethics statement
The authors declare that this submission is in accordance with the principles laid down by the Responsible Research Publication Position Statements as developed at the 2nd World Conference on Research Integrity in Singapore, 2010. Prior to submission of the case series, ethical approval was obtained from the following ethical review board: Health Research Ethics Committee of Stellenbosch University (reference number C20/06/017). All procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. We applied for a waiver of informed consent, which was approved by the Health Research Ethics Committee.
Declaration
The authors declare authorship of this article and that they have followed sound scientific research practice. This research is original and does not transgress plagiarism policies.
Author contributions
MC: data capture, first draft preparation, manuscript revision VG: data capture, first draft preparation, manuscript revision TM: manuscript revision JdT: data collection, manuscript revision
JHD: study conceptualisation, data collection, manuscript revision
ORCID
Cetinkaya M https://orcid.org/0000-0002-7131-4280
Gezengana V https://orcid.org/0000-0002-4846-0204
Mann T https://orcid.org/0000-0002-9750-5106
Du Toit J https://orcid.org/0000-0002-0958-5450
Davis JH https://orcid.org/0000-0002-1909-7629
References
1. Tuli SM. Severe kyphotic deformity in tuberculosis of the spine. Int Orthop. 1995;19(5):327-31. https://doi.org/10.1007/bf00181121 [ Links ]
2. Jain AK, Dhammi IK, Jain S, Mishra P. Kyphosis in spinal tuberculosis - Prevention and correction. Indian J Orthop. 2010;44(2):127-36. https://doi.org/10.4103/0019-5413.61893 [ Links ]
3. Jain AK, Kumar J. Tuberculosis of spine: neurological deficit. Eur Spine J. 2013;22 Suppl 4:624-33. https://doi.org/10.1007/s00586-012-2335-7 [ Links ]
4. Sangondimath G, Mallepally AR, Yelamarthy PKK, Chhabra HS. Severe Pott's kyphosis in a 19-month-old child: case report and review of literature. World Neurosurg. 2019;130:30-36. https://doi.org/10.1016/.wneu.2019.06.097 [ Links ]
5. Horn A, Watt J, Dunn R. Spinal fusion for paediatric lumbosacral spondylolisthesis. SA Orthop J. 2018;17(4):39-43. https://doi.org/10.17159/2309-8309/2018/v17n4a5 [ Links ]
6. Kose KC, Bozduman O, Yenigul AE, Igrek S. Spinal osteotomies: Indications, limits and pitfalls. EFORT Open Rev. 2017;2(3):73-82. https://doi.org/10.1302/2058-524L2.160069 [ Links ]
7. O'Brien JP, Yau AC, Smith TK, Hodgson AR. Halo pelvic traction. A preliminary report on a method of external skeletal fixation for correcting deformities and maintaining fixation of the spine. J Bone Joint Surg Br. 1971;53:217-29. [ Links ]
8. Muheremu A, Ma Y, Ma Y, et al. Halo-pelvic traction for severe kyphotic deformity secondary to spinal tuberculosis. Medicine (Baltimore). 2017;96(28):e7491. https://doi.org/10.1097/md.0000000000007491 [ Links ]
9. Koller H, Zenner J, Gajic V, et al. The impact of halo-gravity traction on curve rigidity and pulmonary function in the treatment of severe and rigid scoliosis and kyphoscoliosis: a clinical study and narrative review of the literature. Eur Spine J. 2012;21(3):514-29. https://doi.org/10.1007/s00586-011-2046-5 [ Links ]
10. Iyer S, Duah HO, Wulff I, et al. The use of halo gravity traction in the treatment of severe early onset spinal deformity. Spine (Phila Pa 1976). 2019;44(14):E841-45. https://doi.org/10.1097/brs.0000000000002997 [ Links ]
11. Bono CM. The halo fixator. J Am Acad Orthop Surg. 2007;15(12):728-37. https://doi.org/10.5435/00124635-200712000-00006 [ Links ]
12. Iyer S, Boachie-Adjei O, Duah HO, et al. Halo gravity traction can mitigate preoperative risk factors and early surgical complications in complex spine deformity. Spine (Phila Pa 1976). 2019;44(9):629-36. https://doi.org/10.1097/brs.0000000000002906 [ Links ]
13. Kim N-H, Kim H-J, Moon S-H, Lee H-M. 20-year-follow up of treatment using spine osteotomy and halo-pelvic traction for tuberculous kyphosis - a case report. Asian Spine J. 2009;3(1):27-31. https://doi.org/10.4184/asj.2009.31.27 [ Links ]
14. Qi L, Xu B, Li C, Wang Y. Clinical efficacy of short-term pre-operative halo-pelvic traction in the treatment of severe spinal deformities complicated with respiratory dysfunction. BMC Musculoskelet Disord. 2020;21(1):665. https://doi.org/10.1186/s12891-020-03700-9 [ Links ]
15. Chen J, Sui W-Y, Yang J-F, et al. The radiographic, pulmonary, and clinical outcomes of patients with severe rigid spinal deformities treated via halo-pelvic traction. BMC Musculoskelet Disord. 2021;22(1):106. https://doi.org/10.1186/s12891-021-03953-y [ Links ]
16. Wang Y, Li C, Liu L, Qi L. Halo-pelvic traction for extreme lumbar kyphosis: 3 rare cases with a completely folded lumbar spine. Acta Orthop. 2021;92(1):9-14. https://doi.org/10.1080/17453674.2020.1824170 [ Links ]
17. Ouyang B, Luo C, Ma X, et al. [Comparison of radiological changes after Halo-pelvic traction with posterior spinal osteotomy versus simple posterior spinal osteotomy for severe rigid spinal deformity]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi [Chinese Journal of Reparative and Reconstructive Surgery]. 2020;34:900-906. [ Links ]
18. Kalamchi A, Yau AC, O'Brien JP, Hodgson AR. Halo-pelvic distraction apparatus. An analysis of one hundred and fifty consecutive patients. J Bone Joint Surg Am. 1976;58(8):1119-25. [ Links ]
19. Pourtaheri S, Shah SA, Ditro CP, et al. Preoperative halo-gravity traction with and without thoracoscopic anterior release for skeletal dysplasia patients with severe kyphoscoliosis. J Child Orthop. 2016;10(2):135-42. https://doi.org/10.1007/s11832-016-0721-0 [ Links ]
20. Verhofste BP, Glotzbecker MP, Birch CM, et al. Halo-gravity traction for the treatment of pediatric cervical spine disorders. J Neurosurg Pediatr. 2020;25:384-93. [ Links ]
21. Limpaphayom N, Skaggs DL, McComb G, et al. Complications of halo use in children. Spine (Phila Pa 1976). 2009;34(8):779-84. https://doi.org/10.1097/brs.0b013e31819e2d90 [ Links ]
22. Dove J, Hsu LC, Yau AC. The cervical spine after halo-pelvic traction. An analysis of the complications of 83 patients. J Bone Joint Surg Br. 1980;62-B(2):158-61. https://doi.org/10.1302/0301-620x.62b2.7364826 [ Links ]
Received: June 2021
Accepted: August 2021
Published: August 2022
* Corresponding author: jdavis@ior.health
Editor: Prof. Robert N Dunn, University of Cape Town, Cape Town, South Africa
Funding: No funding was received for this study.
Conflict of interest: The authors declare they have no conflicts of interest that are directly or indirectly related to the research.














