Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SA Orthopaedic Journal
versión On-line ISSN 2309-8309
versión impresa ISSN 1681-150X
SA orthop. j. vol.21 no.2 Centurion 2022
http://dx.doi.org/10.17159/2309-8309/2022/v21n2a3
HAND
Splints and immobilisation approaches used for second to fifth metacarpal fractures: a systematic review
Monique M KellerI, *; Roline Y BarnesI; Corlia BrandtII; Lauren M HepworthIII
IDepartment of Physiotherapy, School of Health and Rehabilitation Sciences, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
IIDepartment of Physiotherapy, School of Therapeutic Sciences, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIIOccupational therapist, private practice, Durban, South Africa
ABSTRACT
BACKGROUND: The second to fifth metacarpal fractures are immobilised with splints, plaster of Paris (POP) or buddy strapping for a period of time. However, no recent evidence-based splinting and immobilisation programme exists for the management thereof, leaving a gap in the literature to inform clinical practice. This review aimed to review, appraise and collate the literature on splints and immobilisation approaches used for second to fifth metacarpal fractures after surgical and conservative management in adults aged 20 to 59 years.
METHODS: The review included experimental study designs, quasi-experimental studies, cohort studies and case-control studies from January 2008 to September 2018. Two reviewers independently screened, selected, appraised and extracted data from the included studies. Preferred reporting items for systematic reviews and meta-analysis (PRISMA) guided the reporting. Joanna Briggs Institute (jBl) critical appraisal tools were used to assess the risk of bias for each included study.
RESULTS: Database searches generated 1 005 articles with ten additional articles found on Google Scholar. Ten articles were included: two randomised controlled trials (RCTs), one quasi-RCT, four prospective studies, one retrospective record review, one retrospective study and one comparative study with descriptive reporting of the results.
CONCLUSION: High level 1b evidence suggests that no reduction, a soft wrap and buddy strapping for three weeks with early active finger and wrist mobilisation are effective for individuals who sustained boxer's fractures with < 70° angulation. To guide clinical practice, high-level research is needed to determine the immobilisation of second to fifth metacarpal fracture types.
Level of evidence: Level 2
Keywords: boxer's fracture/s, immobilisation, metacarpal fractures, splints, orthosis
Introduction
Metacarpal fractures account for 10% of bony injuries and are one of the most prevalent upper limb injuries among adults.1 Among all hand fractures identified in the United States (US), metacarpal fractures have an incidence rate of 13.6 per 100 000 persons per year and a prevalence of 33%.2 Fifth metacarpal neck fractures or boxer's fractures account for 10% of all hand fractures that have left individuals with functional deficits, including weakened grip strength and decreased metacarpal joint range of motion (ROM).3 The concern is the residual deficits that impact the young and working adult population as they seem to sustain metacarpal fractures more often.4 The potential functional implications of sustaining a second to fifth metacarpal fracture can impact the individual in all components of the International Classification of Functioning, Disability and Health (ICF) framework, namely body functions and structures, activity and participation.5
The problem is that no best-evidence splinting and immobilisation programme exists to inform clinical practice. This can lead to disability, decreased hand function and poor health-related quality of life (HRQoL). A period of immobilisation is widely deemed part of the management after sustaining second to fifth metacarpal fractures.6 Surgical intervention includes open reduction internal fixation with compression and plates, screws, or Kirshner wires (K-wires) to improve stability, followed by a period of immobilisation.7-9 Conservative management includes closed reduction if required, with external protection utilising a splint, U-shaped, non-circumferential plaster of Paris (POP), strapping the injured metacarpal finger to the adjacent uninjured metacarpal finger (buddy strapping) or mobilisation.
Splints and immobilisation approaches for second to fifth metacarpal fracture management vary in the literature. Fabrication of customised splints requires technical skill, in-depth knowledge of pathology and anatomy, bone-healing time frames, and surgery. Occupational therapists and physiotherapists trained in the management of hand injuries are qualified to choose, design, apply, individualise and adjust splints according to their specific needs, and administer rehabilitation programmes. Reviewing existing literature on splints and immobilisation approaches used for second to fifth metacarpal fractures would provide an appraisal of evidence on the various splints and immobilisation approaches currently used to provide guidance to clinicians in clinical practice.
Therefore, the research question guiding the scoping type systematic review was: What evidence is available for conservative and post-surgical splints and immobilisation approaches utilised (including, but not limited to, POP and/or splints) as part of initial management for adults older than 20 years and younger than 59 years of age, reporting on outcomes which included, but were not limited to, hand function, HRQoL, disability, digital ROM, grip strength and fine motor dexterity after sustaining single or multiple second to fifth metacarpal fractures?
The review's objective was to determine the immobilisation and splint approaches utilised for post-surgical and conservative management for 20- to 59-year-old adults who sustained a single or multiple second to fifth metacarpal fracture.
Methods
This research was registered with PROSPERO (number CRD 42019132620), and the review protocol adhered to PRISMA recommendations.10 Databases accessible to the University of the Free State and the electronic platforms searched were: Academic Search Ultimate, MEDLINE with Full Text, CINAHL with Full Text, CAB Abstracts, Health Source: Consumer Edition, Africa-Wide Information, Health Source: Nursing/Academic Edition, SPORTDiscus with Full Text and MasterFILE Premier with additional searches on Scopus and Web of Science. An information scientist, an expert librarian at the University of the Free State was consulted and assisted with searching databases and searching for databases. The reference lists of included full-text articles were screened for additional research/articles. An additional search for grey literature was performed on the internet with Google and Google Scholar with the keywords: boxer's fracture/s, immobilisation, metacarpal fractures, splints, orthotic devices, splinting with Boolean operators. An example of the search strategy keywords for one database is presented in Table I.

An adapted Cochrane document for randomised controlled trials (RCT) and non-RCTs (Cochrane website) was piloted on three studies to ensure accuracy and consistency. Two independent reviewers independently screened, selected, appraised and extracted data from three eligible studies. The pilot study was undertaken to assess the consistency of the review procedures. Joanna Briggs Institute (JBI) critical appraisal tools were used to assess risk of bias for the pilot studies.12 No changes were made after the pilot study, a high inter-rater agreement was found, and one of the pilot studies was included in the final data extraction.
Eligibility
Intervention studies in English for the period January 2008 to September 2018 were included. Eligible studies complied with the following inclusion criteria: adult participants between 20 and 59 years of age, reporting on conservative and post-surgical immobilisation and splints utilised (including, but not limited to, POP and/or splints, buddy strapping) for single or multiple second to fifth metacarpal fractures. Studies with participants younger than 20 years were not included due to skeletal immaturity.11 Nakashian et al. reported that very few individuals sustain metacarpal fractures after 59 years of age.2 Thus, studies with participants older than 59 years were omitted. Studies reporting on outcomes included, but were not limited to, hand function, HRQoL, disability relating to the loss of hand function, digital ROM, grip strength, return to work, and fine motor dexterity.
Exclusion criteria were studies investigating thumb metacarpal fractures, studies investigating second to fifth metacarpal fractures with an associated tendon injury, nerve injury or preexisting osteoarthritis or rheumatoid arthritis. Studies reporting on concurrent fractures of the phalangeal, carpal, distal radius and ulna bones were also excluded. Studies reporting on fractures with infections were also excluded.
Screening
After the database searches, all identified articles were imported into Endnote® (Clarivate Analytics, PA, USA), and duplicates removed. Two reviewers independently screened the identified articles against their titles and abstracts. The remaining articles were independently assessed for eligibility according to the inclusion criteria in a standardised and unbiased manner. Disagreement in selecting included articles was resolved between the reviewers. Inter-rater reliability of 0.80 Cronbach's alpha among the two reviewers during the second phase indicated a substantial agreement and consensus during the eligibility phase. Full-text articles were retrieved for all eligible articles. Data was extracted from the included articles using the piloted data extraction template.
Data extraction
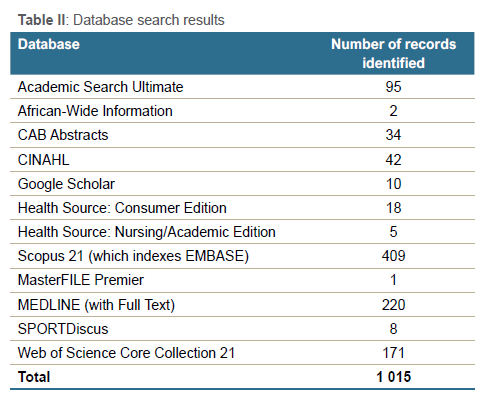
The database searches generated 1 005 research articles, with ten additional articles identified through a Google Scholar search, resulting in 1 015 articles (Table ll). From the total 1 015 research articles, 490 duplicates were removed, with 525 articles remaining for screening by the two reviewers. The reviewers excluded 515 articles due to languages other than English (69), paediatric articles (37), metacarpal fractures with associated tendon injuries (15), studies performed on animals (88), articles reporting on only surgical intervention for metacarpal fractures (295) and other sources with participants older than 59 years and first (thumb) metacarpal fractures (11) (Figure l).
Assessment of the methodological quality
The reviewers independently assigned a grade and assessed the risk of bias for each included study, with the JBI critical appraisal tools assessing the studies' relevance, results and trustworthiness.12 Depending on the study design, the aspects assessed were: use of true randomisation, concealment of allocation to treatment groups, clear description of the study setting, and included participant numbers, whether the exposure to the measurement was valid and reliable, identification of confounding variables, strategies to deal with confounding variables reported on, outcomes measured reliably and validly, appropriate statistical analysis, to name a few.
To ensure methodological rigour, the reviewers assessed all the included eligible articles according to the grading of recommendations assessment, development and evaluation (GRADE) method.13 A high and moderate certainty level of evidence was accepted, and a low and very low certainty level was documented.11
Ten articles were included in totality, showing a dearth of literature in the field. Two articles had high-quality ratings, one moderate quality, and seven low-quality ratings, as shown in the summary of the findings table available online (Supplemental table). High-quality rating indicated confidence in estimating effects, and future research is unlikely to affect or change the confidence. A moderate quality rating indicated that further research is likely to impact confidence and may even change the estimate. A low quality indicated that future research has a very high likelihood of impacting the confidence in effect estimation.13 A narrative analysis of all ten included articles is provided with a summary of the findings in the supplemental table (https://saoj.org.za/index.php/saoj/article/view/524/626).
Results
According to the objective, the presentation of the narrative results below is to appraise and collate the literature on splint and immobilisation approaches for conservative and post-surgical immobilisation and splint approaches used in 20- to 59-year-old patients who sustained a single and/or multiple second to fifth metacarpal fracture(s) according to the specified fracture levels.
Evidence on shaft metacarpal fractures
A prospective study conducted in Saudi Arabia investigated the conservative management of spiral and long oblique shaft fractures of second to fifth metacarpal bones.14 Participants presenting with minimally displaced, no significant angulation fractures with no rotation malalignment, were included in the study.14 A low GRADE quality of evidence rating was given. Management included immobilisation using a wrist POP (20° to 30° wrist extension with fingers free) for two weeks, which was followed by mobilisation guided by a home programme. Follow-up occurred at two weeks, six weeks, three months and six months postoperatively (n = 42). Extension lag was noted in all participants (50%) at two and six weeks, but no extension lag was reported at six months. Total active motion (TAM) and grip strength were significantly increased by six months with a resulting mean TAM of 260° and 90% grip strength compared to the contralateral hand.14
A prospective study conducted in the United Kingdom included 30 individuals who sustained single or multiple, middle or border, closed spiral metacarpal fractures.15 All participants had fractures with malrotation.15 A low GRADE quality of evidence rating was given. Management included both no splint and thus no immobilisation. Gradual early mobilisation was encouraged. The participants had to make a fist, up to 2 cm measured from finger to the palm, before they were discharged. Twenty-five participants attended the follow-up session. At seven days after injury, malrotation was measured through visual observation, and no formal X-ray measurements were taken. Malrotation was present in a third of the participants during the clinic follow-up session. The outcomes measured between six and 14 months after injury included: ROM, grip strength, palpation of the fracture site to assess bone union, obtaining verbal feedback from participants on a scale of poor, fair and good, verbally assessing functional limitations, verbally assessing cosmetic satisfaction of the hand on a scale of good, fair and poor, and shortening of the Angers. Fingers shortening ranged between 2 and 5 mm with a mean of 4 mm. The authors concluded that good hand function and no clinically significant sign of malrotation was present.15 The lack of formal X-ray measurements to ensure optimal bone healing and guide management is a concern. Not using standardised outcome measures for hand function compromised the generalisability and quality of the findings.
In Nova Scotia, a prospective research study was conducted on 61 patients with second to fifth non-scissoring spiral metacarpal fractures where they were managed conservatively.16 A low GRADE quality of evidence rating was given. Exclusion criteria included metacarpal fractures requiring surgical intervention and thumb fractures. Conservative management included immobilisation in a splint moulded to 20° of wrist extension, affected metacarpophalangeal joint (MCPJ) with one adjacent unaffected MCPJ in 30° flexion and the interphalangeal joints extended for one week. After one week, the splint was removed for showering, exercises, and at night for the patients deemed to be compliant and who no longer took pain medication or experienced pain. The splint was kept on during sleep periods and for more demanding activities during the day. During less busy daytime periods, the splint was removed, hands were moved when movements did not cause pain, but no other use of the hand was allowed. The splint was removed after three weeks. Grip strength and ROM as outcomes were measured at three, six and > 22 weeks after the injury. At five months, the final follow-up, the mean grip strength for the uninjured hand was 36.18 kg and the injured hand 36.58 kg.16
From these three studies, the following splint can be used with confidence for individuals who sustained second to fifth metacarpal shaft fractures:
• Thermoplastic splint with the wrist in 20-30° with the fingers free.
Evidence on neck and shaft of fifth metacarpal fractures
A Turkish retrospective record review comparative study was conducted on 140 participants with a mean age of 30.56 years. A low GRADE quality of evidence rating was given. The inclusion criteria included sustaining an isolated, extra-articular, neck or shaft fifth metacarpal fracture with more than 30° of angulation. The participants were allocated to two groups.17 The management of group A included reduction and immobilisation of the fourth and fifth fingers in a short arm POP with the following joint positions: wrist 30° extension, MCPJ 45° flexed, proximal interphalangeal joints (PIPJs) and distal interphalangeal joints (DIPJs) in 15° flexion for a mean of 29.15 days. Group B's management included reducing and immobilising the fourth and fifth fingers in a U-shaped gutter splint with the following joint positions: wrist 30° extension, MCPJ 45° flexed, PIPJs and DIPJs in 15° flexion for a mean of 29.15 days.17 After removing the POP and splints, an X-ray was taken, and bone healing clinically assessed with pain present or absent on the fracture line. A month later, assessments were performed including: ROM with a goniometer, clinical assessment of rotational deformity in the fifth finger and grip strength of the dominant and non-dominant hands with a Jamar hand dynamometer. Group A scored 90.38% grip strength compared to the unaffected side, and group B 90.58%. Two participants from group A and group B had a 10° extension lag. In group A, two participants had hypoesthesia along the ulnar nerve's dorsal cutaneous branch, which resolved in three weeks. One participant presented with a superficial wound between the third and fourth webspace due to POP pressure. No complications were experienced in group B. No significant statistical difference was found between groups for grip strength, range of motion (ROM) and dorsal angulation.
A clinical concern is that group A and group B, the wrist, PIPJ and DIPJ joints were included with possible reporting bias where complete ROM reporting was omitted. In the POP group, the long period of immobilisation caused pressure points and neuropraxia. The participants preferred the U-shaped ulnar gutter splints for their comfort, which clinicians should consider.
From these studies:
• No best-evidence splinting and immobilisation approach can be deducted as unaffected joints are included in the immobilisation.
Evidence on neck, shaft and base of fifth metacarpal fractures
A retrospective study was conducted in Glasgow, on 162 individuals who sustained fifth metacarpal (neck, shaft, base) fractures.18 A low GRADE quality of evidence rating was given. Exclusion criteria included dislocations, open injuries, intra-articular fractures, significant rotational deformities and polytrauma. The management had buddy strapping of the affected fifth finger to the neighbouring fourth finger for one week that allowed early active mobilisation, with information and no follow-up sessions. The information provided to the participants included an explanation of the fracture, guidance on how to commence early mobilisation and the natural history of the injury.18 Assessments were performed at a mean follow-up period of 21.6 months via a postal questionnaire and a follow-up telephone call. Outcomes assessed were: satisfaction with the injury outcome and the process on a four-point Likert scale, hand function with the QuickDASH, and disability with the EQ-5D. Response from 59% of the contacted individuals indicated satisfactory outcomes. The results revealed a median EQ-5D score of 0.87 (interquartile range [IQR] 0.74-1) out of a possible best score of 1 and a median QuickDASH score of 2.3 (IQR 0-6.8). Normative QuickDASH data used to make comparisons were a mean of 10.9, median 4.5, a standard deviation of 15.3, IQR 0-14.3 and a range of 0-88.6. Eighty-three participants (84.9%) were satisfied with the management process, and 79 participants (80.6%) were satisfied with the outcome of their injury. No significant difference was found when comparing EQ-5D (p = 0.307) and QuickDASH (p = 0.820) scores of uninjured individuals.18
A lack of reporting on outcomes, such as pain information measured with the EQ-VAS, which is part of the EQ-5D, TAM of the fifth finger and grip strength, affects the generalisability of this study's results to other populations. However, in a well-selected group of individuals who sustained fifth metacarpal neck, shaft and base fractures, the management pathway adds a valuable option for clinicians, especially in settings with limited resources. The benefits include decreased orthopaedic and hand therapy follow-up sessions, with positive financial and time implications for both government and patients.
From the studies, the immobilisation that can be used with moderate confidence, for individuals who sustained single or multiple neck, shaft or base of fifth metacarpal fractures, is:
• Buddy strapping the fifth to the fourth finger.
Evidence on neck of fifth (boxer's) metacarpal fractures
In Switzerland, a randomised multicentre trial on 68 participants who sustained fifth metacarpal neck fracture with < 70° of angulation and no rotational deformities was conducted.19 A high GRADE quality of evidence rating was given. The 68 participants were allocated to two intervention groups. Management for one group included no reduction, a soft wrap around the palm, and a buddy strap around the fourth and fifth fingers for three weeks. Immediate active wrist and finger mobilisation was encouraged with the soft wrap/buddy strap as conservative management. The other intervention included a reduction followed by a forearm wrist POP immobilisation extending to the PIPJ with MCPJ in extension for four weeks.19 The QuickDASH questionnaire results at four months displayed a mean difference of -10.9 between the groups indicating no significant difference. For other outcomes: pain, MCPJ ROM, grip strength, and aesthetic appearance, no significant differences were found. However, a significant difference was measured with days off work. The soft wrap and buddy strapping group participants returned to their occupation on average 11 days sooner than the reduction and POP immobilisation group (p = 0.03).19 The evidence provides clinical guidance that using a soft wrap and buddy strapping is as effective as reduction and POP immobilisation with no complications for neck of fifth metacarpal (boxer's) fractures with < 70° of angulation and no rotational deformities.
In Turkey, a comparative study included 24 male participants working in professional environments and who sustained uncomplicated closed fifth metacarpal neck fractures.20 A low GRADE quality of evidence rating was given. The participants were allocated to either a conservative or a surgical group based on preference.20 The conservative management group's intervention consisted of the Jahss closed reduction manoeuvre and immobilisation in a U-shaped ulnar gutter splint. The U-shaped splints positioned the fourth and fifth MCPJs and the PIPJs and DIPJs in a slightly flexed position. Follow-up appointments were conducted on the second and seventh days post-reduction, with the splint removed after four weeks. The surgical group underwent closed reduction with the Jahss manoeuvre and insertion of two K-wires. U-shaped ulnar gutter splints were applied directly after wound dressing for the surgical group and were removed after seven days.
The participants were allowed to perform self-care and other light everyday activities. Outcomes included: satisfaction and hand function on days 30 and 45 follow-up, with the QuickDASH questionnaire, TAM, angulation, shortening and rotation of the fractures at 30 days follow-up and return to work. All participants returned to work by 30 days postoperatively. No statistically significant difference between the conservative and surgical groups was seen in TAM, final shortening and final angulation. However, statistically significant differences were seen when the surgical group returned to work earlier (p < 0.001) and presented with improved hand function (p < 0.05). The recommendation from the authors was that antegrade intramedullary K-wire fixation for fifth metacarpal fractures should be performed.20 Randomisation, according to preference, is a limitation and a methodological flaw that affects the trustworthiness of the results. The prolonged period of immobilisation in the U-shaped ulnar gutter splints, which crosses the wrist for four weeks as conservative management compared to only seven days post-surgical immobilisation, may be the reason for a statistically significant difference in hand function and return to work. For clinical practice, it is advisable to have a shorter immobilisation period to avoid stiffness and facilitate earlier return to work. Also imperative is not to include unaffected joints in the splints to improve the hand's functionality.
In a Swiss study, 40 individuals sustained a closed neck of fifth metacarpal fracture with palmar displacement of 30° to 70°.21 A moderate GRADE quality of evidence rating was given. Pseudo-randomisation was used to allocate 20 participants to the surgical group and 20 participants to the conservative group. The surgical group was managed with a Jahss manoeuvre reduction, K-wire insertion followed by a five-day immobilisation in a palmar two-finger splint, followed by a metacarpal hand-based brace (thermoplastic splint covering the dorsal and palmar aspects of the metacarpals of the fourth and fifth Angers) for Ave weeks where functional mobilisation was encouraged. K-wires were removed at three months. The conservative group received no reduction, with immobilisation for five days in a palmar two-finger splint, followed by functional mobilisation in the metacarpal hand-based brace for five weeks. No hand therapy was prescribed for either group. Follow-up appointments were: two and six weeks, three, six, and 12 months. Outcomes measured included: fifth finger MCPJ ROM, palmar angulation, MCPJ shortening, grip strength, and patient satisfaction. The mean fifth MCPJ ROM for the operative group was 98° and 96° for the conservative group compared to the unaffected side. At one year, the surgical group's mean grip strength was 51 kg, and 46 kg for the conservative group. None of the ROM or grip strength was statistically significantly different between groups. The surgical group indicated higher satisfaction scores and satisfaction with hand appearance.21 The metacarpal hand-based thermoplastic splint used as immobilisation covered the metacarpal and the metacarpal head without covering the wrist or PIPJs. Strub et al. found similar results to Van Aaken et al., where conservative management for boxer's fractures with < 70° degrees of angulation had satisfactory patient satisfaction outcomes, MCPJ ROM and grip strength.19,21 A palmar two-finger splint, followed by a metacarpal hand-based brace, supports the fracture site while allowing hand function and ROM while the fracture is healing.
From the three studies, the following splints can be used with confidence for individuals who sustained neck of fifth metacarpal fractures:
• Soft wrap and buddy strapping the fifth to the fourth fingers for three weeks.
• Palmar two-finger splint for five days followed by applying a thermoplastic metacarpal hand-based splint including the fourth and fifth MCPJs for five weeks.
In conclusion, in carefully selected individuals who sustained fifth neck of metacarpal fractures, buddy strapping and metacarpal hand-based splint immobilisation provide comfort, improved hand function, less stiffness and earlier return to work.
Evidence on second to fifth (not yet covered in other objectives) metacarpal fractures
A German prospective cohort RCT was conducted on 60 participants who sustained non-thumb metacarpal fractures.9 A high GRADE quality of evidence rating was given. The aim was to measure the effectiveness of a traditional physiotherapy (PT) programme compared to a home exercise (HE) programme after surgical management with open reduction internal fixation procedures. The 60 individuals were divided into two groups. Standardised controlled block randomisation was used to randomise participants into either a PT or HE group. A dorsal splint, including wrist, placed the MCPJ at 70° flexion (the interphalangeal joints were not included in the splint to move without restriction), was issued to both group participants for two weeks, after which the intervention and control group programmes commenced. The follow-up assessments at two weeks postoperatively demonstrated a severe loss of digital ROM in both groups. The grip strength improved for the PT group from six weeks to 12 weeks from 68% to 91% (100% is 270°) and from 71% to 93% for the HE group. At three months, the ROM improved to 245° TAM for the PT group and 256° TAM for the HE group out of a normal digit range of motion of 270°.9 A limitation of the study is that the management was not specific to the type of fracture sustained, and uninvolved joints were included during immobilisation. A further limitation was that a non-surgical management option was not included. In resource-restricted countries, surgical intervention with open reduction and internal fixation is not always feasible; thus, the results cannot be generalised to these countries, although they will greatly benefit from an HE programme for individuals with second to fifth metacarpal fractures to save resources expended for follow-up sessions.
In another article, an evidence-based pathway was compiled using a systematic review of all research before 2008.22 Following the development, the evidence-based pathway was tested on a sample of 50 patients in London who received surgical or nonsurgical management for metacarpal fractures.22 Thumb metacarpal and phalangeal fractures were excluded. The therapy treatment sessions included: splint fabrication, treatment administered and a leaflet describing fracture management. The pathway will now be presented according to the area where the fracture occurred, namely base, shaft, neck and head.
The base of the metacarpal fracture treatment pathway of the index finger (IF), middle finger (MF), ring finger (RF), and little finger (LF) was as follows: extra- and intra-articular fractures treated conservatively or with K-wires were given a forearm wrist splint positioned with the wrist at 20° extension, for four weeks. At four weeks from the day of the injury, light function and wrist exercises were encouraged. The splint was discarded after six weeks. When the fracture was managed surgically with an ORIF, light function was commenced at two weeks, with the splint discarded at four weeks.22
The shaft of metacarpal fracture treatment pathway for the IF, MF, RF and LF: forearm-based splints incorporating and positioning the wrist at 20° extension with the affected and one adjacent finger MCPJs positioned in 70° of flexion with a dorsal hood piece of the splint which was to be worn for three weeks. All other joints were left free and were able to move in the splint. After three weeks, the dorsal hood was removed, but the forearm-based splint was continued and only taken off for exercise periods. Exercises at three weeks included wrist and MCPJ active movement. The splint was worn only at night for two more weeks and discarded at six weeks. At four weeks, light function commenced. This time frame was applied to conservative or K-wire management of MJPJ shaft fractures. The fracture was managed with an ORIF, light function was initiated at two weeks, and the splint was discarded at four weeks.22
Neck and head metacarpal fracture treatment pathway for the IF, MF, RF and LF: a splint (hand-based) that positioned the affected MCPJ and an adjacent Anger's MCPJ in flexion of 70° was worn for a period of two to four weeks. After this period, the splint was removed, and the Anger's buddy strapped for another two weeks. In conservative or K-wire management, light function was commenced at four weeks, splint intervention continued at night and for protection during activities, and discarded at six weeks. In the ORIF managed fractures, light function was commenced at two weeks, splint intervention continued at night and for protection during activities and discarded at four weeks. Strengthening was started at six weeks.22
The evidence-based pathway was tested on 23 individuals.23 A low GRADE quality of evidence rating was given. Telephonic interviews performed follow-up assessments at 10-24 weeks post injury with the following results: compliance with the splint intervention was 47%, no complications were present, no pain in 72% of patients, employed patients had all returned to work, 92% of patients had full hand function, satisfaction with service among patients was 8/10, and three therapy sessions on average were provided.23 The results' generalisability was compromised by the small sample size and low compliance with the splint intervention. The lack of standardised outcomes used for hand ROM, disability and grip strength, and telephonic interview assessments affect the trustworthiness of the results. However, the splints proposed in the evidence pathway remain highly valuable for clinical practice because of the careful consideration given to not immobilise unaffected joints. The authors made a recommendation to conduct further research to evaluate the evidence pathway.23
From these studies for individuals who sustained a variety of different types of single or multiple second to fifth metacarpal fractures:
• Thermoplastic customised splinting and immobilisation period with all the unaffected joints not included, with early active mobilisation of unaffected joints encouraged.
Discussion
The purpose of this scoping-type systematic review was to determine the immobilisation and splint approaches utilised for post-surgical and conservative management for 20- to 59-year-old adults who sustained a single or multiple second to fifth metacarpal fracture. A detailed description of the literature has been provided, indicating no single preferred splint and method of immobilisation for each type of second to fifth metacarpal fracture.
Shaft fractures of second to fourth metacarpals were managed with certain similarities, such as spiral fractures, receiving forearm-based wrist splints.15,16 Active mobilisation was suggested for spiral fractures, but intra- and extra-articular fractures were conservatively or surgically managed with forearm-based thermoplastic splints with a dorsal hood piece left for three weeks with the splint being removed from four weeks.14,23 Wrist POP for two weeks was also suggested for spiral and long oblique fractures.14 A clinical recommendation is to use thermoplastic forearm wrist splints, which place the wrist at 20° extension, MCPJ in 70° of flexion, not including the PIPJs and DIPJs. Various articles suggest that care should be taken not to immobilise the unaffected joints, such as the wrist, for long periods, which will delay return to work and affect hand function.15,16,20 The authors in the sourced articles recorded various immobilisation methods for the neck (boxer's) of the fifth metacarpal fractures. These included a short POP wrist splint, a U-shaped gutter splint including the wrist, a soft palmar wrap and buddy strapping for three weeks or a wrist POP up to PIPs for four weeks.16,19 Also included was a U-shaped ulnar gutter splint for four weeks for conservative management and a U-shaped ulnar gutter splint seven days from K-wire insertion.20 Another method was a K-wire palmar two-finger splint for five days followed by a metacarpal hand-based splint for five weeks and conservative no reduction and similar splints.21 The hand surgery group had higher satisfaction and hand appearance satisfaction (including head). Finally, a hand-based thermoplastic splint for two to four weeks followed by buddy strapping for a further two weeks was used.23 In their multicentre RCT, Van Aaken et al. preferred buddy strapping as management for boxer's fractures with less than 70° palmar displacement.19 Recent literature supports buddy strapping instead of POP immobilisation for uncomplicated neck of fifth metacarpal fractures, and for neck of fifth metacarpal fractures without rotation deformities and for volar angulation less than 70°, due to less time off work and no complications due to POP immobilisation.24,25 At eight weeks, participants who sustained neck of fifth metacar-pal fractures managed with an elastic bandage around their metacarpals and wrist with early protected movement, displayed stronger grip strengths than the immobilisation in a U-shaped splint participants. 26 Patients with closed, isolated neck of fifth metacarpal fractures without rotational deformity were managed either by functional metacarpal splints supporting only the metacarpals or an ulnar gutter splint immobilising the wrist. At the six-month follow-up, both groups displayed similar grip strengths, reduction and hand function outcomes. In conclusion, patient comfort and splint-wearing compliance seen in the functional metacarpal splint group should be considered in practice.27
For the metacarpal base, intra- and extra-articular fractures, a forearm wrist splint for four weeks after K-wires and six weeks after conservative management was utilised.23 However, taking into account the post-surgical immobilisation for all types of second to fifth metacarpal fractures, a dorsal wrist splint for two weeks was sufficient as four weeks may be too long.9 In terms of positioning and type of material used, it was found that thermoplastic splinting material was preferred over POP due to the lower prevalence of pressure sores and hypoesthesia.17
The heterogeneity of the studies prevented the authors from conducting an effectiveness systematic review, and hence a scoping-type systematic review resulted. OpenDOAR was not used in the grey literature search and is a limitation.
Conclusion
We report on the evidence on splinting and immobilisation approaches used for second to fifth metacarpal fractures. The information provided should be used to guide decision making in clinical practice to ensure optimal hand function, decreased stiffness and early return to work. As the review only yielded ten relevant articles, a gap in the literature regarding evidence-based splinting and immobilisation programmes is seen, except for the initial immobilisation of boxer's fractures, where adequate evidence was found. Level 1b evidence for no reduction, a soft wrap and buddy strapping for three weeks with early active wrist and finger for management of boxer's fractures was found to be effective. Further research is, however, required for the other types of second to fifth metacarpal fracture immobilisation.
It is recommended that future research focuses on the effects of splints and immobilisation approaches using adequately powered RCTs and controlling for confounding variables, e.g., fracture type. Standardised outcome measures for both conservative and post-surgical groups should be used.
Acknowledgements
Thanks to Ms Annamarie du Plooy, an information scientist at the University of the Free State, for assisting with searching the databases. Thanks to Prof. Joanne Potterton for her reading of the draft and her support.
Ethics statement
The authors declare that this submission is in accordance with the principles laid down by the Responsible Research Publication Position Statements as developed at the 2nd World Conference on Research Integrity in Singapore, 2010.
Prior to commencement of the study, ethical approval was obtained from the following ethical review board: The Health Sciences Research Ethics Committee of the University of the Free State, ethical clearance number UFS-HSD2019/0046/2602. All procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Declaration
The authors declare authorship of this article and that they have followed sound scientific research practice. This research is original and does not transgress plagiarism policies.
Author contributions
MMK: conceptualised, drafted the protocol, submitted for ethical clearance, wrote the first draft and refined the article
RYB: read, elaborated on and refined the article
CB: read, elaborated and refined the article
LMH: assisted as an independent reviewer, read, elaborated on and refined the article
ORCID
Keller MM https://orcld.org/0000-0002-1513-295X
Barnes RY © https://orcld.org/0000-0002-3743-0077
Brandt C https://orcld.org/0000-0002-8445-1348
Hepworth LM © https://orcld.org/0000-0002-5747-7382
References
1. Bucholz RW. The epidemiology of fractures. Philadelpla, PA.: Llpplncott Williams & Wllklns; 2009. [ Links ]
2. Nakashian MN, Pointer L, Owens BD, Wolf JM. Incidence of metacarpal fractures in the US population. Hand. 2012;7(4):426-30. https://doi.org/10.1007/s11552-012-9442-0. [ Links ]
3. De Jonge JJ, Kingma, J, Van der Lei B, et al. Fractures of the metacarpals. A retrospective analysis of incidence an aetiology a review of the English-language literature. Injury. 1994;25(6):365-68. https://doi.org/10.1016/0020-1383(94)90127-9. [ Links ]
4. Anakwe RE, Aitken SA, Cowie JG, et al. The epidemiology of fractures of the hand and the influence of social deprivation. J Hand Surg Eur Vol. 2007;36(1):62-65. https://doi.org/10.1177/1753193410381823. [ Links ]
5. Saleeby PW. An introduction to the International Classification of Functioning, Disability and Health (ICF). Int J Disabil Hum Dev. 2016;15(1):1-3. https://doi.org/10.1515/ijdhd-2015-0027. [ Links ]
6. Wong VW, Higgins JP. Evidence-based medicine: management of metacarpal fractures. Plast Reconst Surg. 2017;140(1):140e-51e. https://doi.org/10.1097/PRS.0000000000003470. [ Links ]
7. Ozer K, Gillani S, Williams A, et al. Comparison of intramedullary nailing versus plate-screw fixation of extra-articular metacarpal fractures. J Hand Surg. 2008;33(10):1724-31. https://doi.org/10.1016/j.jhsa.2008.07.011. [ Links ]
8. Wong TC, Ip FK, Yeung SH. Comparison between percutaneous transverse fixation and intramedullary K-wires in treating closed fractures of the metacarpal neck of the little finger. J Hand Surg. 2006;31(1):61-65. https://doi.org/10.10164.jhsb.2005.06.022. [ Links ]
9. Gülke J, Leopold B, Grõzinger D, et al. Postoperative treatment of metacarpal fractures- Classical physical therapy compared with a home exercise program. J Hand Ther. 2018;31(1):20-28. https://doi.org/10.1016/jjht.2017.02.005. [ Links ]
10. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analysis: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006-12. https://doi.org/10.1016/j.jclinepi.2009.06.005. [ Links ]
11. De Sanctis V, Di Maio S, Soliman A, et al. Hand X-ray in pediatric endocrinology: Skeletal age assessment and beyond. Indian J Endocrinol Metab. 2014;18(7):63. https://doi.org/10.4103/2230-8210.145076. [ Links ]
12. Tufanaru C, Aromataris E, Campbell J, Hopp LMZ. Institute TJB. Chapter 3: Systematic reviews of effectiveness. [Internet]. 2017. Available from: https://reviewersmanual.joannabriggs.org/. [ Links ]
13. Oxman AD. Grading quality of evidence and strength of recommendations. BMJ. 2004;328(7454):1490-94. https://doi.org/10.1136/bmj.328.7454.1490. [ Links ]
14. Al-Qattan MM. Outcome of conservative management of spiral/long oblique fractures of the metacarpal shaft of the fingers using a palmar wrist splint and immediate mobilisation of the fingers. J Hand Surg Eur Vol. 2008;33(6):723-27. https://doi.org/10.1177/1753193408093559. [ Links ]
15. Khan A, Giddins G. The outcome of conservative treatment of spiral metacarpal fractures and the role of the deep transverse metacarpal ligaments in stabilising these injuries. J Hand Surg Eur Vol. 2015;40(1):59-62. https://doi.org/10.1177/1753193414540408. [ Links ]
16. Macdonald BB, Higgins A, Kean S, et al. Long-term follow-up of unoperated, nonscissoring spiral metacarpal fractures. Plast Surg. 2014;22(4):254-58. https://doi.org/10.4172/plastic-surgery.1000888. [ Links ]
17. Gulabi D, Avci CC, Cecen GS, et al. A comparison of the functional and radiological results of Paris plaster cast and ulnar gutter splint in the conservative treatment of fractures of the fifth metacarpal. Eur J Orthop Surg Traumatol. 2014;24(7):1167-73. https://doi.org/10.1007/s00590-013-1290-2. [ Links ]
18. Gamble D, Jenkins PJ, Edge MJ, et al. Satisfaction and functional outcome with 'self-care' for the management of fifth metacarpal fractures. Hand. 2015;10(4):607-12. https://doi.org/10.1007/s11552-015-9749-8. [ Links ]
19. Van Aaken J, Fusetti C, Lucchina, S, et al. Fifth metacarpal neck fractures treated with soft wrap/buddy taping compared to reduction and casting: results of a prospective, multicenter, randomised trial. Arch Orthop Trauma Surg. 2016:136(1):135-42. https://doi.org/10.1007/s00402-015-2361-0. [ Links ]
20. Cepni SK, Aykut S, Bekmezci T, et al. A minimally invasive fixation technique for selected patients with fifth metacarpal neck fracture. Injury. 2016;47(6):1270-75. https://doi.org/10.1016/j.injury.2016.01.034. [ Links ]
21. Strub B, Schindele S, Sonderegger J, et al. Intramedullary splinting or conservative treatment for displaced fractures of the little finger metacarpal neck? A prospective study. J Hand Surg Eur Vol. 2010;35(9):725-29. https://doi.org/10.1177/1753193410377845. [ Links ]
22. Toemen A, Midgley R. Hand therapy management of metacarpal fractures: An evidence-based patient pathway. Hand Therapy. 2010:15(4):87-93. https://doi.org/10.1258/ht.2010.010018. [ Links ]
23. Midgley R, Toemen A. Evaluation of an evidence-based patient pathway for non-surgical and surgically managed metacarpal fractures. Hand Therapy. 2011;16(1):19-25. https://doi.org/10.1258/ht.2010.010026. [ Links ]
24. Pellatt R, Fomin I, Pienaar C, et al. Is buddy taping as effective as Plaster immobilization for adults with an uncomplicated neck of fifth metacarpal fracture? a randomized controlled trial. Ann Emerg Med. 2019;74(1):88-97. https://doi.org/10.1016/jannemergmed.2019.01.032. [ Links ]
25. Martínez-Catalán N, Pajares S, Llanos L, et al. A prospective randomized trial comparing the functional results of buddy taping versus closed reduction and cast immobilisation in patients with fifth metacarpal neck fractures. J Hand Surg Am. 2020;45(12):1134-40. https://doi.org/10.1016/j.jhsa.2020.05.013. [ Links ]
26. Retrouvey H, Jakubowski J, Al-Taha M, et al. Prospective multicenter randomised controlled trial comparing early protected movement and splinting for fifth metacarpal neck fracture. Plast Surg. 2022;30(1):6-15. https://doi.org/10.1177/22925503211011952. [ Links ]
27. Kaynak G, Botanlioglu H, Caliskan M, et al. Comparison of functional metacarpal splint and ulnar gutter splint in the treatment of fifth metacarpal neck fractures: a prospective comparative study. BMC Musculoskelet Disord. 2019;20(1)169:1-10. https://doi.org/10.1186/s12891-019-2556-6. [ Links ]
Received: June 2021
Accepted: January 2021
Published: May 2022
* Corresponding author: monique.keller@wits.ac.za
Editor: Dr Duncan McGuire, University of Cape Town, Cape Town, South Africa
Funding: The authors declare that no commercial funding was received. The reviewer payments were funded by the Early Career Academic Development grant from the University of the Witwatersrand.
Conflict of interest: The authors declare they have no conflicts of interest that are directly or indirectly related to the research.














