Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.21 n.1 Centurion 2022
http://dx.doi.org/10.17159/2309-8309/2022/v21n1a7
CURRENT CONCEPTS REVIEW
Transarticular gunshot injuries: a systematic review of 150 years of management
Nando Ferreira; Cameron Anley; Etienne Joubert
Division of Orthopaedic Surgery, Department of Surgical Sciences, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
ABSTRACT
BACKGROUND: This review aims to collate all published work on the management of transarticular gunshot injuries to better inform decision-making when managing these injuries
METHODS: A systematic review using the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) was undertaken. A literature search of major electronic databases was conducted to identify journal articles relating to the management of transarticular gunshot injuries published from database inception until 31 January 2021
RESULTS: Sixty-eight publications reporting on the management of 544 patients were included. Injuries to the lower limbs were reported in 438 cases (81%), while injuries to the upper limb accounted for 106 cases (19%). A total of 145 patients (27%) developed a deep infection. Following the routine use of antibiotics, 6% of patients (14/251) developed an infection. A significantly higher hip joint infection rate was seen in patients who sustained associated hollow viscus injury (11/30, 37%
CONCLUSION: The management of transarticular gunshot injuries is currently based on limited high-quality evidence. Modern antibiotic and surgical management practices have resulted in low overall septic complications; however, different joints have different injury and complication profiles. Future research should be aimed at identifying joint-specific evidence-based care pathways
Level of evidence: Level 4
Keywords: gunshot, ballistic, joint, transarticular, intra-articular
Introduction
The global surge in civilian gun-related violence has focused a need for evidence-based management protocols.1-3 At present, the management of transarticular gunshot injuries remains controversial, with limited high-quality research to guide evidence-based management. Controversies regarding the need for surgical debridement, the long-term local and systemic effects of retained bullets or bullet fragments, the choice and duration of antibiotic therapy, and the management of intra-articular fractures remain.4-9 This systematic review explores the literature reporting on the treatment of transarticular gunshot injuries and aims to interpret the data to provide physicians with evidence to guide the management of these cases.
Methods
A systematic review using the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) was undertaken.
The review was prospectively registered on the PROSPERO database (CRD42021233384).
Search strategy for the identification of relevant studies
A literature search of databases was conducted and included Medline, Sciencedirect, Articlefirst, SA ePublications Journal collection and Web of Science. The search terms included 'gunshot', 'ballistic', 'bullet', 'joint', 'intra-articular' and 'transarticular' with the Boolean terms 'AND' and 'OR'. Searches were conducted from database inception to 31 January 2021 and were limited to human participants and publications in English. A manual search of the reference list of included studies was also undertaken to identify other studies meeting the inclusion criteria.
Inclusion and exclusion criteria
The PICOTT framework was used to develop the inclusion and exclusion criteria (Table I).
Study selection
Identified records were downloaded into Mendeley Desktop (version 1.19.4) and deduplicated. Titles were screened by a single reviewer (NF). Abstracts and then full texts were independently screened by two researchers (NF, CA) against the eligibility criteria, and any discrepancies were resolved through discussion.
Quality assessment
Included articles were assigned a level of evidence according to Sackett's rules of evidence that rank studies according to the probability of bias.10
Data extraction and synthesis
Data extracted from the included studies were captured in Microsoft Excel for Mac (version 16.45). Information relating to the joint involved, injury characteristics, treatment instituted, and complications/outcomes were collected. Additionally, the following information was listed for all articles: research theme, year of publication and geographic origin. A qualitative synthesis of studies with sufficient homogeneity was performed, while a narrative descriptive synthesis was used for the remaining data.
Results
The search strategies identified 1 587 references after deduplication. Full-text review of 97 studies resulted in 68 publications being retained for final review (Figure 1).
Study characteristics
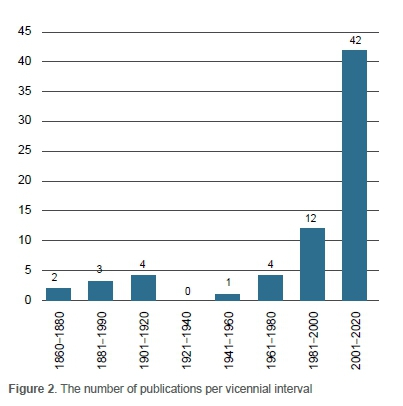
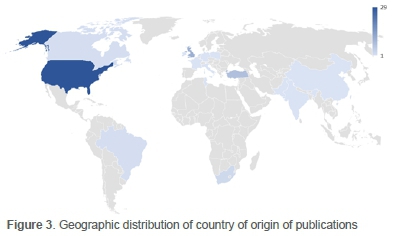
The included studies spanned 153 years and were published between 1867 and 2020, with a marked increase in publications over the last two decades (Figure 2).11-79Ten studies were published before 1944 (pre-antibiotic era), with the remaining 58 being published in the antibiotic era. The United States of America (n = 29) and the United Kingdom (n = 11) contributed the bulk of the publications (n = 40, 60%) (Figure 3).11-23,26,28-30,33,34,36,38-40,44,46,48,49,52,64,65,66 The majority of publications consisted of case studies (n = 45, 66%), while 22 (32%) were retrospective case series.11-60,62-79 Only one randomised control trial was included.61 According to Sackett's rules of evidence, the included studies consisted of one level 2, 22 level 3 and 45 level 4 studies.10
The research themes for the included articles broadly fell into three categories:
1. The management and outcome of acute injuries (n = 22)
2. The presentation and management of late complications (n = 23)
3. Bullet extraction techniques (n = 23)
Cumulative results of included cases
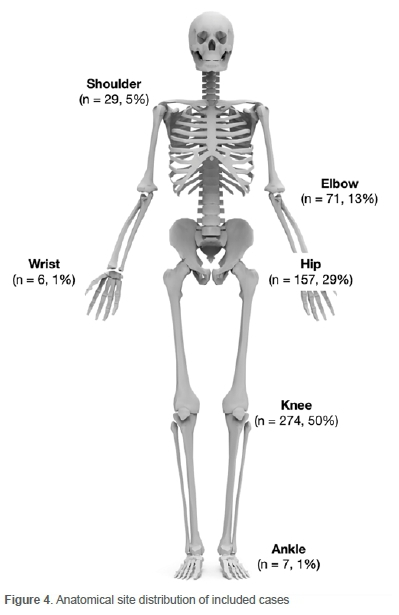
Sample sizes of the included papers ranged from 1 to 86 cases and included 544 transarticular gunshot injuries. Injuries to the lower limbs were reported in 438 cases (81%), while injuries to the upper limb accounted for 106 cases (19%) (Figure 4). Two hundred and seventy"nine patients (51%) sustained an intra"articular fracture, and 490 patients (90%) underwent surgical debridement as part of their management. A total of 145 patients (27%) developed a deep infection because of their injury. The mean follow"up for the entire cohort was four months, ranging from 0 to 142 months.
Retained intra-articular bullets or bullet fragments were reported in 198 patients (36%). Lead arthropathy due to retained bullet fragments was diagnosed in 24 patients (12%) and was seen after gunshots to 16 hips, three knees, two ankles, two wrists and one shoulder.21,22,28,30,50,54,58-60,63,65,69,71,73,76,77,79 These patients presented at a median of 42 months (range 3-624) following the injury. All patients underwent surgical joint exploration and bullet removal, including total joint arthroplasty in 15 patients (14 total hip arthroplasty, one total shoulder arthroplasty) and joint arthrodesis for two patients (one radiocarpal joint and one ankle). All papers reported good functional outcomes following arthroplasty for lead arthropathy.
Eleven patients (6%) presented with systemic lead toxicity at a median of 82 months (range 8-624) following the initial injury.21,54,58,60,65,69,71,73,77 All patients who developed systemic lead toxicity were also diagnosed with lead arthropathy due to retained intra-articular bullets or bullet fragments. Involved joints included seven hips, two ankles, one knee and one wrist. Seven patients were commenced on chelation therapy at presentation and, following bullet removal, the systemic complications resolved in all cases. The intra-articular bullet was not removed in one patient, and this patient returned two years later with repeat acute systemic lead toxicity.69
Reviewing the management outcomes of acute presenting cases, a clear difference in septic complications is seen between the pre-antibiotic and antibiotic eras. Before the routine use of antibiotics, 52% of patients (39/75) developed an infection compared to 6% (14/251) following the widespread use of antibiotics. However, many of the initial papers reported on patients already infected at the time of presentation. All reported sepsis-related deaths (n = 9) and amputations (n = 25) also occurred before the routine use of antibiotics (Table II). During this period, management generally consisted of repeat open debridements, joint excision or amputation and daily antiseptic solution irrigation.
Management of acute injuries during the antibiotic era
Following the dawn of the antibiotic era, virtually every patient reported in the literature (99%, 198/199) who presented with an acute transarticular gunshot injury received systemic antibiotics as part of their management; the only patient who did not receive antibiotics left the hospital against medical advice before receiving medication (Table III).32First-generation cephalosporins were the antibiotic of choice in most publications (84%, 166/198). One paper combined gentamycin with a first-generation cephalosporin for seven patients who sustained gunshot injuries to the shoulder.29 One report used a third-generation cephalosporin following gunshot injuries to the hip.26 Although the authors did not expand on the motivation for using a third-generation rather than a first-generation cephalosporin, it is worthy to note that most of the patients in this report also sustained associated hollow viscus injuries.26
Most cases (80%, 202/251) underwent surgical arthrotomy, debridement and joint lavage. An open debridement was performed in 123 patients (61%). In 19 cases of gunshot injuries to the hip, a surgical hip dislocation was performed to facilitate bullet removal. An arthroscopic debridement was performed in 79 patients (39%).
Two papers investigated the need for operative intervention of transarticular gunshot injuries. A 2018 study by Maqungo et al. and a 2019 study by Shultz et al. compared antibiotics alone versus antibiotics in addition to operative treatment of transarticular gunshot injuries.32,61 Both studies showed no difference in infective complications, but when considering a baseline infection rate of 6% for acute presenting patients, these studies were possibly underpowered, and additional research is needed before the widespread adoption of this management strategy.
Intra-articular fractures were reported in 154 patients (65%).
These injuries were treated nonoperatively in 110 cases, by fracture fixation in 36 cases, arthroplasty in five cases (four shoulders, one hip)27,29 and shoulder arthrodesis in three patients.29 Poor outcomes requiring implant removal were experienced in all four shoulder arthroplasty cases (three periprosthetic joint infections and one painful implant loosening).29
Thirty-three papers reported 157 transarticular gunshot wounds to the hip, including 30 patients who sustained transabdominal or transpelvic bullet trajectory with associated hollow viscus injury.24,26,48,49,62,74 Bowel injury treatment consisted of primary repair in 20 cases and bowel diversion in ten patients. A significantly higher hip joint infection rate was seen in patients who sustained hollow viscus injury (11/30, 37%) than those who did not (6/127, 5%). The included papers did not provide enough information to discern any difference in infective complications following small bowel or large bowel injuries.
Late complications during the antibiotic era
Seventy patients presented with late complications (Table IV) following transarticular gunshot injuries at a median of 15.7 months after the injury (range 3-624); 26 patients had retained intra-articular bullets, 24 of whom developed lead arthropathy, of which 11 had signs of systemic lead toxicity. All (n = 70, 100%) were managed surgically.
Fifty-five patients underwent arthroplasty for complications following transarticular gunshot injuries. These patients presented at a median of 15.7 months (range 3-624) following the initial injury. Total joint arthroplasty of the hip was the most common procedure (n = 46). Eight cases (17%) were complicated by periprosthetic joint infection, including both patients who sustained associated hollow viscus injuries; five patients underwent revision arthroplasty, while one patient was treated by resection arthroplasty.30,50,54,63,65,67,71,77,79 Seven total elbow replacements were performed of which five patients (71%) required implant removal for either septic (n = 4) or aseptic loosening (n = 1).41 Good outcomes were reported in both patients who underwent shoulder arthroplasty.31,59
Bek et al. reported a 100% fusion rate following Ilizarov circular external fixation ankle arthrodesis in five patients who presented at a median of 27 months following gunshot injuries to the ankle joint.53
Bullet extraction techniques
Twenty-three publications reporting on the management of 44 patients focused on extraction techniques for retrieving retained bullets from 27 hips, 13 knees and four shoulder joints. Most publications (n = 20, 33 patients) described arthroscopic bullet removal, including 15 hips, 13 knees and four shoulder joints; one failed arthroscopic removal from a knee converted to an open arthrotomy.52 Two publications (11 patients) reported a 100% success rate, without complications, with the use of surgical hip dislocation for removal of bullets lodged in the femoral head and acetabulum.23,57 Krishnan et al. described a posterior approach and extracapsular cortical window to remove a bullet lodged in the posterior wall of the acetabulum.48
Most authors reported the successful use of a pituitary rongeur to grasp loose bullets within the joint cavity during arthroscopic removal.24,34,35,38,39,42,47 Budeyri and Cankus resorted to using an arthroscopic shaver with high-pressure suction to 'grasp' the bullet and rongeur claw after the rongeur claw broke off in the joint.66 Several authors noted instances of iatrogenic cartilage damage when embedded bullets were levered from their bony recesses. To circumvent this, Singleton et al. and Lee et al. described using a 3.2 mm threaded guide pin inserted into the bullet under power to capture the embedded bullet and extract it from the bone (Figure 5).49,52

Discussion
The management of transarticular gunshot injuries is currently based on limited high-quality evidence. This systematic review aimed to explore the literature reporting on treating these injuries to interpret the data and provide physicians with evidence to guide their management.
Together with a surge in global civilian gun-related violence, a drive for evidence-based medical care has stimulated a reciprocal increase in gunshot injury research over the last 20 years. A recent bibliometric analysis and the current review have confirmed that most publications on orthopaedic ballistic injuries originated from developed countries, including the United States of America and the United Kingdom, despite most gun-related violence reported in developing countries.80 El Salvador, Jamaica, Eswatini, Honduras and Venezuela, for example, have the highest firearm-related homicide rates.81 Yet, no publications on gunshot-related injuries have originated from any of these five countries. Researchers and non-governmental organisations in countries that see high numbers of firearm-related trauma should be encouraged to report their experience of managing these injuries to assist the development of global gun violence care pathways.
It is interesting to note that complication profiles were not consistent across different joints. The most prominent example was septic complications following transarticular gunshot injuries to the hip with associated hollow viscus injury, which was significantly higher than for any other joint (11/30, 37%). Different infection rates were also observed for the other joints: 15% for shoulder, 8% for hip, 2% for knee and 0% for wrist and elbow injuries. From arthroplasty and arthroscopy research, it is evident that different joints experience different infective complications, which might also be true for transarticular gunshot injuries.82-87 It might therefore be plausible to develop individualised care pathways for gunshot injuries based on each joint and associated injuries. This will, however, require more extensive cohort studies focusing on specific joint injuries.
The quality of the included publications limits recommendations that could be extracted from this review, most reports being either retrospective case series or case reports. No publications reported patient-reported outcomes following the management of gunshot-related transarticular injuries. The heterogeneity and quality of the included studies precluded performing a meta-analysis.
Conclusion
The contemporary management of transarticular gunshot injuries is based on limited high-quality evidence predominantly from developed countries. Modern antibiotic and surgical management practices have resulted in low overall septic complications; however, different joints have different injury and complication profiles. Future research should be aimed at identifying joint-specific evidence-based care pathways.
Key points
1. All intra-articular bullets or bullet fragments should be removed to mitigate long-term complications.
2. Gunshot injuries to the hip joint with associated hollow viscus injury have a high infection incidence and should be treated aggressively.
3. Although systemic lead toxicity is a severe complication, lead arthropathy is more common following retained intra-articular bullets and bullet fragments.
4. At present, there is insufficient evidence to propose nonoperative treatment of acute presenting transarticular gunshot injuries.
Ethics statement
The authors declare that this submission is in accordance with the principles laid down by the Responsible Research Publication Position Statements as developed at the 2nd World Conference on Research Integrity in Singapore, 2010.
Declaration
The authors declare authorship of this article and that they have followed sound scientific research practice. This research is original and does not transgress plagiarism policies.
Author contributions
NF: assembled the team of reviewers, coordinated the review process, conducted the primary review and compiled the manuscript
CA: screened eligible manuscripts, assisted with data extraction, reviewed, and approved the final submission
EJ: assisted with data extraction, reviewed and approved the final submission
ORCID
Ferreira N https://orcid.org/0000-0002-0567-3373
Anley C https://orcid.org/0000-0002-5983-3520
Joubert E https://orcid.org/0000-0001-6328-9110
References
1. Jakoet MS, Burger M, Van Heukelum M, et al. The epidemiology and orthopaedic burden of civilian gunshot injuries over a four-year period at a level one trauma unit in Cape Town, South Africa. Int Orthop. 2020;44(10):1897-904. https://doi.org/10.1007/s00264-020-04723-6. [ Links ]
2. Martin C, Thiart G, McCollum G, et al. The burden of gunshot injuries on orthopaedic healthcare resources in South Africa. S Afr Med J. 2017;107(7):626-30. https://doi.org/10.7196/SAMJ.2017.v107i7.12257. [ Links ]
3. Van Heukelum M, le Roux N, Jakoet S, Ferreira N. Financial burden of orthopaedic gunshot-related injury management at a major trauma centre. S Afr Med J. 2020;110(9):882-86. https://doi.org/10.7196/SAMJ.2020.v110i9.14638. [ Links ]
4. Maqungo S, Kauta N, Held M, et al. Gunshot injuries to the lower extremities: Issues, controversies and algorithm of management. Injury. 2020;51(7):1426-31. https://doi.org/10.1016/j.injury.2020.05.024. [ Links ]
5. Dickey RL, Barnes BC, Kearns RJ, Tullos HS. Efficacy of antibiotics in low-velocity gunshot fractures. J Orthop Trauma. 1989;3(1):6-10. https://doi.org/10.1097/00005131-198903010-00002. [ Links ]
6. Sathiyakumar V, Thakore RV, Stinner DJ, et al. Gunshot-induced fractures of the extremities: a review of antibiotic and debridement practices. Curr Rev Musculoskelet Med. 2015;8(3):276-89. https://doi.org/10.1007/s12178-015-9284-9. [ Links ]
7. Metcalf KB, Smith EJ, Wetzel RJ, et al. Comparison of clinical outcomes after intramedullary fixation of tibia fractures caused by blunt trauma and civilian gunshot wounds: a retrospective review. J Orthop Trauma. 2020;34(6):e208-13. https://doi.org/10.1097/BOT.0000000000001709. [ Links ]
8. Papasoulis E, Patzakis MJ, Zalavras CG. Antibiotics in the treatment of low-velocity gunshot-induced fractures: A systematic literature review trauma. Clin Orthop Relat Res. 2013;471(12):3937-44. https://doi.org/10.1007/s11999-013-2884-z. [ Links ]
9. Simpson BM, Wilson RH, Grant RE. Antibiotic therapy in gunshot wound injuries. Clin Orthop Relat Res. 2003;(408):82-85. https://doi.org/10.1097/00003086-200303000-00008. [ Links ]
10. Sackett DL. Rules of evidence and clinical recommendations for the management of patients. Can J Cardiol. 1993;9(6):487-89. https://doi.org/10.1378/chest.95.2_Supplement.2S. [ Links ]
11. Tatum. Gunshot wound of the shoulder. Lancet. 1867;89(2280):565. https://doi.org/10.1016/S0140-6736(02)51608-1. [ Links ]
12. Lupton. Gunshot wound of left knee-joint with longitudinal and transverse fracture of the femur. Lancet. 1880;115(2961):837. https://doi.org/10.1016/S0140-6736(02)36994-0. [ Links ]
13. Sympson. Country hospital, Lincoln. Gunshot injury; Destruction of right knee-joint and amputation of thigh; Aneurism of left femoral artery treated by digital pressure and Esmarch's bandage. Lancet. 1881;117(2999):292-93. https://doi.org/10.1016/S0140-6736(02)34118-7. [ Links ]
14. MacCormac W. Gunshotinjuryin the neighbourhood of the knee-joint. Lancet. 1886;127(3261):389-91. https://doi.org/10.1016/S0140-6736(00)59100-4. [ Links ]
15. Thomson GS. Perforating gunshot wounds of the chest and of the wrist joint, both in the same patient and followed by recovery. Ind Med Gaz. 1890;25(9):270-71. http://www.ncbi.nlm.nih.gov/pubmed/29000400. [ Links ]
16. Gray HMW. Treamtnet of gunshot wounds of the knee-joint. BMJ. 1915;2(2845):41-43. https://doi.org/10.1136/bmj.2.2845.41. [ Links ]
17. Swan RHJ. The treatment of severe infected gunshot injuries of the shoulder and elbow joints. Lancet. 1917;189(4884):524-29. https://doi.org/10.1016/S0140-6736(01)38916-X. [ Links ]
18. Charles R. Gunshot wounds of the knee-joint: the conservative operation at the casualty clearing station. BMJ. 1918;1(3000):713-17. https://doi.org/10.1136/bmj.L3000.713. [ Links ]
19. Neve A. Gunshot wounds of the knee-joint with septic arthritis. Ind Med Gaz. 1918;53(12):459-60. http://www.ncbi.nlm.nih.gov/pubmed/29006719. [ Links ]
20. Buxton JD. Gunshot wounds of the elbow-joint. Lancet. 1943;242(6274):663-65. https://doi.org/10.1016/S0140-6736(00)88214-8. [ Links ]
21. Switz DM, Elmorshidy ME, Deyerle WM. Bullets, joints, and lead intoxication. A remarkable andinstructive case. Arch Intern Med. 1976;136(8):939-41. https://doi.org/10.1001/archinte.136.8.939. [ Links ]
22. Lai CC. Delayed appearance of popliteal cyst caused by a bullet. J Trauma Inj Infect Crit Care. 1977;17(2):144-50. https://doi.org/10.1097/00005373-197702000-00009. [ Links ]
23. Delaney R, Albright M, Rebello G. Utilization of the safe surgical dislocation approach of the hip to retrieve a bullet from the femoral head. Case Rep Orthop. 2011;2011:160591. https://doi.org/10.1155/2011/160591. [ Links ]
24. Al-Asiri J, Wong I. Arthroscopic bullet removal from the acetabulum (hip joint). J Surg Tech Case Rep. 2012;4(2):121-25. https://doi.org/10.4103/2006-8808.110260. [ Links ]
25. De Witte PB, Rhemrev SJ. Diagnostics and treatment of low-velocity gunshot wounds in the hip joint region. Eur Orthop Traumatol. 2012;3(3):205-207. https://doi.org/10.1007/s12570-012-0124-8. [ Links ]
26. Najibi S, Matta JM, Dougherty PJ, Tannast M. Gunshot wounds to the acetabulum. J Orthop Trauma. 2012;26(8):451-59. https://doi.org/10.1097/BOT.0b013e31822c085d. [ Links ]
27. Ho C-J, Hung S-H, Huang H-T, et al. Successful treatment of a delayed presentation of a gunshot injury to the femoral neck in an elderly man: a case report. Eur J Orthop Surg Traumatol. 2012;22(1):131-33. https://doi.org/10.1007/s00590-012-0975-2. [ Links ]
28. Cvetanovich GL, Erickson B, Haughom BD, et al. Initial evaluation of gunshot wounds about the knee: bullet-induced synovitis. Am J Emerg Med. 2013;31(8):1291.e3-1291.e5. https://doi.org/10.1016/j.ajem.2013.03.053. [ Links ]
29. Zsoldos CM, Basamania CJ, Bal GK. Shoulder fusion after a self-inflicted gunshot wound: An injury pattern and treatment option. Bone Jt J. 2013;95 B(6):820-24. https://doi.org/10.1302/0301-620X.95B6.31447. [ Links ]
30. Naziri Q, Issa K, Rizkala A, et al. Posttraumatic arthritis from gunshot injuries to the hip requiring a primary THA. Orthopedics. 2013;36(12):E1549-E54. https://doi.org/10.3928/01477447-20131120-21. [ Links ]
31. Amri K, Chefi MAA, Znagui T, et al. Resurfacing shoulder hemi arthroplasty in ballistic injuries. A case report. Int J Surg Case Rep. 2019;65:48-51. https://doi.org/ https://doi.org/10.1016/j.ijscr.2019.10.027. [ Links ]
32. Shultz CL, Schrader SN, Garbrecht EL, et al. Operative versus nonoperative management of traumatic arthrotomies from civilian gunshot wounds. Iowa Orthop J. 2019;39(1):173-77. http://www.ncbi.nlm.nih.gov/pubmed/31413691. [ Links ]
33. Tornetta P, Hui RC. Intraarticular findings after gunshot wounds through the knee. J Orthop Trauma. 1997;11(6):422-24. https://doi.org/10.1097/00005131-199708000-00009. [ Links ]
34. Cory JW, Ruch DS. Arthroscopic removal of a .44 caliber bullet from the hip. Arthroscopy. 1998;14(6):624-26. https://doi.org/10.1016/s0749-8063(98)70061-1. [ Links ]
35. Sansone V, Mora L, De Spirito D. Arthroscopic retrieval of an unusual foreign body of the knee. Arthroscopy. 2002;18(2):E6. https://doi.org/10.1053/jars.2002.30711. [ Links ]
36. Cho MS, Warme WJ. Arthroscopic treatment of a transarticular low-velocity gunshot wound using tractoscopy. Arthroscopy. 2002;18(5):532-37. https://doi.org/10.1053/jars.2002.31963. [ Links ]
37. Petersen W, Beske C, Stein V, Laprell H. Arthroscopical removal of a projectile from the intra-articular cavity of the knee joint. Arch Orthop Trauma Surg. 2002;122(4):235-36. https://doi.org/10.1007/s00402-001-0373-4. [ Links ]
38. Teloken MA, Schmietd I, Tomlinson DP. Hip arthroscopy: a unique inferomedial approach to bullet removal. Arthroscopy. 2002;18(4):E21. https://doi.org/10.1053/jars.2002.32232. [ Links ]
39. Mineo RC, Gittins ME. Arthroscopic removal of a bullet embedded in the acetabulum. Arthroscopy. 2003;19(9):E121-24. https://doi.org/10.1016/j.arthro.2003.09.014. [ Links ]
40. Tarkin IS, Hatzidakis A, Hoxie SC, et al. Arthroscopic treatment of gunshot wounds to the shoulder. Arthroscopy. 2003;19(1):85-89. https://doi.org/10.1053/jars.2003.50024. [ Links ]
41. Demiralp B, Komurcu M, Ozturk C, et al. Total elbow arthroplasty in patients who have elbow fractures caused by gunshot injuries: 8- to 12-year follow-up study. Arch Orthop Trauma Surg. 2008;128(1):17-24. https://doi.org/10.1007/s00402-007-0324-9. [ Links ]
42. Gupta RK, Aggarwal V. Late arthroscopic retrieval of a bullet from hip joint. Indian J Orthop. 2009;43(4):416-19. https://doi.org/10.4103/0019-5413.54764. [ Links ]
43. Sozen YV, Polat G, Kadioglu B, et al. Arthroscopic bullet extraction from the hip in the lateral decubitus position. Hip Int. 2010;20(2):265-68. https://doi.org/10.1177/112070001002000221. [ Links ]
44. Bartkiw MJ, Sethi A, Coniglione F, et al. Civilian gunshot wounds of the hip and pelvis. J Orthop Trauma. 2010;24(10):645-52. https://doi.org/10.1097/BOT.0b013e3181cf03ea. [ Links ]
45. Mollan RA, Beavis V. A curious gunshot injury. Injury. 1978;9(4):327-28. https://doi.org/10.1016/s0020-1383(77)80056-9. [ Links ]
46. Goldman A, Minkoff J, Price A, Krinick R. A posterior arthroscopic approach to bullet extraction from the hip. J Trauma. 1987;27(11):1294-300. https://doi.org/10.1097/00005373-198711000-00016. [ Links ]
47. Otero F, Cuartas E. Arthroscopic removal of bullet fragments from the subacromial space of the shoulder. Arthroscopy. 2004;20(7):754-56. https://doi.org/10.1016/j.arthro.2004.04.055. [ Links ]
48. Krishnan KM, Vashista GN, Sinha A, Lin K. Transabdominal gun shot injury to the hip joint - a new open technique for removal of the bullet. Inj Extra. 2004;35(10):81-84. https://doi.org/10.1016/j.injury.2004.06.009. [ Links ]
49. Singleton SB, Joshi A, Schwartz MA, Collinge CA. Arthroscopic bullet removal from the acetabulum. Arthroscopy. 2005;21(3):360-64. https://doi.org/10.1016/j.arthro.2004.10.005. [ Links ]
50. Rehman MA, Umer M, Sepah YJ, Wajid MA. Bullet-induced synovitis as a cause of secondary osteoarthritis of the hip joint: A case report and review of literature. J Med Case Rep. 2007;1(1):171. https://doi.org/10.1186/1752-1947-1-171. [ Links ]
51. Mahirogullari M, Cilli F, Akmaz I, et al. Acute arthroscopic removal of a bullet from the shoulder. Arthroscopy. 2007;23(6):676.e1-3. https://doi.org/10.1016/j.arthro.2006.01.022. [ Links ]
52. Lee GH, Virkus WW, Kapotas JS. Arthroscopically assisted minimally invasive intraarticular bullet extraction: technique, indications, and results. J Trauma. 2008;64(2):512-16. https://doi.org/10.1097/TA.0b013e31814699ee. [ Links ]
53. Bek DD, Demiralp B, Kürklü M, et al. Ankle arthrodesis using an Ilizarov external fixator in patients wounded by landmines and gunshots. Foot Ankle Int. 2008;29(2):178-84. https://doi.org/10.3113/FAI.2008.0178. [ Links ]
54. Oomen JWPM, Smits BW, Swinkels DW, et al. A toxic shot from the hip. J Neurol Neurosurg Psychiatry. 2011;82(3):353-54. https://doi.org/10.1136/jnnp.2009.191312. [ Links ]
55. Keskinbora M, Yalçin S, Oltulu i, Erdil ME, Örmeci T. Compartment syndrome following arthroscopic removal of a bullet in the knee joint after a low-velocity gunshot injury. Clin Orthop Surg. 2016;8(1):115-8. https://doi.org/10.4055/cios.2016.81.115. [ Links ]
56. Çatma MF, Ünlü S, Ersan Ö, Öztürk A. Treatment of the bullet, traversing femoral neck, lodged in hip joint: initial arthroscopic removal and subsequent cartilage repair. J Orthop case reports. 2016;6(4):13-16. https://doi.org/10.13107/jocr.2250-0685.548. [ Links ]
57. Maqungo S, Hoppe S, Kauta JN, et al. Surgical hip dislocation for removal of retained intra-articular bullets. Injury. 2016;47(10):2218-22. https://doi.org/10.1016/j.injury.2016.06.020. [ Links ]
58. McAninch SA, Adkison J, Meyers R, Benham M. Bullet fragment-induced lead arthropathy with subsequent fracture and elevated blood lead levels. Baylor Univ Med Cent Proc. 2017;30(1):88-91. https://doi.org/10.1080/08998280.2017.11929543. [ Links ]
59. Dosari MAA Al, Hameed S, Mukhtar K, Elmhiregh A. Reverse shoulder arthroplasty for deltoid-deficient shoulder following latissimus dorsi flap transfer. Case report. Int J Surg Case Rep. 2017;39:256-59. https://doi.org/10.1016/jijscr.2017.08.042. [ Links ]
60. Ramji Z, Laflamme M. Ankle lead arthropathy and systemic lead toxicity secondary to a gunshot wound after 49 years: a case report. J Foot Ankle Surg. 2017;56(3):648-52. https://doi.org/10.1053/j.jfas.2016.12.005. [ Links ]
61. Maqungo S, Swan A, Naude P, et al. The management of low velocity transarticular gunshot injuries: A pilot study. SA Orthop J. 2018;17(3):25-27. https://doi.org/10.17159/2309-8309/2018/v17n2a4. [ Links ]
62. Ferro FP, Bessa FS, Ejnisman L, et al. Arthroscopic bullet removal from the hip joint and concurrent treatment of associated full-thickness chondral defects: A case report. SAGE Open Med Case Reports. 2019;7:2050313X1982967. https://doi.org/10.1177/2050313X19829670. [ Links ]
63. Pazarci O, Kilinc S, Camurcu Y Bulut O. Total hip arthroplasty after hip joint gunshot injury. J Orthop Surg. 2019;27(3):1-6. https://doi.org/10.1177/2309499019873113. [ Links ]
64. Fournier MN, Rider CM, Olinger CR, et al. Arthroscopic treatment of a low-velocity gunshot injury to a primary total hip arthroplasty. JBJS Case Connect. 2019;9(1):e18. https://doi.org/10.2106/JBJS.CC.18.00204. [ Links ]
65. Rohlfing G, Refaat M, Kollmorgen R. Pseudotumor caused by a retained intra-articular bullet: a case report. JBJS Case Connect. 2020;10(1):e0209. https://doi.org/10.2106/JBJS.CC.19.00209. [ Links ]
66. Budeyri A, Cankus MC. Shaver suction technique for troubleshooting in arthroscopic double foreign body removal from the hip joint. Cureus. 2020;12(10):e10911. https://doi.org/10.7759/cureus.10911. [ Links ]
67. Özden R, Davut S, Dogramaci Y, et al. Treatment of secondary hip arthritis from shell fragment and gunshot injury in the Syrian civil war. J Orthop Surg Res. 2020;15(1):464. https://doi.org/10.1186/s13018-020-01993-z. [ Links ]
68. Maqungo S, Fegredo D, Brkljac M, Laubscher M. Gunshot wounds to the hip. J Orthop. 2020;22(August):530-34. https://doi.org/10.1016/jjor.2020.09.018. [ Links ]
69. Dillman RO, Crumb CK, Lidsky MJ. Lead poisoning from a gunshot wound. Report of a case and review of the literature. Am J Med. 1979;66(3):509-14. https://doi.org/10.1016/0002-9343(79)91083-0. [ Links ]
70. Parisien JS, Esformes I. The role of arthroscopy in the management of low-velocity gunshot wounds of the knee joint. Clin Orthop Relat Res. 1984;(185):207-13. [ Links ]
71. Beazley WC, Rosenthal RE. Lead intoxication 18 months after a gunshot wound. Clin Orthop Relat Res. 1984;(190):199-203. http://www.ncbi.nlm.nih.gov/pubmed/6488632. [ Links ]
72. Sclafani SJ, Vuletin JC, Twersky J. Lead arthropathy: arthritis caused by retained intra-articular bullets. Radiology. 1985;156(2):299-302. https://doi.org/10.1148/radiology.156.2.4011890. [ Links ]
73. Slavin RE, Swedo J, Cartwright JJ, et al. Lead arthritis and lead poisoning following bullet wounds: a clinicopathologic, ultrastructural, and microanalytic study of two cases. Hum Pathol. 1988;19(2):223-35. https://doi.org/10.1016/s0046-8177(88)80353-8. [ Links ]
74. Becker VV, Brien WW, Patzakis M, Wilkins J. Gunshot injuries to the hip and abdomen: the association of joint and intra-abdominal visceral injuries. J Trauma. 1990;30(11):1324-29. https://doi.org/10.1097/00005373-199011000-00003. [ Links ]
75. Berg EE, Ciullo JV. Arthroscopic debridement after intraarticular low-velocity gunshot wounds. Arthroscopy. 1993;9(5):576-79. https://doi.org/10.1016/S0749-8063(05)80408-6. [ Links ]
76. Janzen DL, Tirman PF, Rabassa AE, Kumar S. Lead 'bursogram' and focal synovitis secondary to a retained intraarticular bullet fragment. Skeletal Radiol. 1995;24(2):142-44. https://doi.org/10.1007/BF00198079. [ Links ]
77. Peh WC, Reinus WR. Lead arthropathy: a cause of delayed onset lead poisoning. Skeletal Radiol. 1995;24(5):357-60. https://doi.org/10.1007/BF00197067. [ Links ]
78. Latosiewicz R, Murawski J, Skowrohski J. Bilateral knee gunshot wounds successfully treated with arthroscopic bullet retrieval: a case report. Arthroscopy. 1995;11(1):104-105. https://doi.org/10.1016/0749-8063(95)90096-9. [ Links ]
79. Madureira PR de, De Capitani EM, Vieira RJ, et al. Lead poisoning after gunshot wound. Sao Paulo Med J. 2000;118(3):78-80. https://doi.org/10.1590/S1516-31802000000300006. [ Links ]
80. Held M, Engelmann E, Dunn R, et al. Gunshot induced injuries in orthopaedic trauma research. A bibliometric analysis of the most influential literature. Orthop Traumatol Surg Res. 2017;103(5):801-807. https://doi.org/10.1016/j.otsr.2017.05.002. [ Links ]
81. Homicide rates from firearms, 2017. Available from: https://ourworldindata.org/grapher/homicide-rates-from-firearms. Accessed 18 May 2021. [ Links ]
82. Patton D, Kiewiet N, Brage M. Infected total ankle arthroplasty. Foot Ankle Int. 2015;36(6):626-34. https://doi.org/10.1177/1071100714568869. [ Links ]
83. Rangan A, Falworth M, Watts AC, et al. Investigation and management of periprosthetic joint infection in the shoulder and elbow: evidence and consensus based guidelines of the British Elbow and Shoulder Society. Shoulder Elbow. 2018;10(1 Suppl):S5-S9. https://doi.org/10.1177/1758573218772976. [ Links ]
84. Ahmed SS, Haddad FS. Prosthetic joint infection. Bone Joint Res. 2019;8(11):570-72. https://doi.org/10.1302/2046-3758.812.BJR-2019-0340. [ Links ]
85. Zardi EM, Franceschi F. Prosthetic joint infection. A relevant public health issue. J Infect Public Health. 2020;13(12):1888-91. https://doi.org/10.1016/jjiph.2020.09.006 [ Links ]
86. Voss A, Pfeifer CG, Kerschbaum M, et al. Post-operative septic arthritis after arthroscopy: modern diagnostic and therapeutic concepts. Knee Surg Sports Traumatol Arthrosc. 2021;29(10):3149-58. https://doi.org/10.1007/s00167-021-06525-8. [ Links ]
87. Sircana G, Passiatore M, Capasso L, et al. Infections in arthroscopy. Eur Rev Med Pharmacol Sci. 2019;23(2):279-87. https://doi.org/10.26355/eurrev_201904_17502. [ Links ]
Received: June 2021
Accepted: September 2021
Published: March 2022
* Corresponding author: nferreira@sun.ac.za
Editor: Prof. Sithombo Maqungo, University of Cape Town, Cape Town, South Africa
Funding: No funding was received for this study.
Conflict of interest: The authors declare they have no conflicts of interest that are directly or indirectly related to the research.














