Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.21 n.1 Centurion 2022
http://dx.doi.org/10.17159/2309-8309/2022/v21n1a4
KNEE
Not strong enough? Movements generated during clinical examination of sagittal and rotational laxity in a cadaver knee
Johan A le RouxI; Carel W BezuidenhoutII; Juan KlopperI; Hayden HobbsIII; Richard von BormannIV; Michael HeldI, IV, *
IOrthopaedic Research Unit, Department of Orthopaedic Surgery, Groote Schuur Hospital, University of Cape Town, South Africa
IIDepartment of Orthopaedics, Kimberley Hospital Complex, South Africa
IIILife Vincent Palotti Hospital, Cape Town, South Africa
IVNetcare Christiaan Barnard Hospital, Cape Town, South Africa
ABSTRACT
BACKGROUND: Injury to the anterior cruciate ligament (ACL) is associated with sagittal and rotational laxity, which is exacerbated by damage to the anterolateral capsuloligamentous structures, also known as the anterolateral ligament (ALL). The amount of laxity reported in biomechanical studies might be clinically insignificant during a surgeon's examination, possibly influencing clinical judgement. We aimed to measure whether the motion generated by clinicians in a cadaver model after the ACL and ALL were transected is clinically significant
METHODS: A group of orthopaedic surgeons and trainees examined a cadaver knee for sagittal and rotational laxity at 30° and 90° with intact ligaments, after the ACL was transected, and after the ACL and ALL were transected. The examiners were blinded to the dissection process. Rotational and sagittal movements during these examinations were recorded by a computer-assisted surgery (CAS) system
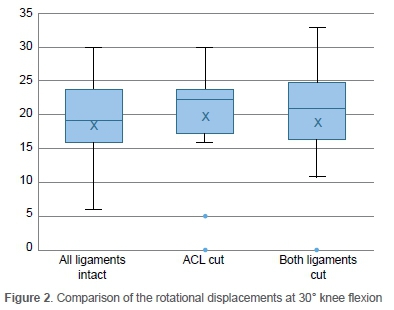
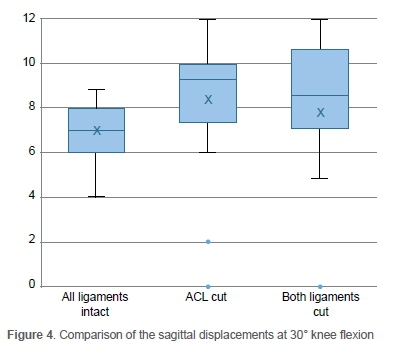
RESULTS: Twenty-four orthopaedic surgeons took part in the study. The median sagittal plane motion captured by CAS at 30° flexion was 7 mm (IQR 2 mm, p-value 0.32) in the intact knee, 9 mm (IQR 1 mm, p-value 0.34) after the ACL was cut and 9 mm (IQR 3 mm, p-value 0.63) after ACL and ALL were cut. The median arc of rotational motion at 30° was 19° (IQR 7°, p-value 0.12) in the intact knee, 24° (IQR 5°, p-value 0.56) after the ACL was cut, and 22° (IQR 6°, p-value 0.8) after the ACL and ALL were cut. None of the differences in these movements was significant
CONCLUSION: The surgeons could not generate significant differences in sagittal or rotational motion in a cadaver model, which could be objectively detected by CAS, when examining the intact knee, ACL deficient (only), or combined ACL and ALL deficient knee. This challenges the utility of known clinical tests and calls for improved objective laxity assessment tools to provide input in clinical decision-making and measure outcomes of these injuries
Level of evidence: Level 5
Keywords: knee, anterolateral ligament, anterior drawer's test, pivot shift, rotatory instability, anterior cruciate ligament, iliotibial band, Kaplan fibres
Introduction
One of the most intriguing questions in the management of anterior cruciate ligment (ACL)-deficient knees is whether we can define abnormal translation or rotation.1 The anatomic and biomechanical complexities to answer this question have challenged surgeons for more than a century after Paul Segond described the anterolateral ligamentous structure of the knee.2 Their role in rotatory stability has gained significant interest recently;3 nevertheless, clinical testing remains controversial.
An anterolateral ligament (ALL) injury affects knee stability, which can potentially be diagnosed by the pivot-shift manoeuvre, anterior translation and increased internal rotation of the tibia in relation to the femur.3-5 However, none of these clinical tests could be validated with high accuracy to diagnose an ALL injury.6 Most surgeons therefore utilise clinical factors and associated injuries such as hypermobility, high grade meniscal tears, expected patient compliance or age to decide on ALL reconstruction.6
Previous biomechanical studies have managed to confirm a statistically significant contribution of the ALL to the stability of the knee, but these movements were insignificant, considering their detectability in millimetres and degrees by clinicians.3,5 External devices such as the KT-1000 (MED-metric, San Diego, CA, US) or the Telos stress device (Telos GmbH, Laubscher, Holstein, Switzerland) for anterior-posterior knee laxity may measure knee laxity more objectively but significant differences have been found when compared to actual tibio-femoral translation measured by optic tracking devices or roentgen stereophotogrammetry (RSA).7-9
Currently no studies have evaluated the motion generated by a large group of clinicians after sequential sectioning of knee ligaments. A decision for further objective evaluation and magnetic resonance imaging (MRI) is often based on the clinical examination by the surgeon, who will likely decide against further investigations with insignificant motion generated. Also, in resource-constrained settings without access to MRI or external ligament stress devices, the clinical exam is the only way to detect pathologic ligament laxity. The goal of our study was therefore to determine if an ACL and ALL deficiency would cause significant clinical laxity in a knee, using an optic motion tracker device. Are clinicians strong enough to generate clinically significant motion in an ACL and ALL-deficient knee?
Methods
This study protocol was formally approved by the local institutional review board and written consent was obtained from all participants.
An optical tracker system in the form of a computer-assisted surgery (CAS) navigation system (Pi-Galileo, Smith and Nephew, Memphis, Tennessee) was used to measure sagittal and rotational movements generated during clinical examination of a cadaver knee with intact ligaments, at 30° and 90° of flexion. For this a previously described protocol by Martelli et al. was adapted.10 This was then compared to movements generated after sectioning of the ACL and finally the ALL. The examination was performed by 24 members of an orthopaedic department at a university hospital with various levels of clinical experience, who were blinded to the ligamentous stability of the knee, and the sectioning of ligaments (Table I).
A fresh frozen and thawed cadaver, with a normal hip and knee range of motion, and intact collateral and cruciate ligaments, was used. The specimen was donated for use by Smith and Nephew. The pelvis and both lower limbs were preserved to determine the hip centre of rotation for calibration. A midline skin incision and mini medial parapatellar arthrotomy was done to confirm the presence of an intact ACL, posterior cruciate ligament (PCL), iliotibial band (ITB), and anterolateral joint capsule. Optical sensors for CAS were secured percutaneously to the femur and the tibia, in such a manner that it would not be in the way while performing an examination of the knee (Figure 1). Twenty-four clinicians with various levels of expertise were asked to assess the sagittal and rotational stability of the leg, with the results captured by the CAS system.

The ACL was cut mid-substance, ensuring the PCL or anterior horn of the lateral meniscus were not damaged. The knee was then again examined by the 24 study participants. After this the anterolateral capsule with the ALL was cut from the anterior border of the lateral collateral ligament (LCL) sub-meniscal to the posterior border of the ITB at its insertion of Gerdy's tubercle. The medial arthrotomy and skin were sutured each time after the initial inspection of the ligaments and sequential sectioning of the ACL and ALL. In this study, the term 'laxity' was used to describe a passive response, described as 'motion' of the knee to an external force or torque applied by clinicians.1
The sample size was calculated for a power of 0.8 using Lin's concordance correlation coefficient power analysis with an alpha value of 0.05. The normality of the data was determined by drawing a histogram, using a Shapiro-Wilk test and the Levene test. Normal data was summarised with parametric analysis. The Wilcoxon rank test was used to compare non-parametric data to detect differences in measurements after each ligament was cut. A p-value of < 0.05 was defined as statistically significant. Sagittal plane movement of more than 5 mm (the upper limit for grade 1 injury) and rotational movement of more than 10° was chosen as a clinically significant difference. Box-and-whisker plots were used to illustrate the comparison of the median and interquartile ranges (IQR) of data of each group.
Results
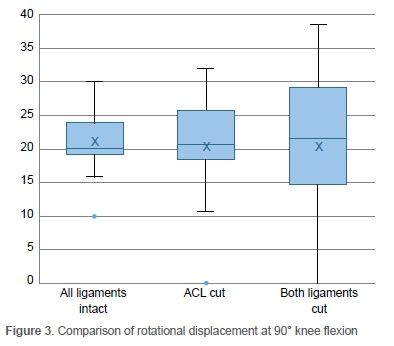
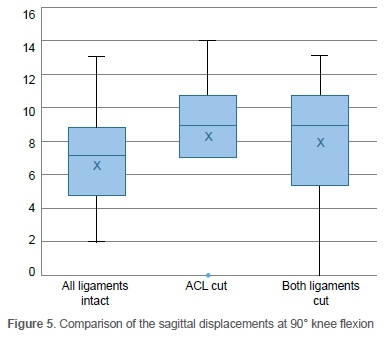
Twenty-four participants with a wide range of clinical experience took part in this study (Table I). The median sagittal plane laxity of the tibia in relation to the femur as captured by CAS at 30° flexion was 7 mm (IQR 2 mm, p-value 0.32) in the intact knee, 9 mm (IQR 1 mm, p-value 0.34) after the ACL was cut and 9 mm (IQR 3 mm, p-value 0.63 ) after the ACL and ALL were cut. At 90° flexion the translation was 7 mm (IQR 3.2 mm, p-value 0.6) in the intact knee, 10 mm (IQR 7.2 mm, p-value 0.24) after the ACL was sectioned, and 15 mm (IQR 5, p-value 0.12) after the ACL and ALL were cut. The largest difference was found after sectioning of the ACL, with minimal difference after the ALL was also sectioned. The median arc of internal rotational laxity measurements as captured by CAS at 30° was 19° (IQR 7°, p-value 0.33) in the intact knee, 24° (IQR 5°, p-value 0.13) after the ACL was cut and 22° (IQR 6°, p-value 0.06) after the ACL and ALL were cut, and 22 mm (IQR 15 mm, p-value 0.26), 30 mm (IQR 18.7 mm, p-value 0.5) and 40 mm (IQR 20 mm, p-value 0.1) with the knee in 90° flexion. The greatest increases occurred after the ACL was cut with minimal change after the ALL was cut (Figures 2-5).
Discussion
This study showed that clinicians generated negligible translational and rotational movement in a cadaver knee after the ACL and ALL were sectioned. Other biomechanical studies performed with constant load generators have shown similar results.3-5,11 The findings of these in vitro studies are similar to ours and interesting when considering the anterior drawer and Lachman tests have been validated to be sensitive tests for diagnosing an ACL injury.12
Miura et al. conducted an in vivo study comparing laxity of both knees in patients with confirmed ipsilateral ACL injuries. A side-to-side difference of 8.6 mm during the Lachman test in 30° flexion was reported, but only a 4.2 mm difference when comparing anterior tibial drawer tests in 90° of flexion.13 A study by Bull et al. also recorded only a 4.2 mm difference with an anterior drawer test at 30° and 90° knee flexion, when comparing knee laxity before and after an ACL reconstruction.14 Similarly, the motion differences in our study were below 3 mm in translation and 3° in internal rotation before and after sectioning of the ACL and the ALL. These are minute compared to commonly used clinical classification systems of at least 5 mm increments in translation and 10° in rotation.12,15
The second finding was that sectioning of the ALL had little effect on the internal tibial rotation and anterior translation compared to the ACL-deficient knee. This is in line with the findings of Kittl et al., who defined the posterior fibres of the iliotibial tract (ITT) as the main structure restricting internal rotation of the tibia and not the ALL as previously thought.16 However, the contribution to an increase in laxity for each ligament was quantified in percentages, and not in millimetres or degrees, and exact values are not available. Similar findings were reported by Sonnery-Cottet et al., confirming the ITB as the primary restrictor to internal rotation of the tibia.3
An interesting finding of the study was the range and maximum displacements generated with the knee in 30° and 90° of flexion before sectioning of the ligaments, namely 11 mm (range 4-9) and 13 mm (range 2-13). Despite this large initial range, the increase in the maximum and average displacements were, however, minimal after the ACL was cut (Figures 4 and 5).
The study had limitations. Only one cadaver was used, and the inherent laxity, or presence of hyperlaxity, was unknown. However, it allowed a standardised evaluation of movement generated by various clinicians in a controlled fashion and was mainly used for assessment before and after sectioning of ligaments. Secondly, the movement generated might be influenced by the sectioning technique used to prepare the cadaver. Although the anterolateral capsule was sectioned, the ITB and posterior Kaplan fibres were not cut, even though they are described as a stabiliser against translational and rotational instability.16 Yet, the cadaver set-up and dissection was done in a similar way to previous biomechanical cadaver studies to allow comparison.3 Future studies should address this by a further sectioning of the posterior Kaplan fibres. Thirdly, this artificial injury to the ACL or ALL might not have taken into account the associated muscular, capsular, meniscal or liga-mentous injuries which are often present in a clinical scenario and which could generate increased laxity. However, mapping movement with CAS by a large number of clinicians in a clinical scenario is not feasible. Lastly, it might have been beneficial to include a pivot-shift test to test the translational movement during the pivot-shift test. We only tested movement in single planes, i.e. sagittal and translational translation.
Furthermore, the 24 participants were only asked to assess for sagittal translation in 30° and 90° knee flexion, and rotational laxity in 30° and 90° of knee flexion, without a specific brief to assess the extremes of motion or perform specific tests (i.e., the pivot-shift test). This could have reduced the difference of movements.
Conclusion
This observational study showed that no significant rotational and sagittal motion was generated by clinicians when comparing a cadaver knee with intact ligaments to sequential sectioning of ACL and ALL - findings that are in keeping with similar studies on the topic and contrary to laxity generated when these injuries happen in vivo. Future cadaver studies should include the pivot-shift test and sectioning of the posterior Kaplan fibres, but ideally these findings should be confirmed in true ACL injuries to maximise the clinical benefit.
Ethics statement
The authors declare that this submission is in accordance with the principles laid down by the Responsible Research Publication Position Statements as developed at the 2nd World Conference on Research Integrity in Singapore, 2010. Prior to commencement of the study, ethical approval was obtained from the University of Cape Town Human Research Ethics Committee (HREC), number 472/2016. Written consent was obtained from all participants.
Declaration
The authors declare authorship of this article and that they have followed sound scientific research practice. This research is original and does not transgress plagiarism policies.
Author contributions
JAR: primary author, design, data contribution, manuscript preparation
CWB: conceptualisation, design, manuscript preparation
JK: conceptualisation, design, data analysis, manuscript preparation
HH: conceptualisation, design, data collection
RB: conceptualisation, design, manuscript preparation
MH: supervisor, conceptualisation, design, data collection, manuscript preparation
ORCID
Le Roux JA https://orcid.org/0000-0002-5658-6827
Bezuidenhout CW https://orcid.org/0000-0001-7024-4914
Klopper J https://orcid.org/0000-0002-7325-1906
Von Bormann R https://orcid.org/0000-0002-4546-3143
Held M https://orcid.org/0000-0002-0671-0439
References
1. Musahl V, Hoshino Y, Becker R, Karlsson J. Rotatory knee laxity and the pivot shift. Knee Surg Sport Traumatol Arthrosc. 2012;20(4):601-602. https://doi.org/10.1007/s00167-011-1844-y. [ Links ]
2. Segond P. Recherches cliniques et experimentales sur les epanchements sanguine der genou par entorse [Clinical and experimental research on board effusions of Knee Sprain. Prog Med VII. 1879;7:297-99, 3:319-21. [ Links ]
3. Sonnery-Cottet B, Lutz C, Daggett M, et al. The involvement of the anterolateral ligament in rotational control of the knee. Am J Sports Med. 2015;44(5):1209-14. https://doi.org/10.1177/0363546515625282. [ Links ]
4. Monaco E, Maestri B, Labianca L, et al. Navigated knee kinematics after tear of the ACL and its secondary restraints: preliminary results. Orthopedics. 2010;33(10 Suppl):87-93. https://doi.org/10.3928/01477447-20100510-58. [ Links ]
5. Ferretti A, Labianca L, Maestri B, et al. Navigated knee kinematics after cutting of the ACL and its secondary restraint. Knee Surg Sports Traumatol Arthrosc. 2012;20(5):870-77. https://doi.org/10.1007/s00167-011-1640-8. [ Links ]
6. Sonnery-Cottet B, Daggett M, Fayard JM, et al. Anterolateral Ligament Expert Group consensus paper on the management of internal rotation and instability of the anterior cruciate ligament-deficient knee. J Orthop Traumatol. 2017;18(2):91-106. https://doi.org/10.1007/s10195-017-0449-8. [ Links ]
7. Fleming BC, Brattbakk B, Peura GD, Badger GJ, Beynnon BD. Measurement of anterior-posterior knee laxity: a comparison of of three techniques. J Orthop Res. 2002;20(3):421-26. https://doi.org/10.1016/s0736-0266(01)00134-6. [ Links ]
8. Monaco E, Labianca L, Maestri B, et al. Instrumented measurements of knee laxity: KT-1000 versus navigation. Knee Surg Sports Traumatol Arthrosc. 2009;17(6):617-21. https://doi.org/10.1007/s00167-009-0724-1. [ Links ]
9. Jonsson H, Kärrholm J, Elmqvist LG. Laxity after cruciate ligament injury in 94 knees: the KT-1000 arthrometer versus roentgen stereophotogrammetry. Acta Orthop Scand. 1993;64(5):567-70. https://doi.org/10.3109/17453679308993694. [ Links ]
10. Martelli S, Zaffagnini S, Bignozzi S, et al. Validation of a new protocol for computerassisted evaluation of kinematics of double-bundle ACL reconstruction. Clin Biomech. 2006;21(3):279-87. https://doi.org/10.1016/jclinbiomech.2005.10.009. [ Links ]
11. Geeslin AG, Chahla J, Moatshe G, et al. Anterolateral knee extra-articular stabilizers: a robotic sectioning study of the anterolateral ligament and distal iliotibial band Kaplan fibers. Am J Sports Med. 2018;46(6):1352-61. https://doi.org/10.1177/0363546518759053. [ Links ]
12. Makhmalbaf H, Moradi A, Ganji S, Omidi-Kashani F. Accuracy of Lachman and anterior drawer tests for anterior cruciate ligament injuries. Arch Bone Jt Surg. 2013;1(2) 94-97. [ Links ]
13. Miura K, Ishibashi Y, Tsuda E, et al. Intraoperative comparison of knee laxity between anterior cruciate ligament-reconstructed knee and contralateral stable knee using navigation system. Arthroscopy. 2010;26(9):1203-11. https://doi.org/10.1016/j.arthro.2010.01.002. [ Links ]
14. Bull AMJ, Earnshaw PH, Smith A, et al. Intraoperative measurement of knee kinematics in reconstruction of the anterior cruciate ligament. J Bone Jt Surg Br. 2002;84(7):1075-81. https://doi.org/10.1302/0301-620x.84b7.13094. [ Links ]
15. Scholten RJPM, Opstelten W, Van Der Plas CG, et al. Accuracy of physical diagnostic tests for assessing ruptures of the anterior cruciate ligament: A meta-analysis. J Fam Pract. 2003;52(9):689-94. [ Links ]
16. Kittl C, El-Daou H, Athwal KK, et al. The role of the anterolateral structures and the ACL in controlling laxity of the intact and ACL-deficient knee. Am J Sports Med. 2016;44(2):345-54. https://doi.org/10.1177/0363546515614312. [ Links ]
Received: March 2021
Accepted: July 2021
Published: March 2022
* Corresponding author: Michael.held@uct.ac.za
Editor: Dr David North, Paarl Hospital, Western Cape, South Africa
Funding: No funding was received for this study.
Conflict of interest: The authors confirm there are no conflicts of interest, financial or otherwise, to declare with regard to this study.














