Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SA Orthopaedic Journal
versão On-line ISSN 2309-8309
versão impressa ISSN 1681-150X
SA orthop. j. vol.20 no.3 Centurion 2021
http://dx.doi.org/10.17159/2309-8309/2021/v20n3a5
TRAUMA AND GENERAL ORTHOPAEDICS
A computer tomography-based anthropomorphic study of forearm osteology: implications for prosthetic design
Henry S Preterms*; Nando Ferreira; Marilize C Burger
Division of Orthopaedic Surgery, Department of Surgical Sciences, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
ABSTRACT
BACKGROUND: The aim of this study was to accurately establish the variability in the anatomy of the radius and ulna in the context of the design of an intramedullary nail for both bones
METHODS: Forearm computed tomography scans were used to measure the specific internal and external anatomy of the radius and ulna in adult patients. Patients with fractures or dislocations involving either the radius and/or ulna were excluded
RESULTS: A total of 97 scans, comprising 84% male and 16% female patients, were included. The mean radius length was 238.43±18.38 mm (95% CI 234.60-241.74 mm). The mean curvature was an arc with a radius of 561.43±93.49 mm (95% CI 543.09-580.78 mm). The smallest measurement of the canal width was 5.17 mm (95% CI 4.87-5.47 mm). The ulna showed a mean length of 259.90±19.88 mm (95% CI 255.89-263.91 mm). The smallest measurement of the canal width was 4.80±1.30 mm (95% CI 4.53-5.87 mm). The mean proximal shaft angle was 11.39±3.30° (95% CI 10.76-12.82°
CONCLUSION: This computed tomography scan-based anthropomorphic study has identified novel anatomical features and associations of human forearm bones. This information will be used in the design and manufacture of anatomic intramedullary devices to better manage radius and ulna fractures or pathology
Level of evidence: Level 4
Keywords: radius, ulna, anatomy, osteology, radius of curvature, intramedullary design
Introduction
The radius and ulna are commonly fractured bones,1 but despite the frequency with which these bones are injured, studies that describe their anatomy are limited. The specifically relevant anatomy of the internal osteology makes the design of new implants challenging as few studies relate to the canal size or radius of curvature.24 In-depth anatomical studies can be used to design the shape and size of implants and will also take advantage of the anatomical relationships that relate implant size or length, which can be extrapolated by measuring specific areas of anatomy, for example, measuring the ulna to extrapolate the radial length.5-7 Due to the diverse injury patterns and numerous strategies of surgical management, a thorough understanding of the anatomy is of paramount importance. In support of this, studies by Beser et al. and others explored the anatomy of the ulna at the elbow joint and concluded that correctly measured angulations can help the design surgeon develop better prostheses and thereby maintain function of the elbow joint.8-12 This study, however, was limited to analysis of cadaveric specimens.
The challenge of anatomical studies is that the architecture of the bone often has to be destroyed in order to measure specific parameters.4 To circumvent this, Itamura et al.2 used computed tomography (CT) scans of the proximal radius of cadaveric specimens. The results demonstrated a clear shape mismatch of the native radial head and available radial head replacement prostheses which could lead to jamming at the radio-capitellar and proximal radioulnar joints.2 The paucity in the literature regarding radius and ulna anatomy is noted as well as previously reported studies with numbers less than 40,2,13 with the notable exception of Rouleau et al. who scanned only the proximal ulna (n=100).14
The morphology of the proximal and distal radius has been studied in great detail. Limited literature on the radius of curvature of the radius makes accurate reconstruction of this curvature when treating forearm fractures challenging.11 The clinical significance is that the union rates are improved for fractures where the anatomy has been restored.15,16 Apart from the radius of curvature of the radius that remains to be better defined, the relationship and relative length of the radius and ulna also need to be established.
The aim of this study was therefore to describe the anatomy of the radius and ulna of individuals that underwent forearm CT scans.
Methods
A retrospective anatomical study of the radius and ulna of patients that underwent forearm CT scan was conducted. Institutional ethics committee approval as well as institutional clearance was obtained prior to commencement of data collection. The hospital picture archiving and communication system (PACS) database was searched for all forearm scans that fitted the study criteria. Specifically, all patients older than 18 years, presenting between January 2014 and October 2015, who subsequently received a CT scan of their forearm were considered for inclusion. Any patients with fractures of the radius and/or ulna or any other anatomical deformities were excluded.
All CT scans were performed with a Siemens SOMATOM Emotion 6 with minimum slice thicknesses of 0.23 mm. The image files were stored as Digital Imaging and Communications in Medicine format (DICOM) files. All measurements were made using RadiAnt 4.2.1 (Medixant, Poland) DICOM viewing software.
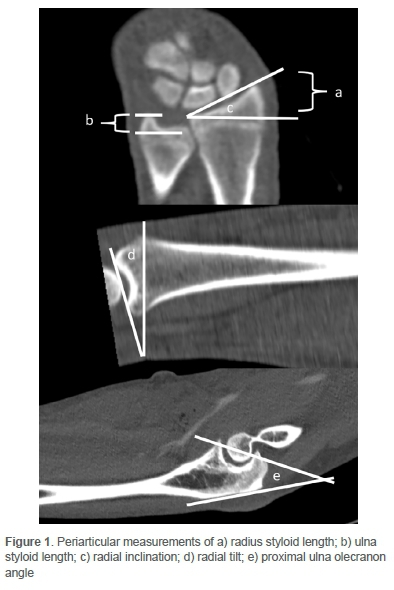
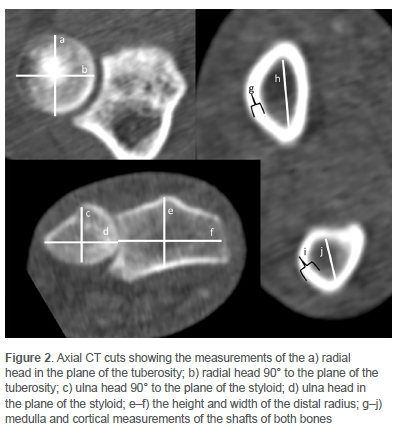
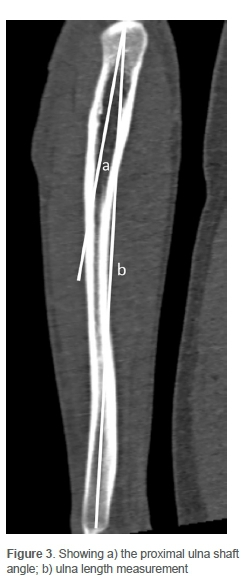
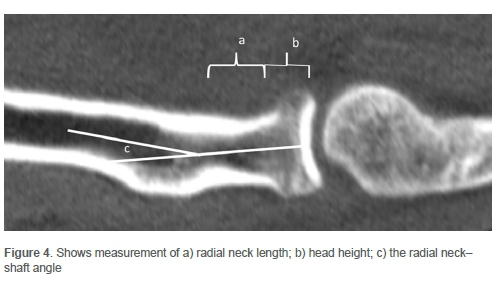
The collected images were processed using image processing software, and measurements were taken by a single investigator. To standardise the measurements, the images were visualised in a multiplanar reconstruction mode (MPR). Measurements of specific anatomical areas were taken to highlight the pertinent anatomy, and included (Figures 1-5):
The radius:
1. Overall length from the midpoint of the wrist to the centre of the radial head
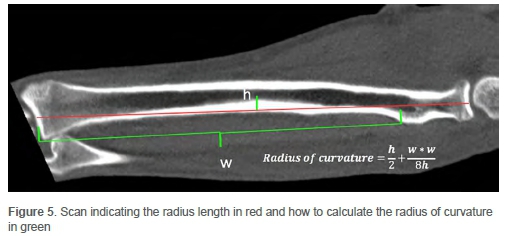
2. Radius of curvature of the shaft of the radius (length from the middle of the shaft proximally where the neck ends and the curved shaft begins, and the distance from the previous line to the apex of the arc)
The radius of curvature uses the arc height (h) and curve length (w) in the formula:
Radius of curvature 
3. Canal diameter in the middle of the bone and at the midpoints of the proximal and distal shafts
4. Cortical diameter of the radius at the neck, proximal, middle and distal shaft
5. Size of the radial head in height and diameter measured in relation to the radial tuberosity
6. Maximum angle between the radius neck and radius shaft
7. Radius tilt, inclination and styloid length of the distal radius
8. Distal radial height including Lister's tubercle, and width of the distal radius
The ulna:
1. Overall length from the midpoint of the olecranon to the centre of the distal ulna
2. Olecranon articular angle
3. Cortical thickness of the ulna at the proximal, middle and distal shaft
4. Canal diameter of the ulna at the proximal, middle and distal shaft
5. Size of the ulna head measured in the plane of the styloid and at 90° to the plane
6. Angle between the olecranon and ulna shaft
Data was analysed using STATISTICA (v13, TIBCO Software). Considering the anatomical nature of the measurements taken, all data was normally distributed as expected. Data is described as means ± standard deviations (SDs) with 95% confidence intervals (CI) indicated in parentheses. Categorical data is described as frequencies with the count indicated in parentheses.
Results
A total of 97 scans were included with an equal distribution between left (49%, n=47) and right (51%, n=49) forearms. The cohort consisted of predominantly male patients (84%, n=82) with a mean age of 34.91±13.33 years (95% CI 32.22-37.59).
The majority of scans (84%, n=81) were performed following trauma, which included 54 (56%) stab wounds, and 22 (23%) gunshot-related injuries. The non-traumatic indications (16%, n=16) scans were performed for vascular or other medical reasons (Figure 6).
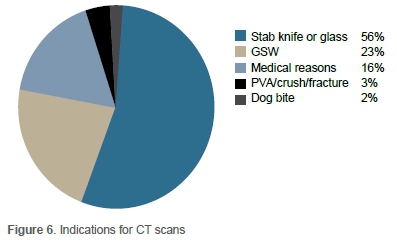
Table I shows the measurement results for the radius and ulna. The mean radius length was 238.43±18.38 mm (95% CI 234.60-241.74 mm), with the mean curvature being an arc with a radius of 561.43±93.49 mm (95% CI 543.09-580.78 mm) and the smallest measurement of the radial canal width being 5.17 mm (95% CI 4.87-5.47 mm). The study shows the radial styloid length of 10.55±2.13 mm (95% CI 10.12-10.98 mm) and the radial inclination 20.99±2.50° (95% CI 20.48-21.49°) as well as volar tilt 12.94±3.68° (95% CI 12.20-13.68°). The distal radius height including Lister's tubercle measured 23.06±2.80 mm (95% CI 22.49-23.62 mm).
The ulna showed a mean length of 259.90±19.88 mm (95% CI 255.89-263.91 mm) with the smallest measurement of the ulna canal width being 4.80±1.30 mm (95% CI 4.53-5.87 mm). The mean proximal shaft angle was 11.39±3.30° (95% CI 10.7612.82°).
Discussion
The aim of this study was to accurately establish the variability in the anatomy of the radius and ulna in the context of the design of intramedullary nails for both bones by assessing CT scans.
When considering the anatomy of the radius, the results are useful in the context of implant design. When the curvature of the radius is discussed, the coronal curve of the radius is not the same as the measurement referred to as the bow of the radius. The bow of the radius is measured as the distance from a longitudinal line connecting the cortex at the level of the radial tuberosity and the ulna border of the distal radius at the radioulnar joint to the radius cortex at its furthest point. As the medullary canal and cortical margin of the radius are not parallel, and the radius of curvature is related to the canal of the radius, it stands to reason that the measurements should be in the medullary cavity of the radius or parallel to that on the outer cortex. This is done using the centre of the canal at the start and end of the curve with the mathematical formula given above. The clinical relevance is that an intramedullary implant with a curvature that recreates the bow of the radius will lead to better union rates.15 Our findings confirm a mean radius of curvature for most forearms of 561.93 mm, with the 95% CI between 543.09 and 580.78 mm.
When considering nail length, we can be confident that an implant length ranging from 220 to 270 mm (radius 238.43±18.38, ulna 259.9±19.88) would represent the shortest radius and the longest ulna in our study population. Additionally, by using 10 mm increments, the nails will be appropriate for most individuals that might require treatment. With respect to canal size, an implant size of 4.5 mm would allow passage through the 5 mm canal observed in our cohort. The distal height of the radius and the proximal diameter of the ulna allows enough space for the 6 mm nail locking block.
The mean distal radius height was found to be 23.06 mm (SD 2.80, range 14.70-33.30) with the 95% CI being between 22 and 24 mm. This observed height can potentially be extrapolated to the length of screws one might need for distal locking plates, thus alleviating the need to manufacture screws far outside of the observed range. This limited range might potentially lead to a cost and inventory advantage for implant manufacturers.
The study confirms some features of previous studies on the Rule of 11 with the styloid length, volar inclination and radial inclination being 11 mm, 11° and 22° (2*11), where this is used for decision-making in distal radius fractures.17 The study shows the radial styloid length of 10.55±2.13 mm (95% CI 10.1210.98 mm) and the radial inclination 20.99±2.50° (95% CI 20.4821.49°), which are in keeping with previously held ideas. The volar tilt of 12.94±3.68° (95% CI 12.20-13.68°) is larger than previously described as 11° and this may have relevance to distal radius fracture management.
Although the sample size of 97 scans is limited, this sample is significantly larger than previously reported studies which included a cadaver study (n=12)13 and a similar CT study (n=22)2 with the notable exception of Rouleau et al. who scanned only the proximal ulna (n=100). Although most patients included in the current study were male, this is potentially the population group that would most require the use of a forearm intramedullary nail. Future studies could potentially repeat these investigations in female-dominated samples. Although our tertiary institution serves a mixed demographic of patients, it is still only including measurements from one geographical area surrounding our hospital; however, we do not anticipate that patient demographics within South Africa will play a large role in variation. There might, however, be variation in other population groups outside of South Africa, which should be the target of future investigations.
This study formed part of a larger study that aims to investigate statistical shape modelling for future predictive models. The present study was the first and investigated the anatomical features of the two most often fractured forearm bones.
Conclusion
This CT scan-based anthropomorphic study has identified novel anatomical features and associations of human forearm bones. This information will be used in the design and manufacture of anatomic intramedullary devices to better manage specific radius and ulna fractures or pathology.
Acknowledgements
Dr Nabeela Adam for the initial measuring and data capturing; Dr Rudolph Venter was integral in the study design for CT anatomical studies.
Ethics statement
The authors declare that this submission is in accordance with the principles laid down by the Responsible Research Publication Position Statements as developed at the 2nd World Conference on Research Integrity in Singapore, 2010. Prior to commencement of the study ethical approval was obtained from the following ethical review board: Stellenbosch University Health Research Ethics committee (S17/10/097). All procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Informed written consent was waived by the ethics committee for all patients included in the study.
Declaration
The authors declare authorship of this article and that they have followed sound scientific research practice. This research is original and does not transgress plagiarism policies.
Author contributions:
HSP: Study conceptualisation, data capture, data analysis, first draft preparation, manuscript revision and final draft preparation
NF: Data analysis, language and grammar correction and final draft review MB: Data analysis, language and grammar correction and final draft review
ORCID
Pretorius HS https://orcid.org/0000-0002-7419-0885
Ferreira N https://orcid.org/0000-0002-0567-3373
Burger MC https://orcid.org/0000-0003-2831-4960
References
1. Ilyas AM. Surgical approaches to the distal radius. Hand (N Y). 2011;6(1):8-17. [ Links ]
2. Itamura JM, Roidis NT, Chong AK, et al. Computed tomography study of radial head morphology. J Shoulder Elb Surg. 2008;17(2):347-54. [ Links ]
3. Malone PSC, Shaw OG, Lees VC. Anatomic relationships of the distal and proximal radioulnar joints articulating surface areas and of the radius and ulna bone volumes - implications for biomechanical studies of the distal and proximal radioulnar joints and forearm bones. Front Bioeng Biotechnol. 2016;4(July):1-7. https://doi.org/10.3389/fbioe.2016.00061. [ Links ]
4. Barrier ILO, L'Abbé EN. Sex determination from the radius and ulna in a modern South African sample. Forensic Sci Int. 2008;179(1):85.e1-7. [ Links ]
5. Köse A, Aydin A, Ezirmik N, et al. Alternative treatment of forearm double fractures: new design intramedullary nail. Arch Orthop Trauma Surg. 2014;134(1):1387-96. https://doi.org/10.1007/s00402-014-2058-9. [ Links ]
6. Alao U, Liew I, Yates J, Kerin C. Correlation between the length from the elbow to the distal interphalangeal joint of the little finger and the length of the intramedullary nail selected for femoral fracture fixation. Injury. 2018;49(11):2058-60. https://doi.org/10.1016/j.injury.2018.08.024. [ Links ]
7. Badkur P, Nath S. Use of regression analysis in reconstruction of maximum bone length and living stature from fragmentary measures of the ulna. Forensic Sci Int. 1990;45(1-2):15-25. [ Links ]
8. Beser CG, Demiryürek D, Özsoy H, et al. Redefining the proximal ulna anatomy. Surg Radiol Anat. 2014;36(10):1023-31. [ Links ]
9. Akpinar F, Aydinlioglu A, Tosun N, Tuncay Í. Morphologic evaluation of the ulna. Acta Orthop Scand. 2003;74(4):415-19. [ Links ]
10. Yong WJ, Tan J, Adikrishna A, et al. Morphometric analysis of the proximal ulna using three-dimensional computed tomography and computer-aided design: varus, dorsal, and torsion angulation. Surg Radiol Anat. 2014;36(8):763-68. [ Links ]
11. Pall Singh TS, Sadagatullah AN, Yusof AH. Morphology of distal radius curvatures: A CT-based study on the Malaysian Malay population. Singapore Med J. 2015;56(10):562-66. [ Links ]
12. Vroemen JC, Dobbe JGG, Jonges R, et al. Three-dimensional assessment of bilateral symmetry of the radius and ulna for planning corrective surgeries. J Hand Surg Am. 2012;37(5):982-88. https://doi.org/10.1016/j.jhsa.2011.12.035. [ Links ]
13. Lamas C, Llusà M, Méndez A, et al. Intraosseous vascularity of the distal radius: Anatomy and clinical implications in distal radius fractures. Hand. 2009;4(4):418-23. [ Links ]
14. Rouleau DM, Canet F, Chapleau J, et al. The influence of proximal ulnar morphology on elbow range of motion. J Shoulder Elb Surg. 2012;21(3):384-88. https://doi.org/10.1016/j.jse.2011.10.008. [ Links ]
15. Yörükoglu A çagdas, Demirkan AF, Akman A, et al. The effects of radial bowing and complications in intramedullary nail fixation of adult forearm fractures. Jt Dis Relat Surg. 2017;28(1):30-34. [ Links ]
16. Dave MB, Parmar KD, Sachde BA. The radial bow following square nailing in radius and ulna shaft fractures in adults and its relation to disability and function. Malaysian Orthop J. 2016;10(2):12-15. [ Links ]
17. Hanley EN. Instructional Course Lectures. J Bone Jt Surg. 2004;86(11):258 7-88. [ Links ]
Received: September 2020
Accepted: January 2021
Published: August 2021
* Corresponding author: hsp359@sun.ac.za
Editor: Prof. Sithombo Maqungo, University of Cape Town, Cape Town, South Africa
Funding: No funding was received for this study.
Conflict of interest: The authors declare they have no conflicts of interest that are directly or indirectly related to the research.














