Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SA Orthopaedic Journal
versión On-line ISSN 2309-8309
versión impresa ISSN 1681-150X
SA orthop. j. vol.20 no.1 Centurion feb./mar. 2021
http://dx.doi.org/10.17159/2309-8309/2021/v20n1a6
ORTHOPAEDIC ONCOLOGY AND INFECTIONS
Intra-operative extracorporeal radiation therapy for skeletally immature patients with malignant bone tumours
Manish R ShahI; Manisha Μ ShahII; Aditya Κ AgrawalI; Malkesh D ShahI; Sarvang Μ DesaiI
IDepartment of Orthopaedics, Dhiraj Hospital, Smt BK Shah Medical Institute and Research Centre, Sumandeep Vidyapeeth deemed to be University, Waghodia, Vadodara, Gujarat, India
IIDepartment of Pathology, Medical College and SSG Hospital, Vadodara, Gujarat, India
ABSTRACT
BACKGROUND: Management of malignant bone tumours has changed dramatically in recent years. Neoadjuvant chemotherapy, irradiation and conservative surgery have improved local control as well as functional outcome. Depending on the histology of the lesion, other modalities like chemotherapeutic agents or radiation can be selected in place of surgical intervention. Operative intervention is the main modality with wide marginal excision and fixation of bone graft from different sources or mega prosthesis to maintain congruity of the bone anatomy. Reconstruction, optimum fit and stability at the affected site are the major areas of concern with this modality. Radiation given outside the body to kill the tumour cells in the bone is called extracorporeal radiotherapy (ECRT). After resection of the bone, it is cleaned of all the surrounding soft tissue and marrow contents and placed in a container. It is then subjected to 50 Gy of radiation which kills all the tumour cells.
METHODS: The study was conducted from June 2014 to May 2020, and included 15 patients (out of 18) diagnosed with either Ewing's sarcoma or osteosarcoma. They were followed up for an average of 4.44 years, up to May 2020. All 15 cases were analysed for bony union at the osteotomy sites. Cases reported with poorly differentiated sarcomas (total three) were subjected to immunohistochemistry and managed with other modalities of treatment.
RESULTS: The average time for union of irradiated bone was 8.1 months (range 5-10; the metaphyseal end united faster than the diaphyseal end). At the final follow-up, the functional status was determined using the Musculoskeletal Tumour Society (MSTS) scoring system. Ninety-three per cent of patients had involvement of the lower limb (14 out of 15). All patients (except one who developed recurrence) did not have symptoms of the disease and no one had died at last follow-up.
CONCLUSION: Biological limb salvage procedures are considered a successful treatment and a welcome alternative for patients who either cannot afford or be treated with an endoprosthesis. Early diagnosis and referral to specialised unit is of vital importance. This procedure can be used for selected patients with malignant bone tumours. Cost factors, and social and cultural considerations also play a role
Level of evidence: Level 4.
Keywords: ECRT, extracorporeal radiation therapy, malignant bone tumours, bone sarcoma, osteosarcoma, Ewing's sarcoma
Introduction
Management of malignant bone tumours has changed dramatically in recent years. Neoadjuvant chemotherapy, irradiation and conservative surgery have improved local control as well as functional outcome. Depending on the histology of the lesion, other modalities like chemotherapeutic agents or radiation can be selected instead of surgical intervention. Operative intervention is the main modality, with wide marginal excision and fixation of bone graft from different sources or metallic modular implant for maintaining congruity of the bone anatomy. Reconstruction, optimum fit and stability at the affected site are the major areas of concern with this modality. This procedure is for a selected few cases done in a specialty unit after multidisciplinary discussion. Some units have found it necessary to augment this segment with a vascularised fibular graft as an inlay technique. Irrespective of method, fixation must be very stable.
In 1968, Spira and Lubin used extracorporeal irradiation therapy (ECRT) of the resected bone intra-operatively for the first time in treating malignant bone tumours.1 Irradiation provides the same individual's strut graft for fixation in the intercalary gap and reconstruction with correct dimensions. Such grafts are used in some cases of malignant bone tumours having less destructive (lytic) and more sclerotic changes.2 As per the literature, people have studied the use of the patient's own bone after sterilisation by different methods. Various processes of sterilisation include use of liquid nitrogen, microwave, autoclave, alcohol inactivation or ECRT. Prosthesis reconstruction and composite arthroplasty have the most favourable results, such as better function and fewer adverse effects.3 However, the metallic modular implant has drawbacks in terms of durability, financial issues and being restricted in use to patients who have achieved skeletal maturity (or we need to consider expandable prostheses with high cost).4 In the paediatric age group, the issue of small canal diameter is another disadvantage.
In developing countries, due to the financial burden, primary bone tumour patients have another option, namely excision of part of the limb proximal to the lesion (amputation). However, this is not acceptable to patient or family when other options are available. Surgeries which preserve the patient's own bone are therefore an attractive option. Young growing children present extra challenges due to the fact that they have open physes and still need to grow substantially, making their reconstruction even more challenging. The option for reconstruction is custom endoprosthesis (growing implants for children) but it is very expensive in the developing world setting. Allograft, autograft (vascularised and non-vascularised), extracorporeal radiated bone, distraction osteogenesis, a combination of the above, and rotationplasty (some centres still offer this procedure) are other options.
Radiation given outside the body to make the bone free of tumour is called extracorporeal radiotherapy (ECRT). After resection of the bone, it is cleaned of all the surrounding soft tissue and intramedullary contents and placed in a container. It is then subjected to 50 Gy of radiation which kills all the tumour cells. The free radicals released during the radiation not only kill the tumour cells within the bone but also in the surrounding soft tissue. This renders the bone specimen tumour free; it is then brought back to the operating theatre and re-implanted by stabilising it with appropriate fixation devices. Ideally radiation therapy in tumours requires 2 Gy radiation (in vivo) per sitting, either daily or on alternate days for a minimum of 25 sittings. Therefore, intra-operative ECRT provides, in one sitting, the equivalent of over a month of radiation therapy of 50-60 Gy of radiation. This reduces the economic and financial burden on the patient. It also reduces the exposure to radiation in multiple sittings; the physical endurance in such treatment is thereby reduced and it becomes more acceptable to the patient. The advantages of re-fixation with the same bone is that you get an exact match to the resected bone which is tumour-free. Post-operatively the joint is mobilised early, and weight bearing can be started according to the union of re-implanted bone. Post-operative radiotherapy is avoided. The end facing towards diaphysis takes more time to unite than the metaphyseal end. There is comparatively less chance of recurrence and fewer chances of any limb length discrepancy (in comparison to limb salvage surgeries by non-expandable prostheses).
If the tumour has caused extensive destruction of bone, pathological fracture or it is a metastatic tumour, it is not sound to reimplant it after ECRT; therefore, this method cannot be advised for such patients. Irradiation given outside the body is a safe and physically stable construct procedure in reconstructing bony defects after tumour resection in skeletally immature patients.
The aim of our study is to know functional results, survival rate and union status after the procedure.
Materials and methods
The study was conducted between June 2014 and May 2020, and included 15 patients (out of 18) diagnosed with either Ewing's sarcoma or osteosarcoma (non-metastatic stage T1N0M0). Cases reported with poorly differentiated sarcomas (total ) were subjected to immunohistochemistry (IHC) and managed with other modalities of treatment. Institutional Review Board approval was obtained. All patients were informed about the procedure and informed consent was taken for each case. Follow-up was done up to May 2020 and those who were on regular follow-up were included in the study. Patients with open physis and non-metastatic tumour were included in the study; patients diagnosed with chondrosarcoma (uncommon in young age, and not radiation-sensitive, with radiation reserved for non-operable cases) and older than 18 years were excluded from the study.
All patients were given neoadjuvant chemotherapy (NACT) as per the advice of the oncologist. All investigations such as blood reports, X-rays, MRI and positron emission tomography (PET) CT scan were done as per standard protocol. The patients eligible for the study underwent wide marginal excision followed by reimplantation of the same part after it had been given radiation outside the body (Table I). We did not use vascularised or non-vascularised fibula graft in any of the cases as the dimensions of the irradiated bone were perfectly matched host bone and the whole construct was stable after fixation.
On follow-up, for an average of 4.44 years up to May 2020, the complete medical records, radiological imaging, and status of the patient at the last follow-up including functions were recorded. Fourteen males and one female with age ranging from 7.5 years to 16 years with average of 9.6 years were studied. Proximal tibia was the commonest (11 of 15). Distal femur (three of 15) and humerus (one out of 15) were also involved. Mean complaints duration (time from initiation of pain or swelling to first reporting at the hospital) was 20 weeks (18 to 52 weeks). A pre-operative MRI and histological diagnosis (by Tru-cut bone biopsy needle) were obtained from all the patients in the study. Patients in whom diagnosis was made elsewhere were included in the study (n=3). In the remaining patients (n=12), core needle biopsy was performed to confirm the diagnosis. A multispecialty approach (tumour board) was used, including a radiologist, pathologist and an oncologist to assess the patients and determine the treatment protocol based on the extent of the disease. A thorough examination of the patient was mandated to rule out metastasis at the time of presentation by primary screening of the chest (multidetector computed tomography), abdomen ultrasound and PET CT scan.
None of the patients included in the study had any metastases on first consultation. As per the oncologist's decision, pre- and postoperative chemotherapeutic agents were given.
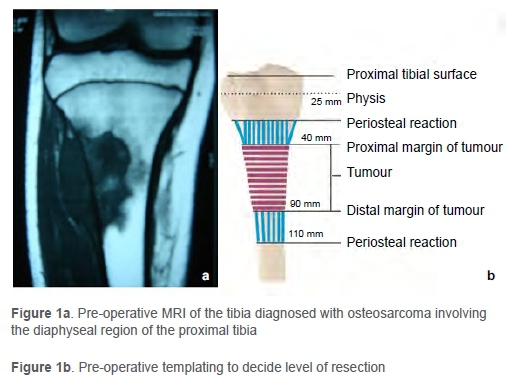
The extent of the lesion and neurovascular involvement were studied by CT angiography and MRI. Wide margin resection was performed with a 2.5-3 cm free margin as per the pre-operative plan based on the MRI (Figure 1).
Intra-operative frozen section was done from the proximal and distal canals to check for malignant cells. The resected bone specimen was cleared off the surrounding soft tissue and periosteum. It was then subjected to ECRT intra-operatively maintaining aseptic precautions. For irradiation, the resected bone was placed in a mop soaked with saline, povidone-iodine and vancomycin, and wrapped with sterile plastic drape in two layers.
It was put in a surgical drum after being wrapped in two surgical towels and was then sent to the radiation unit (Figure 2).
The specimen was subjected to a tumoricidal dose of 50 Gy, creating a dead autologous bone graft (Figures 3a and b). Time taken to transfer the bone out of theatre followed by the ECRT process, and receiving the graft ranged from 40 to 60 minutes (average 45 minutes). The irradiated bone was then prepared for re-implantation by reaming the marrow of its contents and subjecting it to a thorough lavage to remove any residual marrow tissue. The resected tissue was then placed back after ECRT at the operative site (Figure 4), and fixation was done with anatomical plates (Figure 5).

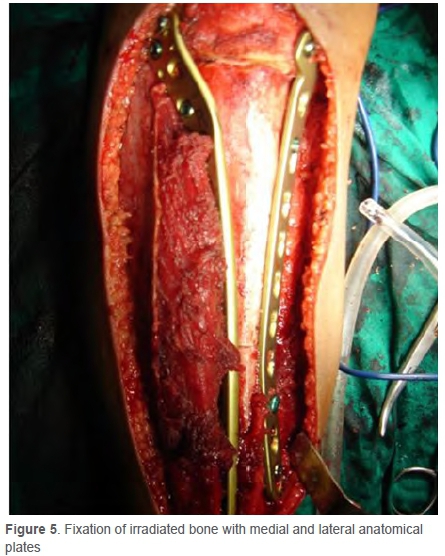
In the younger age group, fixation was done with one locking compression plate and one K-wire. In older children two plates were used.
In lower limb involvement, the patient was advised to immobilise with a long knee brace for four weeks postoperatively followed by gradual mobilisation of knee, and nonweight bearing walking after three months. For upper limb cases, a pouch arm sling was given for immobilisation.
Patients were followed up regularly every month. Apart from local examination for recurrence, X-rays (AP and lateral views) were taken during follow-ups. The osteotomy site was ur examined for union in AP and lateral views by assessing two cortices in each view. A total of three out of four cortices in continuity are required to confirm union at the osteotomy site. Patients are advised against weight bearing walking until osteotomy union has been established. A mean follow-up of 4.44 years (ranging from 1.8 to 5.6 years) for all patients was 3 recorded. During their final visit, the status was decided by the Musculoskeletal Tumor Society scoring method (MSTS score).5 There was no limb length discrepancy on follow-up in any of the patients.
Post-operative chemotherapy (adjuvant chemotherapy) was given as per the oncologist's decision.
Results
The frozen sections taken intra-operatively provided the basis for a tumour-free margin and definitive histopathological diagnosis. One patient (case 1) had post-operative deep infection at the operative site with exposed bone and implant. Two patients (13%) developed superficial infection (cases 4 and 8).
The major concern against ECRT autograft is ruling out malignancy by microscopic examination and to re-confirm the resected specimen. Examination of the gross specimen is not possible. On the patient's follow-up (case 1) in the fifth month, there was evidence of dehiscence over the proximal suture line with an exposed implant (Figure 6).

In the patient with deep infection, the complication resulted in an advantage. The exposed lateral plate was removed as the osteotomy site union had already occurred. Biopsy was taken from the previous tumour site, which revealed no evidence of tumour with marrow tissue necrosis and fibrohyalinisation. The patient did not have any other complications in the subsequent follow-ups. The patient was followed up after three months and advised to fully weight bear as the X-rays suggested complete union (Figure 7). The patients with superficial infection (cases 4 and 8) were treated with debridement and primary closure. One patient (case 15) developed recurrence at the local site without any metastasis (confirmed by PET scan) on follow-up at 2.5 years. He was advised to have an above-knee amputation.



All 15 cases were analysed for bony union (assessed by union in three out of four cortices in AP and lateral views) of the graft. Mean time ranged from Ave to ten months with a mean of 8.1 months. The metaphyseal end united faster (7.3 months) than the diaphyseal end (8.9 months).
At the last visit, functions were determined using the MSTS score. Scoring was done considering pain, activities of daily living and psychological acceptance apart from specific factors per limb. For the upper limb, position of hand, manual skill and lifting ability were tested; for the lower limb, need of support for mobilisation, ability to walk, and gait pattern were examined. Scores of 0 to 5 were given for each factor (a total of seven) as per criteria; the score was therefore given out of a maximum of 35. The time for the last follow-up varied from 1.8 to 5.6 years with a mean of 4.44 years. We found an average MSTS score of 19 to 26 (mean 22.8). Fourteen of the 15 patients had lower limb involvement, while one patient had upper limb involvement. At the time of the final follow-up, all except one were disease-free with no mortality recorded. One patient was treated with above-knee amputation due to recurrence diagnosed at 2.5 years of follow-up. All survived for more than four years from the index surgery.
Discussion
Zhang et al. studied early and late complications in reimplanted involved bone of limb malignancies post-ECRT and en bloc resection. In the retrospective study, fracture, infection, non-union and graft resorption were found in 11 patients out of 39. Functions and longevity rates were better in spite of high re-surgery (39.1%) and complications (47.8%).6 Other studies have also shown treatment by ECRT.7
Ewing's sarcoma (33%) and osteosarcoma (67%) were commonly found in our study, consistent with known numbers found in other studies.8 Here we have studied the treatment protocol followed for osteosarcoma and Ewing's sarcoma.
Before surgery each patient was fully investigated, and biopsy and staging were done. Surgery was planned after consultation with other relevant disciplines and tumour board members. All patients with Ewing's sarcoma and osteosarcoma were subjected to pre-operative (neoadjuvant) chemotherapeutic agents. Postoperative (adjuvant) chemotherapy decisions were taken as per the oncologist's opinion.
Advantages of this method are that the resected tumour undergoes ECRT (in vitro) immediately and the tissue is placed at the operative site thereafter. The autogenous tissue is placed back without subjecting the whole body to radiation and hence the amount of radiation the tumour tissue is exposed to is much higher, keeping in mind that there are no adverse effects to any normal tissue. There is no use of cement or graft to maintain the congruity of the bone. This is advantageous to the patient as there is no need for bone grafting with its associated complications.
It is relatively economical and compliance with treatment is also better. This limb-salvaging procedure also prevented the need for prosthesis in a 16-year-old child. Advantages of this method include less or no risk of disease transmission or immunological reaction, availability of bone, no question of preservation of bone and biological reconstruction.
Poffyn et al. showed that patients with osteosarcoma and Ewing's sarcoma resection showed excellent response to en bloc resection with ECRT of the resected tumour.7 The study was conducted retrospectively from 1978 to 2009, and studied 107 patients with locally aggressive malignant bone tumours. In their study after resection and ECRT, orthotopic autografts were re-implanted. Normal fracture healing times in irradiated grafts do not show accurate results. Follow-up at two years showed healing in 62% (31 out of 50) and 64% at Ave years (27 out of 42). Non-union was found in the remaining 15 of the orthotopic grafts.8
A similar study was done by Puri et al. on non-metastatic diaphyseal sarcomas which were treated by wide marginal excision followed by ECRT (50 Gy) and reconstruction of the same irradiated sterilised bone tumour.9 They studied a total of 32 patients (16 osteosarcoma plus 16 Ewing's sarcoma). Thirty-one patients were followed up for between 12 and 74 months, and showed a mean union time of 7.3 months (3 to 28). At the final follow-up no disease was found in 19; 11 patients demised due to disease; and one patient had disease.
Puri et al.'s evaluation by mean functional MSTS score was found to be 87%. By comparison, our study found it to be 65%. Puri et al. found it to be higher when compared with other methods using irradiated graft.9
Nakamura et al. reported a study of six patients with Ewing's sarcoma of the mid-shaft femur treated by limb-sparing resection and reconstruction with cement augmentation with good results.10 We do not have such experience and did not feel the need to use cement in any of our cases.
The limitations of our study include its small sample size. Follow-ups ranged from 1.8 to 5.6 years with an average of 4.44 years, which can be considered reasonable. The only disadvantage which can be mentioned is the non-availability of full specimens for deciding tumour necrosis by chemotherapy by this modality of treatment. As this procedure is relatively uncommon, suitable for a particular group of patients and being a pilot study, it is a useful guide.
Conclusion
ECRT is a technique that is one of the treatment options of bone tumours in skeletally immature patients. ECRT is a relatively less expensive, versatile option for saving the limb in bone malignancies provided good bone stock is available. However, early diagnosis and referral to a specialised unit is of vital importance. This procedure can be used for selected patients with malignant bone tumours. Cost factors, and social and cultural considerations also play a role. Even if it results in longer surgical time, it is economical and lowers the financial burden compared to other treatment modalities. It is relatively safe, provides good functional results with preservation of the nearby joint. Suitable implant and irradiated orthotopic host bone for internal fixation helps in achieving desired outcomes in patients with non-metastatic local bone tumours.
Ethics statement
The authors declare that this submission is in accordance with the principles laid down by the Responsible Research Publication Position Statements as developed at the 2nd World Conference on Research Integrity in Singapore, 2010. Institutional Review Board (IRB) ethical approval was obtained: approval no. 3/2014/
SH. Prior to commencement of the study ethical approval was obtained from the following ethical review board: SH (HRRP)-3/2014.
All procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Informed written consent was obtained from all patients for being included in the study.
Declaration
The authors declare authorship of this article and that they have followed sound scientific research practice. This research is original and does not transgress plagiarism policies.
Author contributions
MRS: Study conceptualisation, data capture, data analysis, first draft preparation, manuscript revision
MMS: Study design, design of testing set-up, manuscript preparation
AKA: Data analysis, first draft preparation
MDS: Data capture
SMD: Design of testing set-up
References
1. Spira E, Lubin E. Extracorporeal irradiation of bone tumors. A preliminary report. Isr J Med Sci. 1968 Sep-Oct;4(5):1015-19. PMID: 5251288. [ Links ]
2. Böhm P, Fritz J, Thiede S, Budach W. Reimplantation of extracorporeal irradiated bone segments in musculoskeletal tumor surgery: clinical experience in eight patients and review of the literature. Langenbecks Arch Surg. 2003 Jan;387(9-10):355-65. [ Links ]
3. Gilbert NF, Yasko AW, Oates SD, et al. Allograft-prosthetic composite reconstruction of the proximal part of the tibia. An analysis of the early results. J Bone Joint Surg Am. 2009 July;91(7):1646-56. [ Links ]
4. Hardes J, Henrichs MP, Gosheger G, et al. Endoprosthetic replacement after extra-articular resection of bone and soft-tissue tumours around the knee. Bone Joint J. 2013;95B:1425-31. [ Links ]
5. Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993:241-46. [ Links ]
6. Zhang S, Wang X-Q, Wang J-J, Xu M-T. En bloc resection, intraoperative extracorporeal irradiation and re-implantation of involved bone for the treatment of limb malignancies. Mol Clin Oncol. 2017 Dec;7(6):1045-52. [ Links ]
7. Poffyn B, Sys G, Mulliez A, et al. Extracorporeally irradiated autografts for the treatment of bone tumours: tips and tricks. International Orthopaedics (SICOT) 2011;35:889-95. [ Links ]
8. Unni KK. Dahlin's bone tumors: general aspects and data on 11,087 cases. 5th ed. Philadelphia: Lippincott-Raven; 1996. p. 143-83. [ Links ]
9. Puri A, Gulia A, Jambhekar N, Laskar S. The outcome of the treatment of diaphyseal primary bone sarcoma by resection, irradiation and reimplantation of the host bone. J Bone Joint Surg Br. 2012;94-B:982-88. [ Links ]
10. Nakamura T, Abudu A, Grimer RJ, et al. The clinical outcomes of extracorporeal irradiated and re-implanted cemented autologous bone graft of femoral diaphysis after tumour resection. International Orthopaedics, 2012 Dec;37(4):647-51. [ Links ]
 Correspondence:
Correspondence:
Manish R Shah
manishshah2001in@yahoo.co.in
Received: June 2020
Accepted: October 2020
Published: March 2021
Editor: Prof. Theo le Roux, University of Pretoria, Pretoria, South Africa
Funding: No funding was received for this study.
Conflict of interest: The authors declare they have no conflicts of interest that are directly or indirectly related to the research.














