Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SA Orthopaedic Journal
versión On-line ISSN 2309-8309
versión impresa ISSN 1681-150X
SA orthop. j. vol.19 no.3 Centurion ago./sep. 2020
http://dx.doi.org/10.17159/2309-8309/2020/v19n3a6
ARTHROPLASTY
The short-term outcome of hip revision arthroplasty with Trabecular Metal™ components and augments
Noconjo LI; Nortje MBII
IB Physio; MBChB(UKZN); Registrar, Department of Orthopaedic Surgery, University of Cape Town, Groote Schuur Hospital, Cape Town, South Africa
IIMBChB(UCT), FC Orth(SA); MMed(UCT), Consultant Orthopaedic and Arthroplasty Surgeon, Department of Orthopaedic Surgery, University of Cape Town, Vincent Pallotti and Kingsbury Hospitals, Cape Town, South Africa
ABSTRACT
BACKGROUND: Highly porous Trabecular Metal™ acetabular components are increasingly being used in revision hip arthroplasty as they facilitate ingrowth, provide a useful mechanism to deal with bone loss and may decrease the risk of infection. The purpose of this audit was to describe: 1) the total number of hip arthroplasty surgeries over Ave years, the ratio of revision to primary hip arthroplasty and indications for revision; 2) the short-term outcomes of revision hip arthroplasty with Trabecular Metal™ components and augments
METHODS: A retrospective folder and radiograph review of all patients who had revision total hip arthroplasty (THA) at a tertiary level hospital from February 2012 to February 2017 was done
RESULTS: There were 979 THAs performed over the period - 863 (87%) primary THAs, and 116 (12%) hip revision cases performed in 107 patients. Of the 116 (107 patients) hip revisions, there were seven (6%) re-revisions in Ave patients. The indications for revision were aseptic loosening 67 (59%), septic loosening 11 (10%), liner wear 18 (16%), periprosthetic fracture Ave (4%), other 15 (13%). Trabecular Metal™ was used for revision in 16 hips (14 patients), which is 14% of the total 116 revisions. There were ten females and four males with an average age of 61 years. The average duration of follow-up in this group was 18.5 months (1.5-39.2). In these 16 Trabecular Metal™ hips, there were three (19%) early failures of fixation due to technical errors
CONCLUSION: In our institution, 12% of the arthroplasty is revision surgery. The indications for revision are similar to published literature. Trabecular Metal™ revisions had a 19% early failure rate due to technical error
Level of evidence: Level 4
Keywords: Trabecular Metal™, augments, total hip arthroplasty, revision hip arthroplasty
Introduction
Total hip arthroplasty (THA) is reported as one of the most successful procedures to relieve pain and restore function. It has evolved from a salvage procedure with poor long-term outcomes reserved for the most infirm patients, to one of the most successful and frequently undertaken elective surgical procedures.1
Indications for revision in a Swedish registry were aseptic loosening 75%, deep joint infection 8%, dislocation 6%, fracture 5%, technical errors 3% and implant fracture 1%.2 Aseptic loosening is a leading cause of failure in the intermediate and long-term post-operative period. It is hypothesised to be the result of a harmful combination of mechanical and biological events destroying the bond between the implant and the bone bed. To date, a variety of host, implant and surgery-related factors have been delineated to explain the development of aseptic loosening and osteolysis.3
Periprosthetic joint infection (PJI) is a devastating and costly complication of total joint arthroplasty. Diagnosis is challenging and a mixture of multiple tests can reasonably increase the diagnostic accuracy. Some criteria from the Musculoskeletal Infection Society (MSIS), European Bone and Joint Infection Society (EBJIS), and Infection Disease Society of America (IDSA) have been published.4 In our institution we prefer to use the MSIS criteria.
Dislocation is a complication occurring in approximately 0.3% to 10% of all primary procedures and up to 28% in revision surgery. It is a multifactorial problem caused by patient, implant and surgeon factors and can be reduced by thoughtful pre-operative planning and a careful surgical technique.5
Periprosthetic fractures in hip arthroplasty can occur intra- or post-operatively. Intra-operative fractures are estimated to occur in 1% of cemented and in 5.4% of uncemented primary THA. In revision surgery, incidence is higher, reaching 3.6% in cemented and 20.9% during uncemented procedures. Post-operatively, the incidence has been estimated to be less than 1% after THA and up to 4% following revision THA.6
Technical errors are of greater concern. Poor exposure, under-sizing, malposition, intra-operative fractures and failure to achieve correct soft tissue tension can cause any implant to fail despite optimal design characteristics. Lastly, implant fracture after THA is a relevant complication leading to technically demanding revision surgery, with an incidence of 304 fractures per 100 000 implants from a pooled worldwide arthroplasty registry dataset.7
Osteolysis can lead to problematic bone loss. Several classifications exist for acetabular bone loss in THA. The most commonly cited classification is that by Paprosky.8
The porous metal tantalum (Trabecular Metal™ Zimmer/Implex, Warsaw, IN) has been in use since 1997. A rough surface micro-texture provides a high coefficient of friction for increased initial stability. It has a lower modulus of elasticity than that of titanium which creates a potential for improved transfer of forces to the pelvis and reduced stress shielding. Interestingly, equivalent or lower bacterial adherence to porous tantalum has been demonstrated when compared with traditional surfaces.9 In our study all Trabecular Metal™ (or TM) cups were TM revision cups and if augments were used with the TM cup, they were Zimmer Biomet Trabecular Metal™ augments.
The purpose of this audit was to describe:
1. The total number of hip arthroplasty surgeries over five years, the ratio of revision to primary hip arthroplasty and the indications for revision.
2. The short-term outcome of revision hip arthroplasty with Trabecular Metal™ components and augments.
Materials and methods
After receiving approval from the institutional ethics board, we performed a retrospective audit on the use of TM acetabular components and augments in revision hip arthroplasty at Groote Schuur Hospital from February 2012 to February 2017. Eligible patients were identified from a prospectively collected orthopaedic surgery database. Clinical data including patient demographics, date of surgery, type of implant, indication for revision, complications and surgeon were recorded from patient folders. The pictorial archive communicating system (PACS) was used to access digital radiographic images. Pre-operative pelvic anteroposterior and lateral X-rays were reviewed, and defects classified as per Paprosky.8
Initial post-operative and last follow-up X-rays were evaluated for signs of osseous integration using the method of Moore et al.10All radiographs were reviewed by the investigator (registrar) and supervisor (senior consultant); a CT scan was not routinely performed. Patients with incomplete clinical and radiographic information, internal fixation revision to THA and revision for tumours were excluded from the study. Descriptive statistical analysis was used to analyse the data.
Results
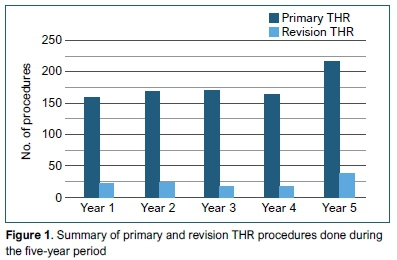
There were 979 THAs performed over the period: 863 (87%) primary THAs, and 116 (12%) hip revision cases performed in 107 patients. Figure 1 shows a breakdown of primary and revision THA procedures done per year. In the revision group there were 43 (40%) males and 64 (60%) females with an average age of 60.8 years (range 50-71). The average follow-up of the revisions was 15.9 months (4.7-25.8)
The indications for revision were aseptic loosening 67 (59%), septic loosening 11 (10%), liner wear 18 (16%), periprosthetic fracture five (4%), cortical perforation four (3%), recurrent dislocation four (3%), early failure of fixation four (3%), broken stem two (2%) and ankylosis one (1%).
The Paprosky classification of the revision cases is shown in Table I.

Of the 116 (107 patients) hip revisions, there were seven (6%) re-revisions. One of these seven re-revisions have not yet been performed due to medical reasons; the patient remains dislocated but is included in the numbers as a revision is indicated. The indications for re-revision and procedure summary for the remaining six re-revisions in five patients are shown in Table II. There were three females and two males, with an average age of 60.2 years (47-71).
Trabecular Metal™ was used for revision in 16 hips (14 patients), which is 14% of the total 116 revisions. There were ten females and four males, with an average age of 61 years (38-86). The average duration of follow-up in this TM group was 18.5 months (1.8-39.2). Three hips (19%) that were revised with TM failed to remain stable and were classified as early failure of fixation. Patient number 2 in Table II was revised with a cup and augment for a Paprosky 3A defect and had an excision arthroplasty when it failed. Patient number 5 in Table II was revised with a TM cup and screws which failed and was re-revised with a cup and augment, which failed and then re-revised with a cup cage construct. This accounts for the 16 hips and 14 patients in the TM group during the five-year study period.
For the purposes of the study, excision arthroplasty and implantation of an antibiotic-impregnated cement spacer followed by reimplantation of components in the same joint were considered as a single two-stage revision procedure.
Discussion
Total hip replacement is one of the most cost-effective procedures to relieve pain and improve function.1 The annual reports of the national arthroplasty registry of Sweden, Norway, Finland, Denmark, Australia and New Zealand show a mean of 1.29 revisions per 100 observed component years. This corresponds to a revision rate of 6.45% after five years and 12.9% after ten years.11 In our study 12% of the procedures were revisions, not necessarily from our unit as we are a tertiary referral centre.
We found similar indications for revision to the published literature. Aseptic loosening was the most common cause of revision surgery in our study. Ulrich et al. evaluated the indications for revision hip arthroplasty and showed that 51% were revised for aseptic loosening.12 It is probably a combination of several events and there is growing evidence indicating that cyclic mechanical loading, production of prosthetic wear particles and ensuing adverse tissue response are important contributors to local osteolysis and bone resorption at the bone-prosthesis interface.13
In our study, liner wear was the second most common indication for revision. There are three fundamental mechanisms of wear: abrasive, adhesive and fatigue. Abrasive wear constitutes the main wear type in hip arthroplasty. The criteria for revision surgery due to a worn polyethylene hip cup or liner have long been controversial. Often there is a dilemma in choosing polyethylene exchange alone or revising the acetabular components. Grobbelaar et al. reported a correlation between cup wear on the one hand, and pain, interface widening and osteolytic failure on the other.14 In our institution, if a cup is radiologically aligned and well fixed, we prefer to do polyethylene exchange alone.
Periprosthetic joint infection is a devastating complication for both patient and surgeon. Sepsis was the cause of 10% of our revisions. This figure is higher than that reported by Ulrich et al.,12 probably because our institution is a tertiary referral centre. We did not analyse reasons for infection.
A periprosthetic fracture of the femur in association with THA is increasingly common and often difficult to treat. Similar to our study, Marsland et al. reported an overall incidence of 4% of periprosthetic femur fractures with higher rates for uncemented and revision THA.15
We started using Trabecular Metal™ after promising findings in a retrospective study of 966 patients (421 men, 545 women and 990 hips) on the use of tantalum (Ta) acetabular components in revision of THA. Tokarski et al. believe that the reason tantalum is more protective against infection is the higher potential of tantalum for osteointegration, thereby obliterating any dead space.16 The ability of osteoblasts to proliferate and integrate onto the surface of the uncemented component may then deprive infecting organisms' access to the surface. The second reason may relate to the topographical three-dimensional structure of the surface of tantalum that may be difficult for organisms to access and colonise. Furthermore, tantalum as an element may carry specific charge or have surface characteristics that are hostile to infecting organisms. Finally, they showed encouraging findings in the use of tantalum components which may be protective against failure due to infection at least in patients who had undergone revision surgery for infection. A case series by Malkani et al. showed that all 21 patients developed ingrowth along the tantalum surface despite compromised bone loss, and he concluded that porous tantalum appears to be a promising material to use in revision hip arthroplasty to facilitate biological ingrowth in patients with acetabular bone loss.17
In most cases of acetabular component revision, there will be some degree of bone loss.18 Our usual management of Paprosky type 3A and 3B includes the use of augments. Our approach is similar to that described by Abolghasemian et al. which suggests that type 1 and type 2 defects do not usually require the use of acetabular augments. In type 1, conventional cemented or cementless components can be used. Type 2 defects are usually managed with morselised bone graft and normal uncemented acetabular cups. If there is less than 50% contact of the cup with viable host bone, the use of an ultra-porous acetabular component is recommended to ensure sufficient initial stability and potential for subsequent bone ingrowth. Type 3 defects are mostly associated with the use of augments.19 Porous acetabular components are manufactured by numerous implant companies; we have used different manufacturers in our series but are focusing on the tantalum TM Revision™ components from Zimmer Biomet.
In Table II, patient 1 had failure of an uncemented 62 mm spiked cup in a 3B defect and was revised successfully to a 64 mm multi-hole uncemented cup with screws. In the first case, augments were incorrectly not ordered, probably causing the early failure of fixation and in the second, the cup screw construct was deemed stable and therefore augments not used.
Patient 2 was revised to a Trabecular Metal™ cup and augment and the augment grew in, but the cup failed due to cement extravasation during liner insertion that prevented osseous integration, evident at excision arthroplasty a year later. The patient had comorbidities precluding further major surgery.
Patient 5 had posterior superior acetabular bone loss which occurred with acetabular preparation at the first revision (Figure 2a). No augments had been ordered and the cup screw fixation failed in 3 months (Figure 2b). The second revision included an augment (Figure 2c) and the cup failed a year later (Figure 2d). This was converted to a cup cage construct (Figure 2e) and at revision the cup and augment were found to have no osseous integration. There was no sign of infection at any stage and the reason for early failure of fixation was thought to be instability of the construct. This patient continues to be monitored and there is no sign of loosening of the cup cage construct at final follow-up. The series of X-rays is shown in Figure 2.
Our study is limited by short follow-up. This is due to only recently starting to use Trabecular Metal™ and the fact that patients are lost to follow-up due to social factors and geographic movement. This audit needs to be repeated with longer follow-up. Our small numbers make statistical analysis difficult.
Conclusion
In our institution, 12% of the arthroplasty performed is revision surgery. The indications for revision are similar to the published literature. Trabecular Metal™ was used in 13% of revisions. Three hips (19%) failed to remain stable and were classified as early failure of fixation due to technical error.
Acknowledgement
I would like to acknowledge the assistance of Mr Archibald Mutsambiwa for information technology contributions.
Ethics statement
This submission is in accordance with the principles laid down by the responsible research publication position statements as developed at the 2nd World Conference on Research Integrity in Singapore. For this study, formal consent was not required and approval was given by our institutional Human Research Ethics Committee (HREC REF:149/2017).
Declaration
The authors declare authorship of this article and that they have followed sound scientific research practice. This research is original and does not transgress plagiarism policies.
Author contributions
LN: Primary author, responsible for study design, data collection, data analysis and manuscript preparation
MN: Conceptualisation, study design, manuscript preparation, supervision of the study
ORCID
Noconjo L https://orcid.org/0000-0001-9411-9392
Nortje MB https://orcid.org/0000-0002-7737-409X
References
1. Pivec R, Johnson AJ, Mears SC, et al. Hip arthroplasty. Lancet. 2012;380(9855):1768-77. https://doi.org/10.1016/S0140-6736(12)60607-2. [ Links ]
2. Kartz IN, Wright J, Wright EA, et al. Failures of total hip arthroplasty: a population-based perspective. Orthop J Harvard Med Sch. 2007;9:101-106. [ Links ]
3. Gallo J, Konttinen YT, Goodman SB, et al. Aseptic loosening of total hip arthroplasty as a result of local failure of tissue homeostasis. In: Fokter S, editor. Recent advances in arthroplasty. InTech; 2012. Available from: http://www.intechopen.com/books/recent-advances-in-arthroplasty/aseptic-loosening-of-totalhip-arthroplasty-as-a-result-of-local-failure-of-tissue-homeostasis. [ Links ]
4. Goel R, Tarabich M, Azboy I, et al. Management of periprosthetic joint infection. Minerva Ortopedica e Traumatology 2017;68(4):207-15. https://doi.org/10.23736/s0394-4210.17.03842-5. [ Links ]
5. Brooks PJ. Dislocation following total hip replacement: causes and cures. Bone Joint J. 2013;95-B(11 suppl A):67-69. https://doi.org/10.1302/031-620X.95B11. [ Links ]
6. Tsiridese E, Pavlou G, Venkatesh R, et al. Periprosthetic femoral fracture around hip arthroplasty. Current concepts in their management. Hip int. 2009;19(2):75-86. https://doi.org/10.1177/112070000901900201. [ Links ]
7. Sadoghi P, Pawelka W. Giebensteiner MC, et al. The incidence of implant fracture after total hip arthroplasty. Int Orthop. 2014;38:39-46. https://doi.org/10.1007/s00264-013-2110-3. [ Links ]
8. Telleria JM, Gee AO. Classification in brief: Paprosky classification of acetabular bone loss. Clin Orthop Relat Res. 2013;471(11):3725-30. https://doi.org/10.1007/s11999-013-3264-4. [ Links ]
9. Long WJ, Noiseux NO, Mabry TM, et al. Uncemented porous tantalum acetabular components: early follow-up and failures in 599 total hip arthroplasties. Iowa Orthop J. 2015;35:108-13. [ Links ]
10. Moore MS, McAuley JP, Young AM, et al. Radiographic signs of osteointegration in porous-coated acetabular components. Clin Ortho Relat Res. 2006;444:176-83. https://doi.org/10.1097/01.blo.0000201149.14078.50. [ Links ]
11. Labek G, Thaler M, Janda W, et al. Revision rates after total joint replacement: cumulative results from worldwide joint register datasets. J Bone Joint Surg [Br]. 2011;93(3):293-97. https://doi.org/10.1302/0301-620X.93B3.25467. [ Links ]
12. Ulrich SD, Seyler TM, Benett D, et al. Total hip arthroplasty: what are the reasons for revision? Int Orthop. 2008;32:597-604. https://doi.org/10.1007/s00264-007-0364-3. [ Links ]
13. Hukkanen M, Corbett SA, Batten J, et al. Aseptic loosening of total hip replacement. Macrophage expression of inducible nitric oxide synthase and cyclo-oxygenase-2, together with peroxynitrite formation, as a possible mechanism for early prosthesis failure. J Bone Joint Surg [Br]. 1997;79-B:467-74. [ Links ]
14. Grobbelaar CJ, Du Plessis TA, Van der Linder MJ, et al. Long term evaluation of polyethylene wear in total hip arthroplasty. A statistical analysis of the association between the degree of wear versus pain, interface change, osteolysis and implant failure. SA Orthop J. 2011;10(1):49-56. [ Links ]
15. Marsland D, Mears SC. A review of periprosthetic femoral fractures associated with total hip arthroplasty. Geriatr Orthop Surg Rehabil. 2012;3(3):107-20. https://doi.org/10.1177/2151458512462870. [ Links ]
16. Tokarski AT, Novack TA, Parvizi J. Is tantalum protective against infection in revision total hip arthroplasty? Bone Joint J. 2015;97-B45-9. https://doi.org/10.1302/0301-620X.97B1.34236. [ Links ]
17. Malkani AL, Prince MR, Crawford CH, et al. Acetabular component revision using a porous tantalum biomaterial: a case series. J Arthroplasty. 2009;24(7):1068-73. https://doi.org/10.1016/j.arth.2008.07.008. [ Links ]
18. Reid C, Grobler GP, Dower BJ, et al. Revision total hip arthroplasty: Addressing acetabular bone loss. SA Orthop J. 2012;11(3):34-46. [ Links ]
19. Abolghasemian M, Tangsataporn S, Sternheim A, et al. Porous metal augments: Big hope for big holes. Bone Joint J. 2013;95-B(Suppl A):103-108. https://doi.org/10.3928/01477447-20100722-29. [ Links ]
 Correspondence:
Correspondence:
Dr L Noconjo
Department of Orthopaedic Surgery, Groote Schuur, Observatory
Cape Town, 8000
tel: 021 404 5108; cell: 083 751 1356; email: lubabalonoconjo@gmail.com
Received: October 2018
Accepted: January 2020
Published: August 2020
Editor: Dr Chris Snyckers, University of Pretoria, South Africa
Funding: No funding was received for this study.
Conflict of interest: The authors declare they have no conflicts of interest that are directly or indirectly related to the research.














