Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.19 n.3 Centurion Aug./Sep. 2020
http://dx.doi.org/10.17159/2309-8309/2020/v19n3a3
PAEDIATRIC ORTHOPAEDICS
Short-term outcomes of submuscular bridge plating of length-unstable paediatric femoral shaft fractures in children - Insights from a South African tertiary hospital setting
Du Toit JI; Salkinder RII; Burger MCIII; Du Preez GIV; Lamberts RPV
IMBChB, FC Orth(SA), MSc, PhD; Professor and Head of Division, Division of Orthopaedic Surgery, Faculty of Medicine and Health Sciences, Stellenbosch University, Tygerberg, South Africa
IIMBChB, FC Orth(SA), MMed; Orthopaedic Surgeon, Cape Town Mediclinic, Oranjezicht, Cape Town, South Africa
IIIPhD; Lecturer and Scientific Research Coordinator, Division of Orthopaedic Surgery, Faculty of Medicine and Health Sciences, Stellenbosch University, Tygerberg, South Africa
IVMBChB, FC Orth(SA); Senior Specialist, Division of Orthopaedic Surgery, Faculty of Medicine and Health Sciences, Stellenbosch University, Tygerberg, South Africa
VMSc, PhD, FECSS; Professor and Head of Orthopaedic Research, Division of Orthopaedic Surgery, Faculty of Medicine and Health Sciences, Stellenbosch University, Tygerberg, South Africa
ABSTRACT
BACKGROUND: Femoral diaphyseal fracture is a common paediatric orthopaedic injury; however, the management of these fractures remains controversial in children between the ages of 6 and 13 years. The preferred approach for children appears to be surgical, enabling early mobilisation. Some studies have reported that submuscular bridge plating (SBP) might be a good alternative treatment method with favourable outcomes. The aim of this study was to determine whether SBP a) leads to union in length-unstable fractures
with a low complication rate; b) leads to reasonable alignment and leg length equality; and c) has acceptable clinical outcomes in a South African tertiary hospital setting.
METHODS: All patients with predominantly length-unstable femoral diaphyseal fractures who were treated between 1 January 2011 and 31 December 2012 were included in this study. Patients were treated with SBP using standard of care techniques, and hardware removal was performed at approximately eight months post-operatively. The nine months post-operative assessment between the affected and unaffected leg was used to assess the effectiveness of the SBP intervention
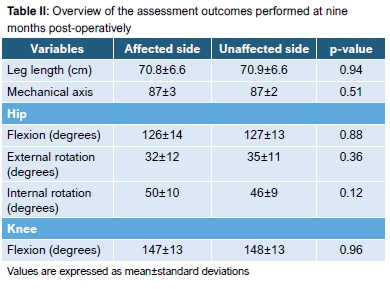
RESULTS: A total of 29 patients (mean age 9±2 years) were included. The majority of the fractures (n=27, 93%) were length-unstable. Two patients (7%) had transverse fractures with >2 cm overlap and/or weighing >45 kg. All fractures healed within expected time frames. No overall leg length discrepancy (p=0.94) or coronal mechanical axis deviation (p=0.51) was observed between the affected and unaffected lower limbs at nine months post-surgery. No differences between the operated and non-operated sides were observed for hip flexion (p=0.88), hip external rotation (p=0.36), hip internal rotation (p=0.12) or knee flexion (p=0.96
CONCLUSION: SBP provides reliable outcomes in children with diaphyseal femoral fractures and is our preferred method of fixation for a) length-unstable fractures; b) fractures close to the metaphysis; and c) children weighing more than 45 kg
Level of evidence: Level 4
Keywords: femoral fractures, paediatric, orthopaedic surgery, children
Introduction
Femoral shaft fractures are among the most common major paediatric orthopaedic injuries,1 accounting for between 1.4 and 1.7% of all fractures seen in the paediatric population.2 There remains much controversy surrounding the management of these fractures, most notably in the 6-13 years of age group, with researchers failing to reach consensus regarding the treatment strategy of choice.
Historically the majority of paediatric femoral shaft fractures have been managed conservatively,3 by means of balanced traction, splints/harnesses and/or hip spicas.3 Although most paediatric femoral fractures unite, complications including delayed union, non-union, re-fracture, leg length discrepancies and/or angular deformities are reported.1 The preferred approach for children of school-going age (6-13 years) appears to be surgical, thus enabling early mobilisation and return to school. The most appropriate surgical options remain controversial.1 The flexible intramedullary nailing system is considered to be the most appropriate option for transverse or short oblique length stable fractures in children who weigh below 45 kg.4,5 This method is not suitable for metaphyseal-diaphyseal junction or spiral/long oblique/comminuted fractures, or patients weighing in excess of 45 kg, given the decreased ability of flexible nails to maintain fracture length and rotational stability.6
In adult patients the locked intramedullary nail is the treatment of choice for femoral shaft fractures, but reports of avascular necrosis of the femoral head in children when using the piriformis entry point, make this technique a poor choice for use in paediatric populations.7 Studies investigating the result of the lateral trochanteric entry nails for children older than 8 years of age are reporting promising results, with no reports of avascular necrosis or significant alteration in the neck shaft angle.3,6 However, lateral trochanteric entry rigid nails cannot address proximal and distal fracture extension and need larger medullary canals.8
Similarly, external fixation is considered to be a safe and effective method of treatment,9,10 but reports of quadriceps contractures, re-fracturing, unsightly scars and associated pin-tract infections are significant drawbacks of this surgical approach.11,12 Traditional compression plating provides excellent stability and maintains fracture length and alignment but complications include the risk of hardware failure, re-fracture at the plate-bone interface due to stress risers, possible severe femoral overgrowth secondary to periosteal stripping, as well as a non-union rate as high as 10%.13,14 Additionally, the necessity for a large incision during surgery further limits the acceptance of this technique.14,15
Another technique to be considered is submuscular bridge plating (SBP). This technique is considered minimally invasive thus causing minimal soft tissue disruption, acts as an internal splint and provides relative stability to the fractured diaphysis, and is reported to maintain length and angulation, thus allowing for maximal biological healing.8,16 In addition, use of this technique avoids the growth plates as well as possible injury of the blood supply to the femoral head. Although it appears that SBP might avoid some of the complications and problems associated with other methodologies, reported outcomes of this treatment in children ages 6 to 13 years are limited.
Therefore, the aim of the study was to prospectively evaluate the outcome of SBP of predominantly length-unstable femoral shaft fractures in children between 6 and 13 years of age, who are treated in a South African tertiary hospital setting. Length-unstable fractures are defined as those that have a comminuted or spiral fracture pattern and/or >2 cm of shortening.
Methods
Study design
Included in this study were 30 children between the ages of 6 and 13 years, admitted to the Division of Orthopaedic Surgery at Tygerberg Hospital, Western Cape, South Africa, with a length-unstable femoral shaft fracture. Two children who sustained transverse diaphyseal fractures with >2 cm of shortening and who weighed more than 45 kg were included in the cohort.
Surgical procedure
Patients awaiting surgery were stabilised and placed in balanced traction with a Thomas splint as an interim immobilisation technique until the definitive surgical intervention.
The patient was placed supine on a traction table and the fracture was provisionally reduced by in-line traction. Moderate coronal and sagittal malalignment were accepted as this is corrected by the subsequent placement of the pre-contoured plate, but rotation and length were confirmed as corrected both clinically and with fluoroscopy.
A Synthes® 4.5 mm staggered low contact-dynamic compression (LC-DC) plate with locking options was used. The plate was overlaid over the injured thigh and the appropriate plate length was selected under fluoroscopic guidance. It was contoured using a bending press to the shape of the femur using the pre-operative radiographs as well as the intra-operative screening radiographs as templates. A 3-4 cm longitudinal lateral incision was placed proximally for more proximally situated fractures and distally for distal or midshaft fractures (Figure 1). The plate was then advanced sub-muscularly along the femoral shaft (Figure 2a), after which the plate was centred and screws were inserted through stab incisions placed over the desired holes, and the fracture was reduced to the plate (Figures 2b-e).

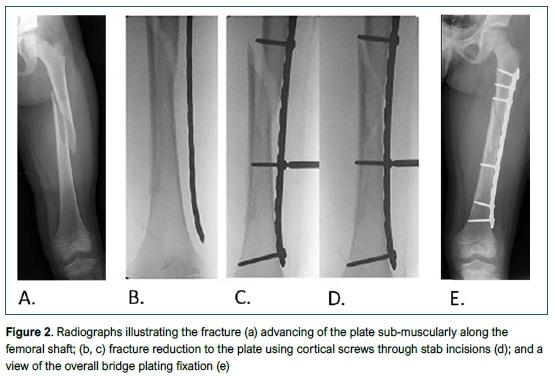
The first two screws were placed near the proximal and distal ends of the plate and thereafter two compression screws were placed proximal and distal to the fracture. If indicated, these compression screws aided in fracture reduction. The aim was to obtain fixation into six cortices on either side of the fracture. Compression screws were used unless the fracture extended into the metaphysis or there were concerns with regard to stability. In these cases, locked screws were used on that side. Wounds were closed in layers with subcutaneous absorbable sutures for the skin. A post-operative radiograph was taken prior to discharge to assess the initial fixation. Patients were discharged once they were able to mobilise with partial weight bearing using either crutches or a walking frame. Progressive weight bearing was allowed once fracture callus was seen on follow-up radiographs.
Radiographic measurements
Radiographs (antero-posterior and lateral) were taken on admission. The fractures were classified according to the anatomic and descriptive classification systems as previously described. Patients returned to the hospital for follow-up assessments at two weeks, six weeks and three months, and radiographs were taken for assessment of fracture union, acceptable alignment and/or hardware complications. Approximately eight months post-operatively, patients returned to the hospital for the removal of the plate during a second surgical intervention.
A final follow-up assessment was performed at nine months post-surgery. In addition to the normal clinical assessment of range of motion and rotational profile, long leg standing antero-posterior and lateral radiographs were taken to assess the mechanical lateral distal femoral angle (mLDFA). These were compared to the non-operated side using the PACS radiological system. Leg length differences between the operated and non-operated sides were also assessed with the use of these radiographs, and any wound-related complications recorded.
Statistical analysis
The data was analysed with Statistica 11.0 (Sta-soft Inc, Tulsa, OK, USA). Distribution and homogeneity of the data was checked with a Levene test. As data was normally distributed, data was expressed as mean±standard deviation. Differences at nine months between the affected and unaffected leg were analysed with the t-test for independent samples. A significant difference was accepted at a p<0.05.
Results
Participant characteristics
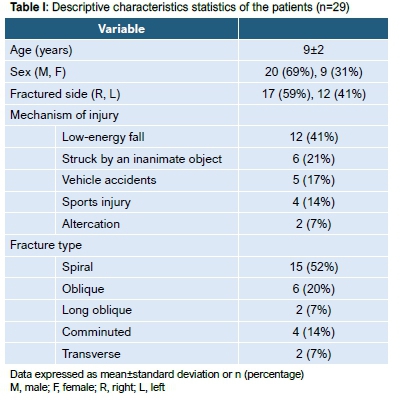
A total of 30 patients were included in this study with one patient failing to complete follow-up. General characteristics of the included patients are shown in Table I. All patients presented with closed fractures barring one that sustained a Gustilo-Anderson grade 1 open femur fracture.
Surgical details
The mean operating time was 66±15 minutes, with average total incision length of 10.4±2.7 cm (range 6-16). Incision length was calculated as the sum of the initial proximal or distal incision (entry portal for the submuscular plate) as well as the three to five additional stab incisions for indirect screw placement. A13-hole plate was used most frequently for fixation. The mean radiation exposure amounted to 88±28 seconds (range 23-138) and the average blood loss during the procedure amounted to 121±83 ml (range 20-400).
Radiographic and clinical outcomes
All 29 patients revisited the hospital for their two- and six-week follow-ups as well as the three-month follow-up assessment.
Radiographs showed that all fractures were fully united by three months post-surgery.
Plates were removed at an average of 8±3 months post-plating. Mean surgical time was 32±9 minutes and blood loss 48±39 ml. Screening time ranged from 0.01 to 60 seconds with the mean being 6±12 seconds.
Outcomes of the nine-month follow-up assessment which included leg length, coronal mechanical axis, as well as hip and knee flexibility are shown in Table II.
Due to severe bony overgrowth overlying the plate, with subsequent difficulty of plate removal, a prolonged screening time (60 seconds) was necessary in one case. One major complication of a femur being plated in 25 degrees of internal rotation occurred but did not cause any functional or cosmetic disturbance to the patient. The patient and his parents decided against further surgical correction. One final, minor complication of hypertrophic scars was observed, which was treated conservatively.
Discussion
The treatment of paediatric femoral shaft fractures, particularly in the 6 to 13 year age group, has in recent times moved away from the traditionally conservative approach.17 Several methods of fixation are available with the fracture pattern and specific patient and economic factors guiding the decision of which approach to use.17,18
Although each surgical approach has its merit, each also comes with specific drawbacks, depending on the patient characteristics and fracture pattern. The flexible nail, for example, is appropriate for use in stable fractures in smaller patients, but use in complex, proximal or distal fractures or in heavier children is associated with higher complication rates.4,5,8,19 In turn, compression plating requires large incisions with the associated increased risk of infection and delayed healing.14,15 External fixation preserves blood supply and offers increased stability, but has a higher incidence of pin-tract infections and high refracture rates.20
The main finding of this study is that SBP is a viable and predictable method of fixation for length-unstable paediatric femoral shaft fractures. This technique was used in 30 patients with length-unstable fractures, and fracture reduction was maintained with no significant leg length discrepancy or malalignment in the axial or coronal planes. Reduction was maintained and all fractures were united within three months. We report one major complication of rotational malalignment, which was caused by a preventable technical error.
In-theatre variables compare favourably with other methods of fixation: the mean operating time of 67±14 minutes for the index procedure in this study was less than that reported in two previous studies where submuscular plating was used, where the mean operating time was reported to be 89 minutes and 106 minutes, respectively.8,16 Theatre time is an important factor to take into account, especially in high-volume settings. The time required in this study compares well to other methods of fixation, with a mean surgical time of 56 minutes for external fixation and 74 minutes for flexible intramedullary nail fixation for femoral shaft fractures being reported by Bar-On et al. in 1999.21 Screening time should ideally be kept as limited as possible. The current study's mean exposure time of 88 seconds was slightly increased compared to the means of 56 and 84 seconds reported, respectively, for similar studies,8,16 but compares favourably against external fixation and the flexible nail which had reported screening times of 1.4 and 2.6 minutes, respectively.21 Open reduction techniques such as compression plating allow for minimum screening exposure but this invasive technique is not generally recommended due to the large incision, loss of the fracture haematoma as well as the moderate blood loss associated with this technique. Caird et al. reported an average blood loss of 200 ml (range 40-1 500) during a series of 60 compression plating procedures.14 Similarly, in their bridge plating study of 69 femoral fractures, Abdelgawad et al. reported blood loss to be 121 ml (range 20-500).8
All fractures that were included in the present study had united by three months post-surgery.22,23 No differences between leg length, hip and knee range of motion and alignment in the axial or coronal planes were observed at our final follow-up visit at nine months post-surgery. These results were not influenced by patient age, mechanism of injury or type of fracture. In their study which also utilised SBP, Kanlic et al. reported leg length discrepancies of between 5 and 23 mm in 8% of their study population (n=4 of 51).16 The elastic nail, which is considered a treatment of choice for length-stable fractures, does not compare as favourably when used to treat length-unstable fractures, with a reported complication rate of 80% in a 2005 study using this technique.19 Similarly, studies using external fixation for femoral shaft fractures in children report less than desirable outcomes including malrotation in 43% of patients10 and leg length discrepancies of up to 20 mm.9-11,21 We agree with previous authors who suggested that external fixation be reserved for polytrauma patients or those with high-grade open femur fractures.20,21
We report one patient where difficulty was encountered in removing hardware that had been in situ for ten months and we therefore recommend removal at six months post-surgery. We experienced no refractures, hardware failures or wound infections. We do, however, report on one major complication with a patient's femur being plated in 25 degrees of internal rotation. In critical review of the case, it was determined that during placement of the patient on the traction table, the upper body and pelvis were inadvertently rotated externally in relation to the distal femur, while the knee was maintained with the patella facing anterior which caused the malrotation. Reported complications in previous bridge plating studies ranged from none,22,24 two reports of hardware failure,8,16 one report of deep infection in a polytrauma patient8 and one refracture.16
Conclusion
The findings of the current study show that in a South African tertiary hospital setting, good results can be achieved when treating length-unstable paediatric femoral shaft fractures with SBP. These finding are in line with previous SBP studies which showed that this technique is a potential alternative to treatment of length-unstable femoral fractures, regardless of fracture type/location, mechanism of injury, patient age or patient weight. It is a minimally invasive technique with resultant small, well-accepted scars which allows for early mobilisation and discharge.
Similar to other surgical options, the only major disadvantage is the requirement for a secondary surgical procedure for hardware removal. This study is, however, not without limitations which include the relatively small sample size and short follow-up study. Although reporting these initial findings of this bridge plating, it is also important to conduct a long-term follow-up study focusing on the long-term effects of this treatment regimen in children who are being treated in a South African tertiary hospital setting.
In conclusion, this study provides further evidence supporting the use of SBP in length-unstable femoral shaft fractures in children between the ages of 6 to 13 years who are being treated in a South African tertiary hospital setting.
Ethics statement
Prior to participation, the parents of all patients were informed about the procedures and gave written informed consent. This study was approved by the Health Research Ethics Committee of the Faculty of Medicine and Health Sciences within the University of Stellenbosch (N10/11/350) and institutional permission was obtained, while the principles outlined in Declaration of Helsinki were followed.25
Declaration
The authors declare authorship of this article and that they have followed sound scientific research practice. This research is original and does not transgress plagiarism policies.
Author contributions
JdT: Conceptualisation, design, manuscript preparation, supervisor
RS: Manuscript preparation, design, data collection
MB: Manuscript preparation
GdP: Manuscript preparation
RL: Design, data analyses, manuscript preparation, supervisor
ORCID
Du Toit J https://orcid.org/0000-0002-0958-5450
Burger MC https://orcid.org/0000-0003-2831-4960
Du Preez G https://orcid.org/0000-0003-2760-7307
Lamberts RP https://orcid.org/0000-0003-1112-2604
References
1. Flynn JM, Schwend RM. Management of pediatric femoral shaft fractures. J Am Acad Orthop Surg. 2004;12(5):347-59. https://doi.org/10.5435/00124635-200409000-00009. [ Links ]
2. Kocher MS, Sink EL, Blasier RD, et al. Treatment of pediatric diaphyseal femur fractures. J Am Acad Orthop Surg. 2009;17(11):718-25. https://doi.org/10.5435/00124635-200911000-00006. [ Links ]
3. Chitgopkar SD. Internal fixation of femoral shaft fractures in children by intramedullary Kirschner wires (a prospective study): its significance for developing countries. BMC Surg. 2005;5:6. https://doi.org/10.1186/1471-2482-5-6. [ Links ]
4. Li Y, Stabile KJ, Shilt JS. Biomechanical analysis of titanium elastic nail fixation in a pediatric femur fracture model. J Paediatr Orthop. 2008;28(8):874-78. https://doi.org/10.1097/BPO.0b013e31818f1136. [ Links ]
5. Barry M, Paterson JMH. Flexible intramedullary nails for fractures in children. J Bone Joint Surg Br. 2004;86(7):947-53. https://doi.org/10.1302/0301-620x.86b7.15273. [ Links ]
6. Flynn J, Hresko T, Reynolds R, et al. Titanium elastic nails for pediatric femur fractures: a multicenter study of early results with analysis of complications. J Paediatr Orthop. 2001;21 (1):4-8. https://doi.org/10.1097/00004694-200101000-00003. [ Links ]
7. MacNeil J, Francis A, El-Hawary R. A systematic review of rigid, locked, intramedullary nail insertion sites and avascular necrosis of the femoral head in the skeletally immature. J Pediatr Orthop. 2011;31(4):2009-12. https://doi.org/10.1097/BPO.0b013e3182172613. [ Links ]
8. Abdelgawad A, Sieg R, Laughlin M, Shunia J, Kanlic E. Submuscular bridge plating for complex pediatric femur fractures is reliable. Clin Orthop Relat Res. 2013;471 (9):2797-807. https://doi.org/10.1007/s11999-013-2931-9. [ Links ]
9. Blasier RD, Aronson J, Tursky EA. External fixation of pediatric femur fractures. J Paediatr Orthop. 1997;17(3):342-46. [ Links ]
10. Sola J, Schoenecker PL, Gordon JE. External fixation of femoral shaft fractures in children : enhanced stability with the use of an auxiliary pin. J Paediatr Orthop. 1999;19(5):587-91. [ Links ]
11. Miner T, Carroll KL. Outcomes of external fixation of pediatric femoral shaft fractures. J Pediatr Orthop. 2000;20(3):405-10. [ Links ]
12. Keeler KA, Dart B, Luhmann SJ, et al. Antegrade intramedullary nailing of pediatric femoral fractures using an interlocking pediatric femoral nail and a lateral trochanteric entry point. J Paediatr Orthop. 2009;29(4):345-51. https://doi.org/10.1097/BPO.0b013e3181a53b59. [ Links ]
13. Fyodorov I, Sturm PF, Robertson WWJ. Compression-plate fixation of femoral shaft fractures in children aged 8 to 12 years. J Paediatr Orthop. 1999;19(5):578-81. [ Links ]
14. Caird MS, Mueller KA, Puryear A, Farley FA. Compression plating of pediatric femoral shaft fractures. J Paediatr Orthop. 2003;23(4):448-52. [ Links ]
15. Eren OT, Kucukkaya M, Kockesen C, Kabukcuoglu Y, Kuzgun U. Open reduction and plate fixation of femoral shaft fractures in children aged 4 to 10. J Paediatr Orthop. 2003;23(2):190-93. [ Links ]
16. Kanlic EM, Anglen JO, Smith DG, Morgan SJ, Pesántez RF. Advantages of submuscular bridge plating for complex pediatric femur fractures. Clin Orthop Relat Res. 2004:426:244-51. https://doi.org/10.1097/01.blo.0000138961.34810.af. [ Links ]
17. Gardner MJ, Lawrence BD, Griffith MH. Surgical treatment of pediatric femoral shaft fractures. Curr Opin Pediatr. 2004;16(1):51-57. https://doi.org/10.1097/00008480-200402000-00010. [ Links ]
18. Beaty JH. Operative treatment of femoral shaft fractures in children and adolescents. Clin Orthop Relat Res. 2005;434:114-22. https://doi.org/10.1097/01.blo.0000163463.05141.1c. [ Links ]
19. Sink EL, Gralla J, Repine M. Complications of pediatric femur fractures treated with titanium elastic nails: a comparison of fracture types. J Paediatr Orthop. 2005;25(5):577-80. https://doi.org/10.1097/01.bpo.0000164872.44195.4f. [ Links ]
20. Kanlic E, Cruz M. Current concepts in pediatric femur fracture treatment. Orthopedics. 2007;30(12):1015-19. https://doi.org/10.3928/01477447-20071201-03. [ Links ]
21. Bar-On E, Sagiv S, Porat S. External fixation or flexible intramedullary nailing for femoral shaft fractures in children. A prospective randomized study. J Bone Joint Surg Br. 1997;79(6):974-78. https://doi.org/10.1302/0301-620x.79b6.7740. [ Links ]
22. Sink E, Hedequist D, Morgan S, Hresko T. Results and technique of unstable pediatric femoral fractures treated with submuscular bridge plating. J Paediatr Orthop. 2006;26(2):177-81. https://doi.org/10.1097/01.bpo.0000218524.90620.34. [ Links ]
23. Agus H, Kalenderer O, Eryanilmaz G, Omeroglu H. Biological internal fixation of comminuted femur shaft fractures by bridge plating in children. J Pediatr Orthop. 2013;23(2):184-89. [ Links ]
24. Samora WP, Guerriero M, Willis L, Klingele KE. Submuscular bridge plating for length-unstable, pediatric femur fractures. J Pediatr Orthop. 2013;33(8):797-802. https://doi.org/10.1097/BPO.0000000000000092. [ Links ]
25. Sussman MD. Ethical standards in the treatment of human subjects involved in clinical research. J Pediatr Orthop. 1998;18(6):701-702. [ Links ]
 Correspondence:
Correspondence:
Prof. Robert P Lamberts
Division of Orthopaedic Surgery, Department of Surgical Sciences, Stellenbosch University, Tygerberg Campus
PO Box 19063, Tygerberg, 7505, South Africa
tel: +27 (0)21 938 9266; email: rplam@hotmail.com or roblam@sun.ac.za
Received: November 2019
Accepted: February 2020
Published: August 2020
Editor: Prof. Leonard C Marais, University of KwaZulu-Natal, Durban, South Africa
Funding: No funding was received for this study.
Conflict of interest: The authors declare they have no conflicts of interest that are directly or indirectly related to the study.














