Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.19 n.1 Centurion Feb./Mar. 2020
http://dx.doi.org/10.17159/2309-8309/2020/v19n1a1
PAEDIATRIC ORTHOPAEDICS
Femoral lengthening in children
Horn AI; Sipilä MII
IMBChB(UP), MMed Ortho(UCT)(Hons), FC Orth(SA); Consultant orthopaedic surgeon, Red Cross War Memorial Children's Hospital, Cape Town; Department of Orthopaedic Surgery, University of Cape Town, South Africa
IIMBChB; Registrar, Department of Surgery, Kymenlaakson Keskussairaala Hospital, Helsinki, Finland
ABSTRACT
BACKGROUND: We evaluated the outcomes following femoral lengthening by distraction osteogenesis in children. Additionally, we determined the incidence and nature of complications, the management thereof and factors associated with the development of complications
METHOD: A retrospective review was performed of all patients who underwent femoral lengthening as an isolated procedure at our institution. Data regarding presenting details and clinical course were collected and X-rays analysed. The healing index (HI) and the percentage lengthened were calculated. Complications were defined as deep sepsis, joint contracture, fracture and neurological injury
RESULTS: Fifteen patients underwent 16 femoral lengthenings from 2008-2018. Nine patients had congenital short femur or proximal focal femoral deficiency, three patients had sequelae of meningococcaemia and four had various other pathologies. The median age at time of surgery was 9 years (6-13). Median follow-up was 1.6 years (0.5-6.6). The median HI was 32 days/cm (20-60). Leg lengths were equalised to <2.5 cm in 11 patients; length achieved was as planned in all but three patients. Eight patients sustained fractures on average six days (2-57) after frame removal, Ave through the regenerate. Four required surgery. Thirteen patients developed joint contractures of which six required additional procedures to address this. Two deep infections required surgery. Two patients developed neurological symptoms of which one recovered fully. Higher percentage length gained (>20%) was associated with increased fracture and joint contracture rate. Diaphyseal osteotomy, as opposed to metaphyseal, was associated with increased risk of fracture (71% vs 25%). A diagnosis of congenital short femur was associated with increased fracture rate. Spanning the knee did not prevent joint stiffness in 4/5 patients but did prevent subluxation
CONCLUSION: Femoral lengthening using external fixation can be successful in achieving leg length equality, but complications are common and often require additional surgery. Limiting lengthening to less than 20% of the original bone length and performing the osteotomy through the metaphysis decreases the risk of fracture and joint contracture
Level of evidence: Level 4
Keywords: femoral lengthening, distraction osteogenesis, leg length discrepancy, congenital short femur
Introduction
Leg length discrepancy (LLD) may arise secondary to a variety of conditions including congenital deficiencies, overgrowth syndromes and post-traumatic or post-infectious sequelae. LLD can result in gait inefficiency and back pain. Osteoarthritis of the hips and spine in adulthood have been associated with LLD.1
Less than 2 cm LLD is normally compensated for, or a shoe raise may be used if symptomatic. Up to 5 cm LLD can be treated with epiphysiodesis of the longer leg. An LLD of more than 5 cm is best treated with limb lengthening with or without contralateral epiphysiodesis.2 This is achieved by performing distraction osteogenesis or callotasis, as described by Ilizarov3 and DeBastiani.4 There are three commonly used devices for performing femoral lengthening: a circular fixator, a monolateral rail or an intramedullary device.1,5 Circular fixators provide more stability than monolateral rails. They also provide the option of deformity correction but are generally poorly tolerated. Monolateral rails are better tolerated, but more commonly lead to regenerate deformation.1 Intramedullary devices have been proven to be effective and very well tolerated, but excessive cost limits its use in developing countries. Complications using external devices are universal. Nearly all patients get pin-site infection, and many develop fractures, either through the regenerate or through the pin sites. Neurological complications and joint contractures are frequently encountered but are also seen with the use of intramedullary devices.3,5-7 Spanning the knee has been suggested to prevent stiffness and subluxation of the knee joint.7
The purpose of this study is to evaluate the outcomes and complications following femoral lengthening at the Maitland Cottage Children's Orthopaedic Hospital in Cape Town, South Africa, between 2008 and 2018. We also wish to identify any modifiable factors, if present, that predisposes to the development of complications.
Patients and methods
We performed a retrospective review of all patients that underwent femoral lengthening as a primary procedure from 2008-2018 at our institution. Patients were excluded if the femoral lengthening formed part of a pelvic support osteotomy.
Medical records were analysed and data collected with regard to presenting pathology, procedures performed, clinical course, complications and outcome.
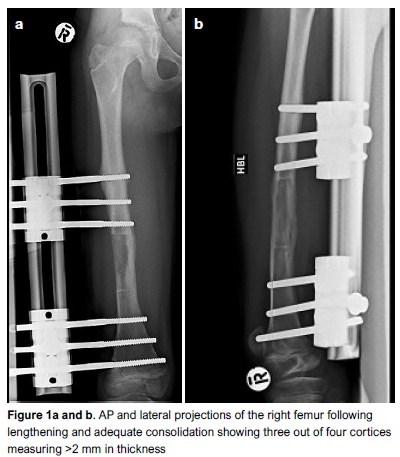
Radiographs were frequently taken throughout the course of treatment. Leg length views were taken prior to surgery to measure the LLD. Radiographs of the affected femur were taken immediately post-op to ensure completeness of the osteotomy and correct pin placement. During the distraction period, radiographs were repeated on a two-weekly basis, and once lengthening was complete, four-weekly until adequate consolidation was evident. Regenerate was deemed adequately consolidated once three out of four cortices measured at least 2 mm on radiographs and the lengthening device was subsequently removed (Figure 1).
For each patient the ratio between the amount of length obtained and the total length of the bone, measured from the tip of the greater trochanter to the intercondylar notch, was calculated and expressed as a percentage. The healing index (HI) was calculated by determining the amount of time spent in the external device for the amount lengthened using the units days/cm.4
We documented whether the osteotomy was performed in the proximal or distal metaphyseal area, or in the diaphysis. X-rays taken just prior to removal of the lengthening device were analysed to determine the amount of lengthening achieved and the presence or absence of three out of four cortices on the AP and lateral projections.
For our series, complications were defined as pin-site infections requiring surgical revision, adjacent joint stiffness or subluxation, neurological injury and fracture.
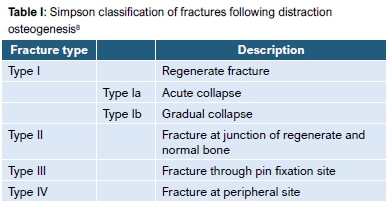
Fractures were classified using the system suggested by Simpson et al.8 (Table I).
Lengthening protocol
All except one patient had lengthening performed using a monolateral rail (Orthofix, Verona, Italy). In the remaining patient a Taylor Spatial Frame (TSF, Smith & Nephew, Memphis, Tennessee) was used. (This method was tried once but abandoned due to patient discomfort and complications.) Fixating pins and wires were placed in the standard fashion and the osteotomy was performed as described by DeBastiani.4 Antiseptic dressings were applied to the pin sites until healing was evident. Following surgery, a latency period of 5-7 days was observed prior to initiation of lengthening. Lengthening was performed at a rate of 1 mm a day, 0.25 mm six hourly. Lengthening was slowed down, and on occasion reversed, if joint stiffness or subluxation became evident. Lengthening was terminated once the desired length was achieved or once joint stiffness, subluxation or neurological symptoms precluded any further lengthening. All patients remained in hospital during the period of lengthening, and the majority of patients remained until consolidation and removal of the lengthening device. During the hospitalisation period, patients received daily physiotherapy with progressive weight bearing and joint mobilisation.
For the purpose of this study, complications were defined as deep infection requiring surgical revision, joint stiffness or subluxation requiring intervention, neurological injury and fracture. Patient outcome was evaluated retrospectively on the grounds of clinical notes and radiographs. Factors considered were equalisation of leg lengths, presence of residual deformity and joint mobility.
Due to the relatively small number of patients, no formal statistical analysis was performed. Descriptive statistics will be presented.
Results
Following exclusions, we identified 15 patients that underwent 16 femoral lengthenings for various aetiologies. The presenting details, as well as the details of surgery and healing are summarised in Table II. The median age at surgery was 9 years (6-13 years). Median follow-up was 1.6 years following femoral lengthening (0.5-6.6 years) The most common cause for femoral shortening was congenital short femur followed by the sequelae of meningococcal septicaemia.
An Orthofix Limb Reconstruction System (LRS) was used in all patients except patient 5 in whom a TSF was used. The knee was spanned in six patients and the hip in one. Mean length obtained was 54 mm (range 35-80). The mean percentage lengthened was 20% (range 8-32%). The mean HI was 32 days/cm (range 20-60). Lengthening was abandoned prior to the desired length being obtained in four patients due to knee stiffness or knee/hip subluxation.
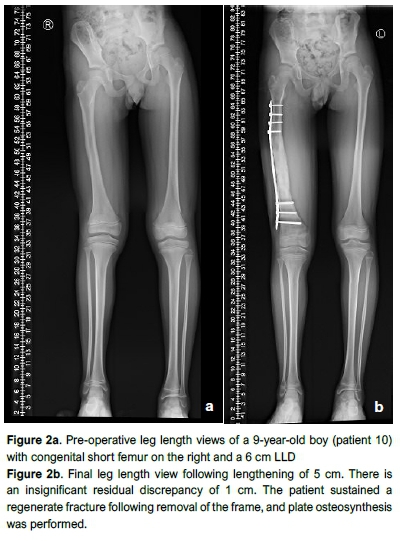
Complications encountered and outcome following femoral lengthening is summarised in Table III. Leg length equality was achieved in five patients. Six patients had residual discrepancies at latest follow-up of <2.5 cm which was managed with an orthosis and well tolerated (Figure 2). In four patients, a significant LLD remains. One patient is still awaiting tibial lengthening (pt 10), two patients have residual discrepancies of 5 cm and 12 cm respectively (pts 14 and 7) but are functioning well and do not desire any further surgery. Patient 5 has ongoing neurological pain and LLD as well as contracture of the knee and ankle. Amputation was offered but the family refused any further surgery.
Our patients developed many complications. Nine patients (50%) sustained fractures of which seven were through the regenerate (Figure 3). Fracture occurred on average six days (range 2-57) following removal of the distracting device. Four patients required additional procedures to manage the fracture.

Thirteen patients developed joint contractures and six required additional procedures including one quadricepsplasty, one distal femoral extension osteotomy and one guided growth procedure for a fixed flexion deformity of the knee.
Eight of our patients developed superficial pin-site infections requiring oral antibiotics and pin-site care only. Two patients developed deep infections requiring surgery. Two patients developed neurological symptoms, of which one recovered fully.
There was no difference in age between patients who sustained fractures (11.4 years) and those who did not (11.3 years). The diagnosis of congenital short femur was associated with an increased rate of fracture following lengthening. Five out of seven patients with this diagnosis sustained a fracture. Patient 15 lost all the length gained due to the regenerate fracture; the other fractures did not result in any significant loss of length.
The development of a fracture was associated with a higher average percentage lengthened (21.4% vs 16.9%). The incidence of fracture in patients who had >20% lengthened was 62.5% compared to 37.5% in those with <20% lengthened. Regenerate fractures occurred in six out of seven patients in whom the osteotomy was performed in the mid-diaphysis. There was no clear association between the HI and the development of fractures. The median HI was 30 days/cm (20-38) and 28 days/cm (22-60) for those that sustained fractures and those that did not, respectively.
Nearly all patients developed loss of range of motion in either the knee or the hip. There was no association between the percentage length gained and the need for secondary procedure for joint stiffness. Spanning of the knee did not prevent joint stiffness but did prevent joint subluxation. Only one patient, patient 7, developed a knee subluxation during his second lengthening. The fixator was subsequently extended to cross the knee joint. The same patient, and one other (patient 13) developed hip subluxation. Patient 7 underwent a shelf acetabuloplasty to address the subluxation; patient 13 still had a subluxed hip at last follow-up but refused further surgery.
There were no cases of premature consolidation. Delayed consolidation was not documented but no patients underwent bone graft or cyst aspiration during the consolidation phase.
Discussion
There are many conditions that can result in an LLD requiring limb lengthening. The majority of cases in our study were congenital shortening, with the rest consisting of post-traumatic, post-infectious and neurological causes. A similar spectrum of disease is described in other published series.5,9
The HI for our patients was on average 30 days/cm. This is quite low when compared to the literature. Launay et al. ,5 and Aston et al.10reported HI in their series of 45.1 days/cm and 39.97 days/cm respectively. It is likely that our high fracture rate may be ascribed to premature removal of the fixator device, although there was no difference in the HI between those that fractured and those that did not.
Fracture following removal of the lengthening device was the most common complication in our series (8/16 segments). Fracture rates described in the literature vary from 9.3% to 56%.8,10 In our series we found an association between the percentage of bone lengthened and the incidence of fractures, with an increased rate of fracture in those lengthened more than 20%. Aston et al. found an increased rate of delayed consolidation in patients lengthened more than 6 cm and an increased rate of fracture in those lengthened more than 20%.10 Launay et al. reports a more conservative upper limit for percentage lengthened of 15%.5 Simpson et al., in a large series of 157 adults and adolescents, demonstrated no association between the length of the regenerate and fracture rate.8
We had an increased rate of fracture in patients with congenital deficiencies (Ave out of seven limbs lengthened). Patients with congenital shortening are known to develop poor regenerate and to be more prone to fractures through the regenerate, with rates of up to 56% reported.5,10
Efforts have been made to reduce the rate of fracture by lengthening over an intramedullary nail. A significant decrease in fracture rate is reported with this modification, as well as reduced time before removal of the fixator.10,11
Superficial pin-site infection developed in 50% of our patients and is regarded as a problem, not a complication.12 All superficial infections responded well to oral antibiotics and pin-site care. Deep pin-site infection requiring surgical revision occurred in two patients (13%). These rates are comparable to the published literature.9,10 We had no pin breakages but one fracture of the distracting device requiring revision.
Seven patients developed joint stiffness or subluxation requiring a surgical intervention, often in the form of a manipulation under anaesthesia. We found no association between the amount lengthened or the underlying diagnosis and the incidence of stiffness/subluxation. Higher rates of stiffness and subluxation have been reported in patients with congenital deficiencies, possibly due to inherent instability of the knee.9,10
Two of our patients developed sciatic and peroneal nerve injury, of which one resolved. The patient in whom the neurological injury did not resolve underwent simultaneous femoral and tibial lengthening. Aston et al. reports a 10% rate of neurological injury, all of which resolved spontaneously and were more common in ipsilateral tibial and femoral lengthening.10
Despite the high rate of complications, we had satisfactory outcomes in 80% of our patients in whom leg lengths were equalised (Ave patients) or insignificant discrepancy remained (six patients), and joint mobility was restored to a functional range.
The use of intramedullary lengthening nails, particularly the new generation magnetic lengthening nails, has offered a less invasive and more acceptable option for lengthening in the absence of significant deformity. These devices reduce the rate of device-related complications such as pin-site sepsis, muscle tethering and scarring, but do not reduce the rate of complications inherent to the distraction procedure such as premature or delayed consolidation, neurological injury and joint stiffness or subluxation.13 The use of these devices is mostly limited by their excessive cost, and limb lengthening using an external fixator remains the gold standard, especially in small paediatric bones and in the presence of significant deformity.
Limitations of this case series include that it is retrospective and therefore lengthening protocols were not standardised. No formal outcome classification was used, and we relied on case notes and radiographs to determine the outcome. A small number of patients were included, making relevant statistical analysis impossible. Our patients suffered from various conditions and our numbers were too small to elucidate any specific role that aetiology may play.
Conclusion
We present a small series of patients undergoing femoral lengthening for the treatment of LLD due to a variety of aetiologies. Our complication rate, though high, is comparable to the existing literature and our outcomes satisfactory in 80% of patients. More complications are encountered when distracting more than 20% of the initial length of the bone and when performing osteotomies in the mid-diaphysis. It is advisable to span the adjacent joint if a long lengthening is planned. Fracture rate may be reduced by lengthening over an intramedullary nail. Patients should be adequately counselled regarding the expected complications and the management thereof.
Ethics statement
Prior to commencement of this study, ethical approval was obtained from the University of Cape Town Human Research Ethics Committee. Ref 260/2018 Dr Anria Horn 15/05/2019.
Declaration
The authors declare authorship of this article and that they have followed sound scientific research practice. This research is original and does not transgress plagiarism policies.
Author contributions
AH and MS both contributed to data capturing and compiling of the final submission.
ORCID
Horn A http://orcid.org/0000-0002-4159-6520
Sipila M http://orcid.org/0000-0002-3751-7666
References
1. Halanski MA, Noonan KJ. Limb length discrepancy. In: Weinstein SL, Flynn JM (eds). Lovell and Winter's Paediatric Orthopaedics. 7th ed. Philidelphia: Lippincott Williams & Wilkins; 2011:1341. [ Links ]
2. Dahl MT, Gulli B, Berg T. Complications of limb lengthening. A learning curve. Clin Orthop Relat Res. 1994;301:10-18. [ Links ]
3. Ilizarov GA. The tension-stress effect on the genesis and growth of tissues. Part I. The influence of stability of fixation and soft-tissue preservation. Clinic Orthop Relat Res. 1989;238:249-81. [ Links ]
4. DeBastiani G, Aldegheri R, Renzi-Brivio L, Trivella G. Limb lengthening by callus distraction (callotasis). J Pediatr Orthop. 1987;7(2):129-34. [ Links ]
5. Launay F, Younsi R, Pithioux M, Chabrand P, Bollini G, Jouve J-L. Fracture following lower limb lengthening in children: a series of 58 patients. Orthop Traumatol Surg Res. 2013;99(1):72-79. [ Links ]
6. Dammerer D, Kirschbichler K, Donnan L, Kaufmann G, Krismer M, Biedermann R. Clinical value of the Taylor Spatial Frame: a comparison with the Ilizarov and Orthofix fixators. J Child Orthop. 2011;5(5):343-49. [ Links ]
7. Prince DE, Herzenberg JE, Standard SC, Paley D. Lengthening with external fixation is effective in congenital femoral deficiency. Clinic Ortho Relat Res. 2015;473(10):3261-71. [ Links ]
8. Simpson A, Kenwright J. Fracture after distraction osteogenesis. J Bone Joint Surg Br. 2000;82(5):659-65. [ Links ]
9. Eralp L, Koacoglu M, Bilen FE, Balci HI, Toker B, Ahmad K. A review of problems, obstacles and sequelae encountered during femoral lengthening: uniplanar versus circular external fixator. Acta Orthop Belg. 2010;76(5):628. [ Links ]
10. Aston W, Calder P, Baker D, Hartley J, Hill R. Lengthening of the congenital short femur using the Ilizarov technique: a single-surgeon series. J Bone Joint Surg Br. 2009;91 (7):962-67. [ Links ]
11. Popkov D, Popkov A, Haumont T, Journeau P, Lascombes P. Flexible intramedullary nail use in limb lengthening. J Pediatr Orthop. 2010;30(8):910-18. [ Links ]
12. Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990;250:81-104. [ Links ]
13. Paley D. PRECICE intramedullary limb lengthening system. Expert Rev Med Devices. 2015;12(3):231-49. [ Links ]
 Correspondence:
Correspondence:
Dr Anria Horn
Department of Orthopaedic Surgery, Room H49, Old Main Building
Groote Schuur Hospital, Observatory, Cape Town, 7701
Tel: +27 21 404 5108; Email: anria.horn@uct.ac.za
Received: May 2019
Accepted: September 2019
Published: March 2020
Funding: No funding was received for this study.
Conflict of interest: Both authors have no conflicts of interest to declare.














