Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.18 n.3 Centurion Aug./Sep. 2019
http://dx.doi.org/10.17159/2309-8309/2019/v18n3a2
PAEDIATRIC ORTHOPAEDICS
Profile of patients with Blount's disease at an academic hospital
Mehtar MI; Ramguthy YII; Firth GBIII
IMBBCh, FC Orth(SA), MMed(Orth); Registrar ;Department of Orthopaedic Surgery, University of the Witwatersrand, Chris Hani Baragwanath Academic Hospital, Johannesburg, South Africa
IIMBBCh, FCS(Orth); Consultant; Department of Orthopaedic Surgery, University of the Witwatersrand, Chris Hani Baragwanath Academic Hospital, Johannesburg, South Africa
IIIMBBCh, FCS(Orth), MMed(Orth); Consultant; Department of Orthopaedic Surgery, University of the Witwatersrand, Chris Hani Baragwanath Academic Hospital, Johannesburg, South Africa
ABSTRACT
BACKGROUND: Despite an apparent increased burden of Blount's disease in South Africa, little is known of its epidemiology and associated features. The aim of this study is to explore the profile of South African patients with Blount's disease seen at an academic hospital, with respect to family history, ethnicity, associated milestones, sex, bilateral involvement and obesity
METHODS: We retrospectively evaluated the hospital records of children diagnosed with Blount's disease (infantile, juvenile and adolescent groups) over a 14-year period, from 1 January 2003 to 31 December 2016 at Chris Hani Baragwanath Academic Hospital. Demographic information including family history, ethnicity, attainment of milestones, age when the deformity was first noticed, age at presentation, sex, bilateral involvement and body mass index were documented
RESULTS: Data was available for 108 patients with a total of 172 involved limbs. In this series all patients were of black African origin. Data for 60 of the patients regarding family history was available - there were 12 documented cases with a positive family history of significant bow legs (20%). The developmental milestones of patients within all three groups were within normal limits and, in particular, were not early. The majority of the patients in the infantile and juvenile groups were female whereas the adolescent group had a male predominance. There was a similar occurrence of bilateral involvement in all groups (infantile group 64%, juvenile group 53% and adolescent group 61%). There was an increased percentage of individuals who were overweight or obese (according to BMI percentiles) in each of the three groups compared to normative data (infantile 76%, juvenile 86% and adolescent 88%). A greater proportion of male patients were classified as obese compared to female patients (82% versus 50%). There was however no significant difference in the bMi of patients with unilateral or bilateral deformity
CONCLUSION: New findings from this large South African population of children with Blount's disease were an increased occurrence of bilateral involvement in all age groups and no association with early walking - both findings are different from the international literature. Similar to other international studies, female preponderance in the infantile group and male preponderance in the adolescent group was confirmed. Other findings include an increased occurrence of obesity in male children in all groups as well as an increasing occurrence of obesity as the groups progressed from infantile (42%), to juvenile (76%), to adolescent (82%) using the CDC percentiles for age. No risk factors were found for unilateral involvement
Level of evidence: Level 4
Key words: Blount's disease, family history, ethnicity, milestones, sex, body mass index, obesity
Introduction
Blount's disease is a developmental disorder presenting in childhood and results in multiplanar deformities of the lower limb. The deformities develop secondary to relative inhibition of the posteromedial aspect of the proximal tibial growth plate and include tibial varus, procurvatum, internal rotation and limb shortening.1-4
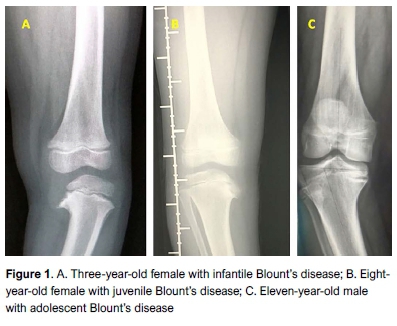
Blount's disease can be classified into two groups depending on the age of onset with the early onset or infantile group, occurring under the age of 4 years, and late-onset, occurring after the age of 4 years.5,6 Late-onset Blount's disease can be further classified into a juvenile group (onset at age 4 to 10 years) and an adolescent group (onset after the age of 10 years). The current paper will use the three groups as described by Thompson and Carter6(Figure 1).
Despite a perceived increased burden of Blount's disease in South Africa, the epidemiology and features of the South African population are largely unknown.
With regard to ethnicity, it has been reported that there is an increased prevalence of all groups in the African American and Hispanic populations compared with European or Asian groups.5,7-9
A genetic component of Blount's disease has been proposed with several reports demonstrating a possible hereditary cause for the disease. A direct pattern of inheritance has not yet been demonstrated.10-12
Early onset walking age has been proposed as an association with infantile Blount's disease and has been hypothesised to produce increased stress on the medial aspect of the proximal tibia in the predisposed infant with bow legs.9 This has been disputed by other work.11,13
Studies regarding sex and Blount's disease also show a mixture of results. The ratio is often affected by the age of the patients in the studies with some showing more female and others more male involvement, depending on age at onset.10,11,13-15
The majority of the international literature shows that bilateral involvement is more common in the infantile group.15,16 In another local study, Bathfield and Beighton found a high incidence of bilateral involvement in the infantile group.13 As the children get older (juvenile and adolescent groups), a recent review showed that unilateral involvement is more common.5
Blount's disease is associated with an increased body mass index (BMI) - defined by the Center for Disease Control and Prevention (CDC) for age as either overweight (BMI between 85th and 95th percentile) or obese (BMI > 95th percentile). A large percentage of patients treated with infantile Blount's disease are obese for age, as reported in a number of studies.5,6,17,18
The aim of this study is to explore the profile of patients with Blount's disease seen at Chris Hani Baragwanath Academic Hospital (CHBAH) in South Africa. Demographic data including family history, ethnicity, attainment of milestones, age when the deformity was first noticed, age at presentation, sex, bilateral involvement and body mass index (BMI) are documented. This study provides further insights into the understanding of this disease, in a South African context.
Patients and methods
This is a hospital-based, retrospective case series with an evaluation of hospital and outpatient records (data sheets) of children diagnosed with Blount's disease (including infantile, juvenile and adolescent groups), over a 14-year period, at CHBAH from 01 January 2003 to 31 December 2016. Demographic information including family history, ethnicity, milestones, age when noticed, age at presentation, sex, bilateral involvement and BMI was documented. All patients diagnosed with Blount's disease were included in the study. Diagnosis in the older patients was based on the typical clinical and radiological features of Blount's disease while the metaphyseal diaphyseal angle (MDA or angle of Drennan) was used to differentiate infantile Blount's disease from physiological bowing (Figure 2). Only patients with an MDA of 16° or higher were included. Patients with genu varum attributable to other causes were excluded. This study was approved by the Human Research Ethics Committee of the University of Witwatersrand (clearance no. M141101).

A total of 108 children with Blount's disease were included in the study. There was some missing data in the fields of family history and milestones. Data regarding family history was available in 60/108 patients. Data regarding milestones was available in 64/108 (sitting), 53/108 (crawling) and 71/108 (walking).
The Center for Disease Control and Prevention (CDC) BMI-for-age growth charts were used to convert the body mass index to a percentile based on a patient's age and sex and compared to normative data.17 The BMI value on its own is not relevant as, with growth, the value will increase normally. A BMI between the 5th percentile and less than the 85th percentile is considered 'normal or healthy weight', that from the 85th percentile to less than the 95th percentile is considered 'overweight', and that equal to or greater than the 95th percentile is 'obese'.17
GraphPad Prism 8 software was used for statistical analyses. Demographic and clinical features were described using medians with a range. Confidence intervals were not used, as the data was not normally distributed. Percentages were reported for categorical variables. Statistical significance was calculated using the Mann-Whitney U-test with a p value <0.05. A Kruskal-Wallis rank-sum test and Dunn's post hoc test was performed to detect differences between more than two groups for independent variables.
Results
Data was available for 108 patients with a total of 172 involved limbs. There were 44 children in the infantile group, 36 children in the juvenile group and 28 children in the adolescent group. Basic demographic data is shown in Table I.
Family history and ethnicity
All patients in the current study were of black African ethnicity.
Data from 60 patients was available regarding a family history of Blount's disease. There were 12/60 (20%) documented cases with a family history of significant bow legs (seven in the infantile group and Ave in the juvenile group) while in the adolescent group there were no patients with a positive family history (Table I).
Milestones
Developmental milestones of patients for all three groups (infantile, juvenile and adolescent) were within normal limits. The mean age for independent walking was 12 months in each group (total of 69 children) (infantile, juvenile and adolescent) (Table I).
Sex
The infantile and juvenile groups had a greater proportion of female patients (82% and 69% respectively) while the adolescent group had a greater proportion of male patients (79%). This difference was statistically significant. (p=0.016) (Table I).
Bilateral involvement
The infantile group had 64% bilateral involvement while the juvenile and adolescent groups had 53% and 61% bilateral involvement respectively in 108 children. The high frequency of bilateral involvement in all groups was not statistically significant (p=0.607) (Table II). In all three groups with unilateral involvement, there was a predominance of left-sided involvement (77%) (Table II).
Obesity
The BMI was calculated in 71 children. Using the CDC growth charts and based on their guidelines, the infantile, juvenile and adolescent groups were 33% (11 patients), 10% (two patients) and 6% (one patient) overweight for age classification, respectively (85th percentile to less than the 95th percentile) (Table III). Those patients classified as obese for age (>95th percentile) were 42% (14 patients) in the infantile group, 76% (16 patients) in the juvenile group, and 82% (14 patients) in the adolescent group. When combining overweight and obese patients for age and comparing them to those patients with a normal BMI (based on CDC normative data) for age, 76%, 86% and 88% of patients had an increased BMI for age in the infantile, juvenile and adolescent groups respectively (Table IV).
Overall, the median BMI was significantly higher in the male patients (33.2 [range 16.8-70.4]) than in the females (22.0 [range 13.4-46.1]) across all ages. Significantly, 82% of male patients were classified as obese while 50% of female patients were classified as obese (p=0.016) (Table III).
There was no significant difference in the median BMI between those patients with bilateral disease (28.1 [range 13.4-64.1]) and those with unilateral disease (23.9 [range 14.0-70.4]). Fifty-two percent with unilateral disease and 67% with bilateral disease were classified as obese (p=0.846) (Table III).
Discussion
Epidemiological data regarding Blount's disease in South Africa is limited. Factors associated with the condition have included ethnicity, early walking age, sex, bilateral involvement and obesity.5 A total of 108 patients with 172 involved limbs were analysed in the current study.
All patients in this study were of black African origin consistent with a previous study by Bathfield and Beighton at the same institution in 1978 during the apartheid era.13 Several studies document an increased prevalence among black populations but the reason for this association has not been elucidated.5,8,14
A review by Bradway et al. found the deformity more common in the West Indies.10
Several authors reported a possible genetic component to the disease without demonstrating a direct pattern of inheritance.10'12,19 Reviews in South Africa by White et al.19did not reveal any positive family history of patients with late onset Blount's disease, while Bathfield and Beighton noted that in 110 children with infantile Blount's disease, ten siblings had bow legs and 16 parents were similarly affected during their own infancy.13 In our study, out of 60 children, there were 12 (20%) documented cases with a family history of bow legs (seven in the infantile group and five in the juvenile group) while in the adolescent group there were no patients with a history of affected family members, thus highlighting a possible genetic component in the infantile and juvenile groups.
Bathfield and Beighton reported no difference with regard to early walking age or obesity in children with Blount's disease compared to unaffected children.13
The current study supports these findings which showed a mean walking age of 12 months for the infantile group which is comparable to that of the general population. In the current study, the gross motor developmental milestones (crawling, sitting, walking) of patients within all three groups of Blount's disease were within normal limits. These findings are corroborated by Inaba et al.11This contrasts with findings of a review by Janoyer et al.9
The literature regarding sex for both early and late-onset Blount's disease are conflicting. With infantile Blount's disease, some studies found boys and girls to be equally affected while other studies showed either a male or female preponderance.10'11,14,19
In the infantile group in the current study we had a high female predominance with a female to male ratio of 4.5:1. This contrasts with Bathfield and Beighton who had an almost equal female to male ratio of 1:1.2 in their series of infantile Blount's patients.13 Inaba et al. found a female preponderance with a female to male ratio of 3:2 in infantile Blount's disease.11 With regard to late-onset Blount's disease, some have reported an increased female to male ratio (White et al. 3:2 and Inaba et al. 1.75:1) but this contrasts with most other studies which showed a male predominance with a female to male ratio of 1:4.11,1419 In the current study the juvenile group had a female preponderance with a 2.3:1 female to male ratio but this was reversed to a male preponderance with a 1:3.7 female to male ratio in the adolescent group. The current study indicates that the sex preference towards female in the juvenile group is similar to that of the infantile group but that this changes as the patients get older and present in the adolescent group.
Several studies document an increased frequency of bilateral involvement in the infantile group while the juvenile and adolescent groups tend to have more unilateral involvement.10,11,13,15,16 Bathfield and Beighton in their series of infantile Blount's patients from South Africa, had 82% of patients with bilateral involvement.13 Inaba et al. had 42% bilateral involvement in the infantile group compared to 19% of patients in the adolescent group.11 The current study failed to affirm these findings with a similar occurrence of bilateral involvement in each group - in the infantile group (64%), juvenile group (53%) and the adolescent group (61%) (Table II). Another study from South Africa by White et al. had 60% of patients with evidence of bilateral involvement in late-onset Blount's disease which is comparable to the current study.19 Sabharwal et al. found similar findings to the current study with 59% of children in the infantile group having bilateral involvement compared to 36% of children in the late-onset group.15 The high occurrence of bilateral involvement in this cohort in every group suggests that Blount's disease is a systemic condition.
Blount's disease is documented in many studies to be associated with an increased frequency of increased BMI.5'8,20,21 A large percentage of patients treated with infantile Blount's disease are greater than the 95th percentile of weight for age (obese) as reported in a number of studies in the USA. Scott et al. had an average BMI percentile of 97.2% in their study on infantile Blount's disease.16 Sabharwal et al. had 88% of infantile Blount's patients and 96% of late-onset Blount's patients classified as overweight.15 Richards et al. had 67% of infantile Blount's patients with a weight greater than the 95th percentile.20 The Heuter-Volkmann principle of asymmetric growth inhibition resulting from increased compressive forces on the medial physis helps to explain the pathogenesis of increasing genu varum in Blount's disease with growth.15,16 The compressive forces on the medial aspect of the proximal tibia is markedly increased in obese children with genu varum.18,21 In the current study, a significant proportion of patients (76%, 86% and 88% in the infantile, juvenile and adolescent groups respectively) had an increased BMI for age (>85th percentile - overweight and obese) (Table IV). Overall a greater proportion of male patients were classified as obese compared to female patients (82% versus 50%) and this was statistically significant (p=0.016). There was no significant difference in the BMI of patients with unilateral and bilateral deformity. This study could not elucidate why some obese children have unilateral involvement and why some children with Blount's disease are not obese, but increased levels of obesity have been found in all age groups of Blount's disease.5
There were several limitations to this study. The retrospective nature of the study led to a number of missing data points for the patients enrolled in the study (undocumented items were treated as missing values). Data for milestone achievements was not available for all children (sitting, n=64; crawling, n=53; and walking, n=69), and a family history was only obtained in 60 children. The CDC normative data was used for comparison with overweight and obesity in the current study; this may be less relevant as the CDC normative data did not come from the same region as the population studied for better comparison.
Conclusion
New findings from this large South African population of children with Blount's disease show an increased occurrence of bilateral involvement in all age groups and no association with early walking - both findings are different from the international literature.
Similar to other international studies, female preponderance in the infantile group and male preponderance in the adolescent group were confirmed.
Other findings include an increased occurrence of obesity in male children in all groups as well as an increasing percentage of obesity as the groups progressed from infantile (42%), to juvenile (76%), to adolescent (82%) using the CDC percentiles for age. No risk factors were found for unilateral involvement.
Ethics statement
This study was approved by the Human Research Ethics Committee of the University of Witwatersrand (clearance no. M141101) and consent was obtained from the CEO of Chris Hani Baragwanath Academic Hospital.
Declaration
The authors declare authorship of this article and that they have followed sound scientific research practice. This research is original and does not transgress plagiarism policies.
Acknowledgement
The authors would like to thank Dr Alison Bentley for her help with the statistics of this paper.
Author contributions
MM contributed to the conceptualisation of the study, collated and analysed the data, and was responsible for the write-up of the manuscript. YR assisted with study design, data collection and preparation of the manuscript. GBF contributed to the conceptualisation of the study, data collection, and assisted with preparation of the manuscript.
ORCID
Mehtar © https://orcid.org/0000-0002-8372-0446 Y Ramguthy @ https://orcid.orq/0000-0003-3956-8050 GB Firth https://orcid.org/0000-0002-1594-2290
References
1. Sabharwal S. Blount disease. J Bone Joint Surg Am. 2009 Jul;91(7):1758-76. [ Links ]
2. Siffert RS, Katz JF. The intra-articular deformity in osteochondrosis deformans tibiae. J Bone Joint Surg Am. 1970 Jun;52(4):800-804. [ Links ]
3. Blount WP. Tibia Vara. J Bone Jt Surg. 1937;19(1). [ Links ]
4. Langenskiold A. Tibia vara; (osteochondrosis deformans tibiae); a survey of 23 cases. Acta Chir Scand. 1952 Mar 26;103(1):1-22. [ Links ]
5. Rivero SM, Zhao C, Sabharwal S. Are patient demographics different for early-onset and late-onset Blount disease? Results based on meta-analysis. J Pediatr Orthop Part B. 2015 Nov;24(6):515-20. [ Links ]
6. Thompson GH, Carter JR. Late-onset tibia vara (Blount's disease). Current concepts. Clin Orthop Relat Res. 1990 Jun;255:24-35. [ Links ]
7. Sabharwal S, Sabharwal S. Treatment of infantile Blount disease: an update. J Pediatr Orthop. 2017 Sep;37 Suppl 2:S26-S31. [ Links ]
8. Burghardt RD, Herzenberg JE, Andre S, Bernius P, Kazim MA. Treatment failures and complications in patients with Blount disease treated with temporary hemiepiphysiodesis: A critical systematic literature review. J Pediatr Orthop Part B. 2018 Nov;27(6):522-29. [ Links ]
9. Janoyer M. Blount disease. Orthop Traumatol Surg Res. 2019 Feb;105(1S):S111-S121. [ Links ]
10. Bradway JK, Klassen R, Peterson H. Blount disease: a review of the English literature. J Pediatr Orthop. 1987;7(C):472-80. [ Links ]
11. Inaba Y, Saito T, Takamura K. Multicenter study of Blount disease in Japan by the Japanese Pediatric Orthopaedic Association. J Orthop Sci. 2014 Jan;19(1):132-10. [ Links ]
12. Sibert JR, Bray PT. Probable dominant inheritance in Blount's disease. Clin Genet. 1977 Jun;11(6):394-96. [ Links ]
13. Bathfield CA, Beighton PH. Blount disease. A review of etiological factors in 110 patients. Clin Orthop Relat Res. 1978 Sep;135:29-33. [ Links ]
14. Birch JG. Blount disease. J Am Acad Orthop Surg. 2013 Jul;21 (7):408-18. [ Links ]
15. Sabharwal S, Zhao C, McClemens E. Correlation of body mass index and radiographic deformities in children with Blount disease. J Bone Joint Surg Am. 2007b;89(6):1275-83. [ Links ]
16. Scott AC, Kelly CH, Sullivan E. Body mass index as a prognostic factor in development of infantile Blount disease. J Pediatr Orthop. 2007 Dec;27(8):921-25. [ Links ]
17. CDC. About Child & Teen BMI. cdc.org. 2015. [ Links ]
18. Dietz WH, Gross WL, Kirkpatrick JA. Blount disease (tibia vara): another skeletal disorder associated with childhood obesity. J Pediatr. 1982 Nov; 101 (5):735-37. [ Links ]
19. White C, Dix-Peek S, van Huyssteen A, Hoffman E. Late-onset Blount's disease. SA Orthop J. 2012;11(2):29-35. [ Links ]
20. Richards BS, Katz DE, Sims JB. Effectiveness of brace treatment in early infantile Blount's disease. J Pediatr Orthop. 1998;18(3):374-80. [ Links ]
21. Gushue DL, Houck J, Lerner AL. Effects of childhood obesity on three-dimensional knee joint biomechanics during walking. J Pediatr Orthop. 2005;25(6):763-68. [ Links ]
 Correspondence:
Correspondence:
Dr M Mehtar
University of the Witwatersrand, Chris Hani Baragwanath Academic Hospital
Department of Orthopaedic Surgery
Johannesburg, South Africa
tel: +27823896594
email: mehtarm@hotmail.com
Received: October 2018
Accepted: April 2019
Published: August 2019
Editor: Prof J du Toit, Stellenbosch University, Cape Town, South Africa
Funding: This study did not require any funding.
Conflict of interest: The authors declare having no conflict of interest with regard to this study.














