Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.17 n.1 Centurion Feb./Mar. 2018
http://dx.doi.org/10.17159/2309-8309/2018/v17n1a9
SPINE
Multilevel paediatric idiopathic intervertebral disc calcification: a case study
Grey JPI; Blake CAII
IMBChB, Orthopaedic registrar, Stellenbosch University, Department of Orthopaedic Surgery, Tygerberg Hospital, Western Cape, South Africa
IIBSc, MBChB, MMed (Ortho) UFS, Consultant, Department of Orthopaedic Surgery, Tygerberg Hospital, Western Cape, South Africa
ABSTRACT
Paediatric idiopathic intervertebral disc calcification (PIIDC) is a rare, mostly self-limiting condition in children that was first described by Baron in 1924. The aetiology is unknown and to date fewer than 400 cases have been described. PIIDC is characterised by calcifications mainly affecting the nucleus pulposus of the intervertebral disc. Most often lesions are located within the lower cervical spine, followed by the thoracic spine. The most common reported symptoms include low grade fever, localised tenderness, torticollis and decreased range of motion of the spine in the affected region. We present a case of multiple level idiopathic intervertebral calcifications in a 12-year-old male.
Level of evidence: Level 5
Key words: multiple paediatric idiopathic intervertebral disc calcifications, torticollis, nucleus pulposus, annulus fibrosis, calcification
Background
Paediatric idiopathic intervertebral disc calcification (PIIDC) is rare with less than 400 cases reported since the first published case in 1924 by Baron et al.1-3
The aetiology is unknown.1 Several hypothesises have been described including minor trauma or a viral infection-induced vasculitis leading to a decreased nutrient supply of the disc.2
Patients commonly present with torticollis with or without fever.
Cervical spine involvement is usually symptomatic whereas lumbar spine lesions are asymptomatic.4,5
PIIDC is characterised by radiographic evidence of single or multiple level oval-shaped calcifications mainly affecting the nucleus pulposus of the intervertebral disc.5,6 The most common region is the lower cervical spine followed by the thoracic spine and very rarely the lumbar spine.2 Within the cervical spine the lesion may herniate anteriorly leading to dysphagia or posterior herniation, leading to nerve root or spinal cord compression.1,5,7-13
The majority of PIIDC cases are self-limiting with the gold standard of treatment being conservative management such as bed rest, analgesics, non-steroidal anti-inflammatories, physiotherapy and cervical orthotics.1,4,6-8,14 The prognosis is excellent, with 95% of cases reporting full symptomatic recovery within six months.1,13,14 Recurrence is rare.1,15
Surgical decompression is indicated in cases with severe radiculopathy or acute worsening neurology.1,11
Case presentation
A 12-year-old male presented to our emergency department with a five-day history of spontaneous onset neck stiffness and low grade fever. No recent trauma was reported, and his past medical history was unremarkable.
On physical examination he did not show signs of photophobia, vomiting nor any focal neurological deficit. The patient had full range of motion of the neck; pain was only exacerbated with forward flexion. No torticollis was noted. Mild central vertebral tenderness at the thoracolumbar junction was present with some vague abdominal discomfort.
Laboratory findings revealed a raised C-reactive protein of 47 mg/L and ESR level of 64 mm/hr. Other results included a normal white cell count, serum calcium and alkaline phosphatase. A lumbar puncture was done and cerebral spinal fluid microscopy and chemistry was within normal limits. Our surgery department was consulted and investigations revealed no intra-abdominal pathology contributing to the pain.
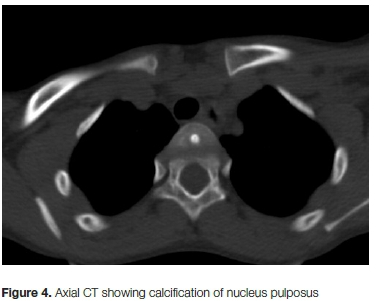
Spinal radiographs revealed multiple level intervertebral disc calcifications (Figures 1 and 2). Computer tomography showed lesions with increased density consistent with calcifications (Figures 3 and 4) at the T1-T4, T10-T12, L1-L2 and S5-coccyx levels. Magnetic resonance imaging was not available at our facility.



The patient was admitted for bed rest, analgesia and non-steroidal anti-inflammatories. He responded within Ave days of admission with complete resolution of neck stiffness and pain.
At his six-week follow-up he had no signs of recurrence and complete symptomatic recovery, with radiographic imaging revealing minimal resolution of the calcifications. At the three-month follow-up visit there were no signs of further radiographic resorption of the calcifications (Figures 5 and 6). Clinically the patient remained asymptomatic.


Discussion
Paediatric idiopathic intervertebral disc calcification is a rare entity. Tsutsumi et al. noted a male predominance with a male to female ratio of 8:5 and the majority of cases being in the 5- to 12-year age group.4
There are several proposed aetiological factors such as trauma, infection, vascular, congenital abnormality and metabolic disease, yet the exact aetiology of paediatric intervertebral disc calcification remains uncertain.1-4,6,13,16
Inflammation is hypothesised to be part of the pathogenesis due to the signs of low grade fever, leukocytosis, raised C-reactive protein, ESR and raised protein in the cerebrospinal fluid.5,17 One theory is viral-induced vasculitis leading to disruption of the nutrient blood supply of the endplate and paediatric disc. This leads to temporary ischaemia followed by cellular necrosis and calcification.18
The combination of pain, fever and raised inflammatory markers may be suggestive of acute discitis. PIIDC differs from discitis in several ways. PIIDC resolves spontaneously without requiring antibiotic treatment. Discitis may have other radiological features including erosion of the adjacent endplates with disc collapse. This does not occur in PIIDC. Intervertebral disc calcification following an episode of discitis is very rare.15
Intervertebral calcifications can affect any region of the spine. Plain radiographs are sufficient to note the presence and extent of intervertebral disc calcification. Computer tomography can define the calcification more clearly and in the presence of neurological deterioration, spinal cord compression and suspected discitis magnetic resonance imaging is recommended.6,14,17
The cervical spine is most commonly affected followed by the thoracic and rarely the lumbar spine.1,2,4 PIIDC usually affects a single intervertebral level with multiple level disc calcification reported in less than 35% of cases.1,6,10,13,14,19 Multiple level disc calcification shows different rates of resorption for each individual lesion.19
PIIDC differs from adult degenerative intervertebral calcification in that it mainly affects the lower cervical and thoracic spine compared to mid-thoracic and upper lumbar spine in adults. The nucleus pulposus is involved in children, and in adults the annulus fibrosis.5,6 In children the calcifications are transient with usually complete resorption.12,14
The most commonly reported symptoms include low grade fever, localised tenderness, torticollis and decreased range of motion of the spine in that affected region.1,5,7,14 Sensorimotor fallout has also been reported. Calcifications involving the cervical spine are much more likely to be symptomatic than lumbar disc calcifications.4,5,20
Anterior or posterior disc herniation has been described in approximately 38% of cases.1 Anterior herniation is often associated with dysphagia, and posterior herniation with radicu-lopathy and neurological deficits in cervical disc calcification.5,7-13
PIIDC is a self-limiting benign entity, and conservative treatment is recommended for the majority of cases. Recurrence is rare.1,15 Conservative measures include bed rest, analgesia, non-steroidal anti-inflammatory medication, physiotherapy and cervical orthotics.1,4,6-8,14 The prognosis is excellent with complete symptom resolution noted in 66% of cases at three weeks and in 95% of cases at six weeks.13,14 Long-term complications include chronic back pain, scoliosis, loss of adjacent vertebral height and anterior osteophyte formation.13,21
Surgical decompression is recommended for cases with progressive neurological deterioration with risk of permanent damage.1,11,13
Conclusion
Multilevel paediatric idiopathic intervertebral disc calcification is a rare entity that requires radiological and biochemical investigations to exclude other more sinister spinal conditions. The identification of PIIDC and the understanding of its natural course is crucial. Management is largely symptomatic and multidisciplinary with predictable resolution of symptoms and resorption of the lesions over time. Only in exceptional cases is surgery considered.
Compliance with ethics guidelines
This article does not contain any studies with human participants or animals performed by any of the authors. For this study, formal consent was not required.
References
1. Chu J, Wang T, Pei S, Yin Z. Surgical treatment for idiopathic intervertebral disc calcification in a child: case report and review of the literature. Childs Nerv Syst. 2015;31(1):123-27. [ Links ]
2. Wang G, Kang Y, Chen F, Wang B. Cervical intervertebral disc calcification combined with ossification of posterior longitudinal ligament in an 11-year-old girl: case report and review of literature. Childs Nerv Syst. 2015;3-8. [ Links ]
3. Liu W, Tang C, Liu L, Zhu QS, Huang LF. Cervical intervertebral disc calcification with extreme lateral herniation in a child: T2-weighted signal intensity of the involved disc can be restored to normal. Child's Nerv Syst. 2016;32(4):749-52. [ Links ]
4. Tsutsumi S, Yasumoto Y, Ito M. Idiopathic intervertebral disk calcification in childhood: A case report and review of literature. Child's Nerv Syst. 2011 ;27(7):1045-51. [ Links ]
5. Sung MP, Kim ES, Duk HS. Cervical radiculopathy caused by neural foraminal migration of a herniated calcified intervertebral disk in childhood: A case report. Arch Phys Med Rehabil. 2005;86(11):2214-17. [ Links ]
6. Lernout C, Haas H, Rubio A, Griffet J. Pediatric intervertebral disk calcification in childhood: Three case reports and review of literature. Child's Nerv Syst. 2009;25(8):1019-23. [ Links ]
7. Fu Z, Shi J, Jia L, Yuan W, Guan Z. Intervertebral thoracic disc calcification associated with ossification of posterior longitudinal ligament in an 11-year-old child. Spine. 2011;36(12):E808-10. [ Links ]
8. Bajard X, Renault F, Benharrats T, Mary P, Madi F, Vialle R. Intervertebral disc calcification with neurological symptoms in children: Report of conservative treatment in two cases. Child's Nerv Syst. 2010;26(7):973-78. [ Links ]
9. Schaser K-D, Stover JF, Kaeaeb MJ, Haas NP, Mittlmeier T. Mild cervical spine trauma showing symptomatic calcified cervical disc herniation in a child: a case report. Spine. 2003;28(5): E93-4. [ Links ]
10. Yang HS, Chen DY, Yuan W, Yang LL, Tsai N, Lin QS. Paresis associated with aconuresis caused by intervertebral disc calcification at c7-t1: a case report and review of the literature. Spine. 2010;35(10):E434-9. [ Links ]
11. Aulisa L, Pitta L, Aulisa AG, Mastantuoni G, Pola E, Leone A. Lumbar nerve root 'walled' by a calcified herniated mass in a young patient. Child's Nerv Syst. 2003;19(5-6):384-86. [ Links ]
12. Mahlfeld K, Kayser R, Grasshoff H. Permanent thoracic myelopathy resulting from herniation of a calcified intervertebral disc in a child. J Pediatr Orthop Part B / Eur Paediatr Orthop Soc Pediatr Orthop Soc North Am. 2002;11:6-9. [ Links ]
13. Donniez H, Mavili E, Ikizceli T, Koç RK. Pediatric intervertebral disc calcification. Diagnostic Interv Radiol. 2008;14(4):225-27. [ Links ]
14. Li M, Rong W, Pan X, Yu L. Single-level calcified cervical disk herniation in a 13-year-old girl. Orthopedics. 2012;35(8): e1297-301. [ Links ]
15. Sasagawa T, Hashimoto F, Nakamura T, Maruhasi Y, Matsumoto N, Segawa T, et al. A pediatric case of single-level idiopathic cervical intervertebral disk calcification with symptom relapse 1 year after initial onset. J Pediatr Orthop. 2014;34(1539-2570 (Electronic)):282-86. [ Links ]
16. Kusabiraki S, Tsubata S. Two karate kids with pediatric idiopathic intervertebral disc calcification. Spine J. Elsevier Inc.; 2014;14(12):3048. [ Links ]
17. Ahemad A, Dasgupta B, Jagiasi J. Intervertebral disc calcification in a child. Indian J Orthop. 2008 Oct-Dec;42(4):480-81. [ Links ]
18. Ho C, Chang S, Fulkerson D, Smith J. Children presenting with calcified disc herniation: a self-limiting process. J Radiol Case Rep [Internet]. 2012;6(10):11-9. [ Links ]
19. Spapens N, Wouters C, Moens P. Thoracolumbar intervertebral disc calcifications in an 8-year-old boy: Case report and review of the literature. Eur J Pediatr. 2010;169(5):577-80. [ Links ]
20. Dhammi IK, Arora A, Monga J. Calcified thoracic intervertebral disc at two levels as a cause of mid-back pain in a child: A case report. J Orthop Sci. 2002;7(5):587-89. [ Links ]
21. Mac-Thiong JM, Leduc S, Marton D, Duhaime M, Morin B. Herniation of a calcified cervical disc into the foramen transversarium in an 8-year-old child. Spine. 2004;29(16): E349-52. [ Links ]
 Correspondence:
Correspondence:
Dr Jan-Petrus Grey
Department of Orthopaedic Surgery, Worcester Provincial Hospital
Western Cape, South Africa
tel: +27 023 348 1100
email: jp11grey@gmail.com
Received: May 2017
Accepted: July 2017
Published: March 2018
Editor: Prof Anton Schepers, University of the Witwatersrand
Funding: No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this article.
Conflict of interest: The authors declare that they have no conflicts of interest.














